User login
Riboflavin helps visualize urine flow during cystoscopy
By increasing urine color, 400 mg of oral riboflavin the night before gynecologic surgery makes it easier to see and confirm urine flow during intraoperative cystoscopy, according to results of a randomized, blinded, placebo-controlled trial.
The traditional go-to for that purpose, intravenous indigo carmine, has been in short supply, if possible to get at all, so surgeons have been looking for other options. Alternatives include intravenous methylene blue, intravenous fluorescein, and oral phenazopyridine, but each have their own problems, including cost, contraindications, and anaphylaxis.
So the study team turned to riboflavin – vitamin B2 – which, in excess, turns the urine bright, sometimes almost neon yellow. It’s “safe, readily available without prescription, and inexpensive ... and should be considered for routine use,” wrote investigators led by Michael L. Stitely, MD, an ob.gyn. at the University of Otago in Dunedin, New Zealand.
The team randomized 33 women to four 100-mg capsules of riboflavin the night before surgery and 33 to four 1,000-IU capsules of vitamin D3, which served as the placebo. Participants, clinicians, researchers, and study staff all were blinded to group allocation, the investigators noted in Obstetrics & Gynecology.
Surgeons rated urine color a median of 2 (slight yellow) in the riboflavin group, compared with 1 (clear) in the placebo arm, on a 3-point scale (P less than .001). About 13 women on riboflavin got a rating of 3 – strong yellow – versus 1 woman in the placebo arm.
The operating surgeons also said it was easier to visualize urine flow in the riboflavin group, giving a median of 5, compared with 4 in the placebo group, on a 5-point scale (P less than .013). They gave a score of 5 to 19 women in the riboflavin group but only to 8 placebo women, meaning that they “strongly agreed” that it was easy to see urine flow; a score of 4 meant that they simply agreed with the statement.
Overall, surgeons confirmed bilateral urine flow in 30 women (91%) in the riboflavin group, compared with 28 women (85%) in the placebo group (P = .71). When a blinded investigator checked the videos, their assessments of the same parameters correlated with those of the surgeons.
No significant differences were found between the groups in age, height, weight, body mass index, or ethnicity. The most common procedure was a midurethral sling (10 in the riboflavin group; 4 in the placebo arm), followed by cystoscopy with botox (4 in the riboflavin group; 7 in the placebo group). None of the women required intervention for urinary tract injury.
Among the limitations cited was the use of subjective and nonvalidated measures of urine color.
The work was funded by the Healthcare Otago Charitable Trust and the Australasian Gynaecological Endoscopy and Surgery Society. The authors reported no conflicts of interest.
SOURCE: Stitely ML et al. Obstet Gynecol. 2019 Jan 8. doi: 10.1097/AOG.0000000000003063.
By increasing urine color, 400 mg of oral riboflavin the night before gynecologic surgery makes it easier to see and confirm urine flow during intraoperative cystoscopy, according to results of a randomized, blinded, placebo-controlled trial.
The traditional go-to for that purpose, intravenous indigo carmine, has been in short supply, if possible to get at all, so surgeons have been looking for other options. Alternatives include intravenous methylene blue, intravenous fluorescein, and oral phenazopyridine, but each have their own problems, including cost, contraindications, and anaphylaxis.
So the study team turned to riboflavin – vitamin B2 – which, in excess, turns the urine bright, sometimes almost neon yellow. It’s “safe, readily available without prescription, and inexpensive ... and should be considered for routine use,” wrote investigators led by Michael L. Stitely, MD, an ob.gyn. at the University of Otago in Dunedin, New Zealand.
The team randomized 33 women to four 100-mg capsules of riboflavin the night before surgery and 33 to four 1,000-IU capsules of vitamin D3, which served as the placebo. Participants, clinicians, researchers, and study staff all were blinded to group allocation, the investigators noted in Obstetrics & Gynecology.
Surgeons rated urine color a median of 2 (slight yellow) in the riboflavin group, compared with 1 (clear) in the placebo arm, on a 3-point scale (P less than .001). About 13 women on riboflavin got a rating of 3 – strong yellow – versus 1 woman in the placebo arm.
The operating surgeons also said it was easier to visualize urine flow in the riboflavin group, giving a median of 5, compared with 4 in the placebo group, on a 5-point scale (P less than .013). They gave a score of 5 to 19 women in the riboflavin group but only to 8 placebo women, meaning that they “strongly agreed” that it was easy to see urine flow; a score of 4 meant that they simply agreed with the statement.
Overall, surgeons confirmed bilateral urine flow in 30 women (91%) in the riboflavin group, compared with 28 women (85%) in the placebo group (P = .71). When a blinded investigator checked the videos, their assessments of the same parameters correlated with those of the surgeons.
No significant differences were found between the groups in age, height, weight, body mass index, or ethnicity. The most common procedure was a midurethral sling (10 in the riboflavin group; 4 in the placebo arm), followed by cystoscopy with botox (4 in the riboflavin group; 7 in the placebo group). None of the women required intervention for urinary tract injury.
Among the limitations cited was the use of subjective and nonvalidated measures of urine color.
The work was funded by the Healthcare Otago Charitable Trust and the Australasian Gynaecological Endoscopy and Surgery Society. The authors reported no conflicts of interest.
SOURCE: Stitely ML et al. Obstet Gynecol. 2019 Jan 8. doi: 10.1097/AOG.0000000000003063.
By increasing urine color, 400 mg of oral riboflavin the night before gynecologic surgery makes it easier to see and confirm urine flow during intraoperative cystoscopy, according to results of a randomized, blinded, placebo-controlled trial.
The traditional go-to for that purpose, intravenous indigo carmine, has been in short supply, if possible to get at all, so surgeons have been looking for other options. Alternatives include intravenous methylene blue, intravenous fluorescein, and oral phenazopyridine, but each have their own problems, including cost, contraindications, and anaphylaxis.
So the study team turned to riboflavin – vitamin B2 – which, in excess, turns the urine bright, sometimes almost neon yellow. It’s “safe, readily available without prescription, and inexpensive ... and should be considered for routine use,” wrote investigators led by Michael L. Stitely, MD, an ob.gyn. at the University of Otago in Dunedin, New Zealand.
The team randomized 33 women to four 100-mg capsules of riboflavin the night before surgery and 33 to four 1,000-IU capsules of vitamin D3, which served as the placebo. Participants, clinicians, researchers, and study staff all were blinded to group allocation, the investigators noted in Obstetrics & Gynecology.
Surgeons rated urine color a median of 2 (slight yellow) in the riboflavin group, compared with 1 (clear) in the placebo arm, on a 3-point scale (P less than .001). About 13 women on riboflavin got a rating of 3 – strong yellow – versus 1 woman in the placebo arm.
The operating surgeons also said it was easier to visualize urine flow in the riboflavin group, giving a median of 5, compared with 4 in the placebo group, on a 5-point scale (P less than .013). They gave a score of 5 to 19 women in the riboflavin group but only to 8 placebo women, meaning that they “strongly agreed” that it was easy to see urine flow; a score of 4 meant that they simply agreed with the statement.
Overall, surgeons confirmed bilateral urine flow in 30 women (91%) in the riboflavin group, compared with 28 women (85%) in the placebo group (P = .71). When a blinded investigator checked the videos, their assessments of the same parameters correlated with those of the surgeons.
No significant differences were found between the groups in age, height, weight, body mass index, or ethnicity. The most common procedure was a midurethral sling (10 in the riboflavin group; 4 in the placebo arm), followed by cystoscopy with botox (4 in the riboflavin group; 7 in the placebo group). None of the women required intervention for urinary tract injury.
Among the limitations cited was the use of subjective and nonvalidated measures of urine color.
The work was funded by the Healthcare Otago Charitable Trust and the Australasian Gynaecological Endoscopy and Surgery Society. The authors reported no conflicts of interest.
SOURCE: Stitely ML et al. Obstet Gynecol. 2019 Jan 8. doi: 10.1097/AOG.0000000000003063.
FROM OBSTETRICS & GYNECOLOGY
Key clinical point: Oral riboflavin the night before gynecologic surgery is a sound alternative to indigo carmine for cystoscopy visualization.
Major finding: Surgeons rated urine color a median of 2 (slight yellow) in the riboflavin group, compared with 1 (clear) in the placebo arm on a 3-point scale (P less than .001). About 13 women on riboflavin got a rating of 3 – strong yellow – versus 1 woman in the placebo arm.
Study details: A randomized trial with 66 women.
Disclosures: The work was funded by the Healthcare Otago Charitable Trust and the Australasian Gynaecological Endoscopy and Surgery Society. The authors reported no conflicts of interest.
Source: Stitely ML et al. Obstet Gynecol. 2019 Jan 8. doi: 10.1097/AOG.0000000000003063.
SGLT2s for heart failure first, diabetes second
Also today, influenza activity hits a seasonal high, the U.S. Supreme Court halts a Louisiana abortion law from taking effect, and cilostazol plus aspirin or clopidogrel reduces the risk of recurrent stroke.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, influenza activity hits a seasonal high, the U.S. Supreme Court halts a Louisiana abortion law from taking effect, and cilostazol plus aspirin or clopidogrel reduces the risk of recurrent stroke.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Also today, influenza activity hits a seasonal high, the U.S. Supreme Court halts a Louisiana abortion law from taking effect, and cilostazol plus aspirin or clopidogrel reduces the risk of recurrent stroke.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
The Underrecognized Risk for Drug Overdose Deaths
The numbers are stunning: 1,643% increase in rates of deaths involving synthetic opioids. A 915% increase for heroin, 830% for benzodiazepines. Even more stunning: Those are the increases only in overdose death rates for women aged 30 to 64 years.
According to CDC data, between 1999 and 2010, the largest percentage change in the rates of overall drug overdose deaths was among women aged between 45 and 64 years. But that research did not account for trends in specific drugs or consider changes in age group distributions, say researchers from the CDC’s National Center for Injury Prevention and Control.
They examined overdose death rates among women aged 30 to 64 years between 1999 and 2017. The unadjusted death rate jumped 260%, from 4,314 deaths to 18,110 deaths. Among women aged 55 to 59 years, the number of deaths involving antidepressants increased approximately 300%; among women aged 60 to 64 years, nearly 400%. The crude rate of deaths involving prescription opioids skyrocketed > 1,000%.
The drug epidemic is “evolving,” the researchers note. In 1999, overdose death rates were highest among women aged 40 to 44 years. In 2017, they were highest among women aged 50 to 54 years. And as demographics shift, prevention programs need to shift as well. As women age, the researchers say, individual experiences can change the type of substance used or misused and in the experiences of pain that might result in an opioid prescription.
The researchers note that “substantial work” has focused on informing women of childbearing age about the risks and benefits of certain drugs. The current analysis demonstrates “the remaining need” to consider middle-aged women who are at risk.
Targeted efforts are needed, and the researchers suggest interventions: Medicaid and other health insurance programs can review records of controlled substance prescribing. States and local communities can expand capacity of drug use disorder treatments and links to care, particularly adding “gender-responsive” substance use disorder treatment centers.
A “multifaceted approach involving the full spectrum of care services is likely necessary,” the researchers say. Health care practitioners who treat women for pain, depression, or anxiety can discuss treatment options that consider the unique biopsychosocial needs of women.
Health care practitioners also can consider implementing the CDC Guideline for Prescribing Opioids for Chronic Pain, which says “Opioids are not first-line or routine therapy for chronic pain.” The guideline also says before starting and periodically during opioid therapy, clinicians should discuss with patients the “known risks and realistic benefits of opioid therapy.” In other words, listen to the women and prescribe carefully.
The numbers are stunning: 1,643% increase in rates of deaths involving synthetic opioids. A 915% increase for heroin, 830% for benzodiazepines. Even more stunning: Those are the increases only in overdose death rates for women aged 30 to 64 years.
According to CDC data, between 1999 and 2010, the largest percentage change in the rates of overall drug overdose deaths was among women aged between 45 and 64 years. But that research did not account for trends in specific drugs or consider changes in age group distributions, say researchers from the CDC’s National Center for Injury Prevention and Control.
They examined overdose death rates among women aged 30 to 64 years between 1999 and 2017. The unadjusted death rate jumped 260%, from 4,314 deaths to 18,110 deaths. Among women aged 55 to 59 years, the number of deaths involving antidepressants increased approximately 300%; among women aged 60 to 64 years, nearly 400%. The crude rate of deaths involving prescription opioids skyrocketed > 1,000%.
The drug epidemic is “evolving,” the researchers note. In 1999, overdose death rates were highest among women aged 40 to 44 years. In 2017, they were highest among women aged 50 to 54 years. And as demographics shift, prevention programs need to shift as well. As women age, the researchers say, individual experiences can change the type of substance used or misused and in the experiences of pain that might result in an opioid prescription.
The researchers note that “substantial work” has focused on informing women of childbearing age about the risks and benefits of certain drugs. The current analysis demonstrates “the remaining need” to consider middle-aged women who are at risk.
Targeted efforts are needed, and the researchers suggest interventions: Medicaid and other health insurance programs can review records of controlled substance prescribing. States and local communities can expand capacity of drug use disorder treatments and links to care, particularly adding “gender-responsive” substance use disorder treatment centers.
A “multifaceted approach involving the full spectrum of care services is likely necessary,” the researchers say. Health care practitioners who treat women for pain, depression, or anxiety can discuss treatment options that consider the unique biopsychosocial needs of women.
Health care practitioners also can consider implementing the CDC Guideline for Prescribing Opioids for Chronic Pain, which says “Opioids are not first-line or routine therapy for chronic pain.” The guideline also says before starting and periodically during opioid therapy, clinicians should discuss with patients the “known risks and realistic benefits of opioid therapy.” In other words, listen to the women and prescribe carefully.
The numbers are stunning: 1,643% increase in rates of deaths involving synthetic opioids. A 915% increase for heroin, 830% for benzodiazepines. Even more stunning: Those are the increases only in overdose death rates for women aged 30 to 64 years.
According to CDC data, between 1999 and 2010, the largest percentage change in the rates of overall drug overdose deaths was among women aged between 45 and 64 years. But that research did not account for trends in specific drugs or consider changes in age group distributions, say researchers from the CDC’s National Center for Injury Prevention and Control.
They examined overdose death rates among women aged 30 to 64 years between 1999 and 2017. The unadjusted death rate jumped 260%, from 4,314 deaths to 18,110 deaths. Among women aged 55 to 59 years, the number of deaths involving antidepressants increased approximately 300%; among women aged 60 to 64 years, nearly 400%. The crude rate of deaths involving prescription opioids skyrocketed > 1,000%.
The drug epidemic is “evolving,” the researchers note. In 1999, overdose death rates were highest among women aged 40 to 44 years. In 2017, they were highest among women aged 50 to 54 years. And as demographics shift, prevention programs need to shift as well. As women age, the researchers say, individual experiences can change the type of substance used or misused and in the experiences of pain that might result in an opioid prescription.
The researchers note that “substantial work” has focused on informing women of childbearing age about the risks and benefits of certain drugs. The current analysis demonstrates “the remaining need” to consider middle-aged women who are at risk.
Targeted efforts are needed, and the researchers suggest interventions: Medicaid and other health insurance programs can review records of controlled substance prescribing. States and local communities can expand capacity of drug use disorder treatments and links to care, particularly adding “gender-responsive” substance use disorder treatment centers.
A “multifaceted approach involving the full spectrum of care services is likely necessary,” the researchers say. Health care practitioners who treat women for pain, depression, or anxiety can discuss treatment options that consider the unique biopsychosocial needs of women.
Health care practitioners also can consider implementing the CDC Guideline for Prescribing Opioids for Chronic Pain, which says “Opioids are not first-line or routine therapy for chronic pain.” The guideline also says before starting and periodically during opioid therapy, clinicians should discuss with patients the “known risks and realistic benefits of opioid therapy.” In other words, listen to the women and prescribe carefully.
High prevalence of sleep problems in children with autism spectrum disorder
Children with a diagnosis of autism spectrum disorder or another developmental delay or disorder that includes autistic characteristics are twice as likely to have sleeping problems, a multisite case-control study has found.
The findings match up with previous similar studies, but this study is among the largest to measure sleeping problems in children with autism spectrum disorder (ASD) with two control groups.
“ including physiologic differences, sleep disorders, developmental comorbidities, medical comorbidities causing sleep disruption, communication impairments, and behavioral disturbances,” Ann M. Reynolds, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and her associates reported in Pediatrics.
“Children with ASD are more likely to have anxiety, which may predispose them to sleep problems,” the authors added.
The study evaluated sleep habits and problems in 1,987 children aged 2-5 years. The study population included 522 children with ASD, 228 children with other developmental delays and disorders that have ASD characteristics, 534 children with other developmental delays and disorders, and 703 children from the general population.
Parents completed the Children Sleep Habits Questionnaire (CSHQ), a 33-item assessment tool typically used with a total score cutoff of 41 and above for identification of children with sleep disorders. The researchers also used a second, more conservative cutoff of 48 – the cutoff for the highest quartile in the general population group – to avoid overidentification with the lower cutoff.
Scores were adjusted for maternal education and race/ethnicity, family income, child age and sex, and child cognitive scores on the Mullen Scales of Early Learning (MSEL). The researchers also adjusted for genetic and/or neurologic diagnoses, including Down syndrome, fragile X, Rett syndrome, tuberous sclerosis, cerebral palsy, and neurofibromatosis.
Autistic children tended to have lower MSEL scores than the other children. Both the autistic children and those with other developmental disorders and delays were more likely than those in the general population to have neurologic or genetic conditions.
Based on a cutoff score of 48, autistic children had more than double the odds of sleep problems, compared with children in the general population (adjusted odds ratio, 2.37; P = .001) and children with other developmental delays (aOR, 2.12; P = .001).
With a cutoff of 41, ASD children’s odds of sleep problems were 1.45 times greater than the general population (P = .023) and 1.75 times greater than those with developmental delays (P = .001).
But children with developmental delays who displayed autistic characteristics did not have not significantly different prevalence of sleep problems than children with ASD had.
“The phenotypic overlay between children with ASD and children with developmental delay with ASD [characteristics] may explain the similarities in sleep disturbance among these two groups,” the authors wrote. Both groups have “higher rates of obsessive-compulsive symptoms, self-injurious behavior, ADHD symptoms, and developmental and communication impairments” than children with developmental delays without autistic characteristics.
The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
SOURCE: Reynolds AM et al. Pediatrics. 2019 Feb. 11. doi: 10.1542/peds.2018-0492.
We can help reduce night waking and improve sleep onset within 5-15 weeks after parents have been trained. “Successful behavioral programs include bedtime fading, teaching healthy sleep practices, and increasing a child’s physical activity during the day,” Catherine Lord, PhD, wrote. Although research supports melatonin as an effective intervention for helping children fall asleep and sleep longer, the high percentage of children in the study already taking melatonin reveals its limitations. “Thus, it is recommended that families try behavioral programs before trials with melatonin,” she wrote.
But families and providers can only work together to address sleep issues if providers ask about sleep concerns, help families implement interventions, and follow up with progress. “In most cases, this help does not have to come from sleep experts, but does require dedicated time and effort using the now-growing base of evidence about effective interventions,” she concluded.
These comments are condensed from an editorial (Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-2629) by Dr. Lord , a professor of psychiatry and biobehavioral sciences at the University of California Los Angeles. Dr. Lord reports royalties from diagnostic instruments used in this study that were donated to a not-for-profit agency. She is supported by grants from the National Institutes of Health and Simons Foundation Autism Research Initiative.
We can help reduce night waking and improve sleep onset within 5-15 weeks after parents have been trained. “Successful behavioral programs include bedtime fading, teaching healthy sleep practices, and increasing a child’s physical activity during the day,” Catherine Lord, PhD, wrote. Although research supports melatonin as an effective intervention for helping children fall asleep and sleep longer, the high percentage of children in the study already taking melatonin reveals its limitations. “Thus, it is recommended that families try behavioral programs before trials with melatonin,” she wrote.
But families and providers can only work together to address sleep issues if providers ask about sleep concerns, help families implement interventions, and follow up with progress. “In most cases, this help does not have to come from sleep experts, but does require dedicated time and effort using the now-growing base of evidence about effective interventions,” she concluded.
These comments are condensed from an editorial (Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-2629) by Dr. Lord , a professor of psychiatry and biobehavioral sciences at the University of California Los Angeles. Dr. Lord reports royalties from diagnostic instruments used in this study that were donated to a not-for-profit agency. She is supported by grants from the National Institutes of Health and Simons Foundation Autism Research Initiative.
We can help reduce night waking and improve sleep onset within 5-15 weeks after parents have been trained. “Successful behavioral programs include bedtime fading, teaching healthy sleep practices, and increasing a child’s physical activity during the day,” Catherine Lord, PhD, wrote. Although research supports melatonin as an effective intervention for helping children fall asleep and sleep longer, the high percentage of children in the study already taking melatonin reveals its limitations. “Thus, it is recommended that families try behavioral programs before trials with melatonin,” she wrote.
But families and providers can only work together to address sleep issues if providers ask about sleep concerns, help families implement interventions, and follow up with progress. “In most cases, this help does not have to come from sleep experts, but does require dedicated time and effort using the now-growing base of evidence about effective interventions,” she concluded.
These comments are condensed from an editorial (Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-2629) by Dr. Lord , a professor of psychiatry and biobehavioral sciences at the University of California Los Angeles. Dr. Lord reports royalties from diagnostic instruments used in this study that were donated to a not-for-profit agency. She is supported by grants from the National Institutes of Health and Simons Foundation Autism Research Initiative.
Children with a diagnosis of autism spectrum disorder or another developmental delay or disorder that includes autistic characteristics are twice as likely to have sleeping problems, a multisite case-control study has found.
The findings match up with previous similar studies, but this study is among the largest to measure sleeping problems in children with autism spectrum disorder (ASD) with two control groups.
“ including physiologic differences, sleep disorders, developmental comorbidities, medical comorbidities causing sleep disruption, communication impairments, and behavioral disturbances,” Ann M. Reynolds, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and her associates reported in Pediatrics.
“Children with ASD are more likely to have anxiety, which may predispose them to sleep problems,” the authors added.
The study evaluated sleep habits and problems in 1,987 children aged 2-5 years. The study population included 522 children with ASD, 228 children with other developmental delays and disorders that have ASD characteristics, 534 children with other developmental delays and disorders, and 703 children from the general population.
Parents completed the Children Sleep Habits Questionnaire (CSHQ), a 33-item assessment tool typically used with a total score cutoff of 41 and above for identification of children with sleep disorders. The researchers also used a second, more conservative cutoff of 48 – the cutoff for the highest quartile in the general population group – to avoid overidentification with the lower cutoff.
Scores were adjusted for maternal education and race/ethnicity, family income, child age and sex, and child cognitive scores on the Mullen Scales of Early Learning (MSEL). The researchers also adjusted for genetic and/or neurologic diagnoses, including Down syndrome, fragile X, Rett syndrome, tuberous sclerosis, cerebral palsy, and neurofibromatosis.
Autistic children tended to have lower MSEL scores than the other children. Both the autistic children and those with other developmental disorders and delays were more likely than those in the general population to have neurologic or genetic conditions.
Based on a cutoff score of 48, autistic children had more than double the odds of sleep problems, compared with children in the general population (adjusted odds ratio, 2.37; P = .001) and children with other developmental delays (aOR, 2.12; P = .001).
With a cutoff of 41, ASD children’s odds of sleep problems were 1.45 times greater than the general population (P = .023) and 1.75 times greater than those with developmental delays (P = .001).
But children with developmental delays who displayed autistic characteristics did not have not significantly different prevalence of sleep problems than children with ASD had.
“The phenotypic overlay between children with ASD and children with developmental delay with ASD [characteristics] may explain the similarities in sleep disturbance among these two groups,” the authors wrote. Both groups have “higher rates of obsessive-compulsive symptoms, self-injurious behavior, ADHD symptoms, and developmental and communication impairments” than children with developmental delays without autistic characteristics.
The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
SOURCE: Reynolds AM et al. Pediatrics. 2019 Feb. 11. doi: 10.1542/peds.2018-0492.
Children with a diagnosis of autism spectrum disorder or another developmental delay or disorder that includes autistic characteristics are twice as likely to have sleeping problems, a multisite case-control study has found.
The findings match up with previous similar studies, but this study is among the largest to measure sleeping problems in children with autism spectrum disorder (ASD) with two control groups.
“ including physiologic differences, sleep disorders, developmental comorbidities, medical comorbidities causing sleep disruption, communication impairments, and behavioral disturbances,” Ann M. Reynolds, MD, of the University of Colorado and Children’s Hospital Colorado, both in Aurora, and her associates reported in Pediatrics.
“Children with ASD are more likely to have anxiety, which may predispose them to sleep problems,” the authors added.
The study evaluated sleep habits and problems in 1,987 children aged 2-5 years. The study population included 522 children with ASD, 228 children with other developmental delays and disorders that have ASD characteristics, 534 children with other developmental delays and disorders, and 703 children from the general population.
Parents completed the Children Sleep Habits Questionnaire (CSHQ), a 33-item assessment tool typically used with a total score cutoff of 41 and above for identification of children with sleep disorders. The researchers also used a second, more conservative cutoff of 48 – the cutoff for the highest quartile in the general population group – to avoid overidentification with the lower cutoff.
Scores were adjusted for maternal education and race/ethnicity, family income, child age and sex, and child cognitive scores on the Mullen Scales of Early Learning (MSEL). The researchers also adjusted for genetic and/or neurologic diagnoses, including Down syndrome, fragile X, Rett syndrome, tuberous sclerosis, cerebral palsy, and neurofibromatosis.
Autistic children tended to have lower MSEL scores than the other children. Both the autistic children and those with other developmental disorders and delays were more likely than those in the general population to have neurologic or genetic conditions.
Based on a cutoff score of 48, autistic children had more than double the odds of sleep problems, compared with children in the general population (adjusted odds ratio, 2.37; P = .001) and children with other developmental delays (aOR, 2.12; P = .001).
With a cutoff of 41, ASD children’s odds of sleep problems were 1.45 times greater than the general population (P = .023) and 1.75 times greater than those with developmental delays (P = .001).
But children with developmental delays who displayed autistic characteristics did not have not significantly different prevalence of sleep problems than children with ASD had.
“The phenotypic overlay between children with ASD and children with developmental delay with ASD [characteristics] may explain the similarities in sleep disturbance among these two groups,” the authors wrote. Both groups have “higher rates of obsessive-compulsive symptoms, self-injurious behavior, ADHD symptoms, and developmental and communication impairments” than children with developmental delays without autistic characteristics.
The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
SOURCE: Reynolds AM et al. Pediatrics. 2019 Feb. 11. doi: 10.1542/peds.2018-0492.
FROM PEDIATRICS
Key clinical point: Sleeping problems are over twice as common in autistic children than in children in the general population.
Major finding: Children with ASD had 2.37 greater odds of sleep problems than did typically developing children.
Study details: Data from the Children Sleep Habits Questionnaire for 1,987 children, either typically developing, diagnosed with autism spectrum disorder, or diagnosed with other developmental disabilities.
Disclosures: The research was funded by the Centers for Disease Control and Prevention, the National Institutes of Health, and the National Center for Advancing Translational Sciences Colorado Clinical and Translational Science Award. Dr. Reynolds consults for Ovid Therapeutics regarding evaluation of sleep severity and improvement in clinical trials. No other authors had disclosures.
Source: Reynolds AM et al. Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2018-0492.
LGBTQ youth struggle in foster or unstable housing situations
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth living in foster care or unstable housing are at greater risk for mental health problems, victimization, and getting into fights at school, compared with LGBTQ youth in stable housing and heterosexual youth in foster care, reported Laura Baums, PhD, of the University of Texas at Austin and her coauthors.
This was the finding of analyses of nested data of more than 493,000 students aged 10-18 years from the cross-sectional California Healthy Kids Survey for 2013-2015; 13% identified as LGBTQ. The analyses published in Pediatrics showed LGBTQ youth also were overrepresented in those living situations as compared with the general population.
Less than 1% of the overall sample was in foster care, but 30% of those youth identified as LGBTQ. About 4% of the overall sample lived in unstable housing, and 25% of those youth identified as LGBTQ. So the proportion of LGBTQ youth in foster care or unstable housing was two to three times greater than would be expected than the estimates of LGBTQ youth in nationally representative adolescent samples (that is 11%), Dr. Baums and her associates said.
LGBTQ youth in unstable housing reported lower grades, higher substance/alcohol abuse, higher rates of absenteeism, more fights in school, and more victimization, compared with heterosexual youth in unstable housing and LGBTQ youth in stable housing. Both LGBTQ youth in unstable housing and those in foster care reported higher rates of depression and suicidality in the past year, but the rates for depression were not different from LGBTQ youth in stable housing. Furthermore, African American LGBTQ youth in unstable housing showed poorer outcomes than non-Hispanic white LGBTQ youth in unstable housing, they said.
“” concluded Dr. Baums and her associates. “The findings of this study point to the need for care that is affirming and respectful of youth’s sexual orientation and gender identity.”
The authors reported no relevant financial disclosures. The study was funded by a Eunice Kennedy Shriver National Institute of Child Health and Human Development grant and supported by the Communities for Just Schools Fund and the Priscilla Pond Flawn Endowment at the university.
SOURCE: Baum L et al. Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2017-4211.
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth living in foster care or unstable housing are at greater risk for mental health problems, victimization, and getting into fights at school, compared with LGBTQ youth in stable housing and heterosexual youth in foster care, reported Laura Baums, PhD, of the University of Texas at Austin and her coauthors.
This was the finding of analyses of nested data of more than 493,000 students aged 10-18 years from the cross-sectional California Healthy Kids Survey for 2013-2015; 13% identified as LGBTQ. The analyses published in Pediatrics showed LGBTQ youth also were overrepresented in those living situations as compared with the general population.
Less than 1% of the overall sample was in foster care, but 30% of those youth identified as LGBTQ. About 4% of the overall sample lived in unstable housing, and 25% of those youth identified as LGBTQ. So the proportion of LGBTQ youth in foster care or unstable housing was two to three times greater than would be expected than the estimates of LGBTQ youth in nationally representative adolescent samples (that is 11%), Dr. Baums and her associates said.
LGBTQ youth in unstable housing reported lower grades, higher substance/alcohol abuse, higher rates of absenteeism, more fights in school, and more victimization, compared with heterosexual youth in unstable housing and LGBTQ youth in stable housing. Both LGBTQ youth in unstable housing and those in foster care reported higher rates of depression and suicidality in the past year, but the rates for depression were not different from LGBTQ youth in stable housing. Furthermore, African American LGBTQ youth in unstable housing showed poorer outcomes than non-Hispanic white LGBTQ youth in unstable housing, they said.
“” concluded Dr. Baums and her associates. “The findings of this study point to the need for care that is affirming and respectful of youth’s sexual orientation and gender identity.”
The authors reported no relevant financial disclosures. The study was funded by a Eunice Kennedy Shriver National Institute of Child Health and Human Development grant and supported by the Communities for Just Schools Fund and the Priscilla Pond Flawn Endowment at the university.
SOURCE: Baum L et al. Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2017-4211.
Lesbian, gay, bisexual, transgender, and questioning (LGBTQ) youth living in foster care or unstable housing are at greater risk for mental health problems, victimization, and getting into fights at school, compared with LGBTQ youth in stable housing and heterosexual youth in foster care, reported Laura Baums, PhD, of the University of Texas at Austin and her coauthors.
This was the finding of analyses of nested data of more than 493,000 students aged 10-18 years from the cross-sectional California Healthy Kids Survey for 2013-2015; 13% identified as LGBTQ. The analyses published in Pediatrics showed LGBTQ youth also were overrepresented in those living situations as compared with the general population.
Less than 1% of the overall sample was in foster care, but 30% of those youth identified as LGBTQ. About 4% of the overall sample lived in unstable housing, and 25% of those youth identified as LGBTQ. So the proportion of LGBTQ youth in foster care or unstable housing was two to three times greater than would be expected than the estimates of LGBTQ youth in nationally representative adolescent samples (that is 11%), Dr. Baums and her associates said.
LGBTQ youth in unstable housing reported lower grades, higher substance/alcohol abuse, higher rates of absenteeism, more fights in school, and more victimization, compared with heterosexual youth in unstable housing and LGBTQ youth in stable housing. Both LGBTQ youth in unstable housing and those in foster care reported higher rates of depression and suicidality in the past year, but the rates for depression were not different from LGBTQ youth in stable housing. Furthermore, African American LGBTQ youth in unstable housing showed poorer outcomes than non-Hispanic white LGBTQ youth in unstable housing, they said.
“” concluded Dr. Baums and her associates. “The findings of this study point to the need for care that is affirming and respectful of youth’s sexual orientation and gender identity.”
The authors reported no relevant financial disclosures. The study was funded by a Eunice Kennedy Shriver National Institute of Child Health and Human Development grant and supported by the Communities for Just Schools Fund and the Priscilla Pond Flawn Endowment at the university.
SOURCE: Baum L et al. Pediatrics. 2019 Feb 11. doi: 10.1542/peds.2017-4211.
FROM PEDIATRICS
Meet the CHEST President-Designate
Steven Q. Simpson, MD, FCCP, is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement. Dr. Simpson acts as a CHEST Regent-at-Large of the Board of Regents, board liaison for the Guidelines Oversight Committee, sits on numerous board task forces and subcommittees and is a member of the CHEST SEEK Critical Care Medicine Editorial Board. He will serve as CHEST President for the 2020-2021 term.
Dr. Simpson is Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the University of Kansas. He is also senior advisor to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the US Department of Health and Human Services. He has conducted research in all areas of severe sepsis, including molecular and cellular mechanisms, translational, quality improvement, and computer modeling studies. He was a founder in 2005 of the Midwest Critical Care Collaborative, a multidisciplinary and interprofessional collaborative effort to improve the quality of critical care services throughout the Midwest. In 2007, he initiated the Kansas Sepsis Project, a statewide program to improve severe sepsis care and outcomes via continuing education both in sepsis and in quality improvement principles and via interprofessional collaborations. Dr. Simpson is an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. He is a member of the board of directors and Chief Medical Officer of Sepsis Alliance, a nationwide patient information and advocacy organization.
During his tenure at the University of New Mexico, he contributed to the discovery of a particular form of sepsis, the hantavirus pulmonary syndrome, and published numerous papers on the clinical description, the hemodynamic description, and the approach to supportive care for patients with the syndrome, including extracorporeal hemodynamic and oxygenation support. Dr. Simpson has authored over 180 scientific articles, book chapters, editorials, abstracts and electronic media publications. He was awarded the 2009 Eli Lilly Distinguished Scholar in Critical Care Medicine Award of the American College of Chest Physicians and the 2013 Roger C. Bone Memorial Lecture in Critical Care Medicine, which recognizes career contributions to the field. He has also been recognized as a Distinguished CHEST Educator in 2017 and 2018.
Steven Q. Simpson, MD, FCCP, is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement. Dr. Simpson acts as a CHEST Regent-at-Large of the Board of Regents, board liaison for the Guidelines Oversight Committee, sits on numerous board task forces and subcommittees and is a member of the CHEST SEEK Critical Care Medicine Editorial Board. He will serve as CHEST President for the 2020-2021 term.
Dr. Simpson is Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the University of Kansas. He is also senior advisor to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the US Department of Health and Human Services. He has conducted research in all areas of severe sepsis, including molecular and cellular mechanisms, translational, quality improvement, and computer modeling studies. He was a founder in 2005 of the Midwest Critical Care Collaborative, a multidisciplinary and interprofessional collaborative effort to improve the quality of critical care services throughout the Midwest. In 2007, he initiated the Kansas Sepsis Project, a statewide program to improve severe sepsis care and outcomes via continuing education both in sepsis and in quality improvement principles and via interprofessional collaborations. Dr. Simpson is an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. He is a member of the board of directors and Chief Medical Officer of Sepsis Alliance, a nationwide patient information and advocacy organization.
During his tenure at the University of New Mexico, he contributed to the discovery of a particular form of sepsis, the hantavirus pulmonary syndrome, and published numerous papers on the clinical description, the hemodynamic description, and the approach to supportive care for patients with the syndrome, including extracorporeal hemodynamic and oxygenation support. Dr. Simpson has authored over 180 scientific articles, book chapters, editorials, abstracts and electronic media publications. He was awarded the 2009 Eli Lilly Distinguished Scholar in Critical Care Medicine Award of the American College of Chest Physicians and the 2013 Roger C. Bone Memorial Lecture in Critical Care Medicine, which recognizes career contributions to the field. He has also been recognized as a Distinguished CHEST Educator in 2017 and 2018.
Steven Q. Simpson, MD, FCCP, is a pulmonologist and intensivist with an extensive background in sepsis and in critical care quality improvement. Dr. Simpson acts as a CHEST Regent-at-Large of the Board of Regents, board liaison for the Guidelines Oversight Committee, sits on numerous board task forces and subcommittees and is a member of the CHEST SEEK Critical Care Medicine Editorial Board. He will serve as CHEST President for the 2020-2021 term.
Dr. Simpson is Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the University of Kansas. He is also senior advisor to the Solving Sepsis initiative of the Biomedical Advanced Research and Development Authority (BARDA) of the US Department of Health and Human Services. He has conducted research in all areas of severe sepsis, including molecular and cellular mechanisms, translational, quality improvement, and computer modeling studies. He was a founder in 2005 of the Midwest Critical Care Collaborative, a multidisciplinary and interprofessional collaborative effort to improve the quality of critical care services throughout the Midwest. In 2007, he initiated the Kansas Sepsis Project, a statewide program to improve severe sepsis care and outcomes via continuing education both in sepsis and in quality improvement principles and via interprofessional collaborations. Dr. Simpson is an author of the 2016 and 2020 updates of the Surviving Sepsis Campaign Guidelines. He is a member of the board of directors and Chief Medical Officer of Sepsis Alliance, a nationwide patient information and advocacy organization.
During his tenure at the University of New Mexico, he contributed to the discovery of a particular form of sepsis, the hantavirus pulmonary syndrome, and published numerous papers on the clinical description, the hemodynamic description, and the approach to supportive care for patients with the syndrome, including extracorporeal hemodynamic and oxygenation support. Dr. Simpson has authored over 180 scientific articles, book chapters, editorials, abstracts and electronic media publications. He was awarded the 2009 Eli Lilly Distinguished Scholar in Critical Care Medicine Award of the American College of Chest Physicians and the 2013 Roger C. Bone Memorial Lecture in Critical Care Medicine, which recognizes career contributions to the field. He has also been recognized as a Distinguished CHEST Educator in 2017 and 2018.
Visual abstracts enhance journal readers’ experience
Physicians’ time is decreasingly their own, and, yet, keeping abreast of clinical literature is increasingly more important. The journal CHEST has introduced a new feature aimed at easing that task and broadening the reach of journal content: visual abstracts.
At the direction of CHEST Editor in Chief Richard Irwin, MD, Master FCCP, Dr. Carroll assembled a team to help carry out an ambitious multimedia strategy (see box). Dr. Irwin charged the Web and Multimedia editorial team with not only extending the reach of journal content but also enhancing readers’ engagement with and understanding of it.
“Our first project was the development of visual abstracts, a type of infographics used to distill the key points of a research abstract into an easily digested graphic form,” says Dr. Carroll, who also is research director of pediatric critical care at Connecticut Children’s Medical Center, Hartford, and a professor of pediatrics at the University of Connecticut School of Medicine, Farmington.
The first visual abstracts were posted to accompany two articles in the July 2018 issue of CHEST. With the exception of August 2018, every issue since has been enhanced with infographics. Insert infographic here (A full gallery of all the visual abstracts so far is available at https://journal.chestnet.org/infographics.) The visual abstracts are available through a number of vehicles: the journal’s website (https://journal.chestnet.org/), the journal’s mobile app (https://journal.chestnet.org/content/mobileaccessinstructions), and social media platforms such as Facebook (https://www.facebook.com/accpchest/) and Twitter (https://twitter.com/accpchest).
“Our goal with the infographics is to promote the exciting research CHEST publishes and to get readers to click through and read the entire article,” says Dr. Carroll. “So far, we’re happy with our results—and we’re looking forward to even greater reach in 2019.”
CHEST Web and Multimedia Section
Editor
Christopher Carroll, MD, MS
Assistant Editors
Yonatan Y. Greenstein, MD, FCCP, Newark, NJ
Roozehra Khan, DO, FCCP, Los Angeles, CA
Dominique J. Pepper, MD, MBChB, MHSc, Bethesda, MD.
###
Physicians’ time is decreasingly their own, and, yet, keeping abreast of clinical literature is increasingly more important. The journal CHEST has introduced a new feature aimed at easing that task and broadening the reach of journal content: visual abstracts.
At the direction of CHEST Editor in Chief Richard Irwin, MD, Master FCCP, Dr. Carroll assembled a team to help carry out an ambitious multimedia strategy (see box). Dr. Irwin charged the Web and Multimedia editorial team with not only extending the reach of journal content but also enhancing readers’ engagement with and understanding of it.
“Our first project was the development of visual abstracts, a type of infographics used to distill the key points of a research abstract into an easily digested graphic form,” says Dr. Carroll, who also is research director of pediatric critical care at Connecticut Children’s Medical Center, Hartford, and a professor of pediatrics at the University of Connecticut School of Medicine, Farmington.
The first visual abstracts were posted to accompany two articles in the July 2018 issue of CHEST. With the exception of August 2018, every issue since has been enhanced with infographics. Insert infographic here (A full gallery of all the visual abstracts so far is available at https://journal.chestnet.org/infographics.) The visual abstracts are available through a number of vehicles: the journal’s website (https://journal.chestnet.org/), the journal’s mobile app (https://journal.chestnet.org/content/mobileaccessinstructions), and social media platforms such as Facebook (https://www.facebook.com/accpchest/) and Twitter (https://twitter.com/accpchest).
“Our goal with the infographics is to promote the exciting research CHEST publishes and to get readers to click through and read the entire article,” says Dr. Carroll. “So far, we’re happy with our results—and we’re looking forward to even greater reach in 2019.”
CHEST Web and Multimedia Section
Editor
Christopher Carroll, MD, MS
Assistant Editors
Yonatan Y. Greenstein, MD, FCCP, Newark, NJ
Roozehra Khan, DO, FCCP, Los Angeles, CA
Dominique J. Pepper, MD, MBChB, MHSc, Bethesda, MD.
###
Physicians’ time is decreasingly their own, and, yet, keeping abreast of clinical literature is increasingly more important. The journal CHEST has introduced a new feature aimed at easing that task and broadening the reach of journal content: visual abstracts.
At the direction of CHEST Editor in Chief Richard Irwin, MD, Master FCCP, Dr. Carroll assembled a team to help carry out an ambitious multimedia strategy (see box). Dr. Irwin charged the Web and Multimedia editorial team with not only extending the reach of journal content but also enhancing readers’ engagement with and understanding of it.
“Our first project was the development of visual abstracts, a type of infographics used to distill the key points of a research abstract into an easily digested graphic form,” says Dr. Carroll, who also is research director of pediatric critical care at Connecticut Children’s Medical Center, Hartford, and a professor of pediatrics at the University of Connecticut School of Medicine, Farmington.
The first visual abstracts were posted to accompany two articles in the July 2018 issue of CHEST. With the exception of August 2018, every issue since has been enhanced with infographics. Insert infographic here (A full gallery of all the visual abstracts so far is available at https://journal.chestnet.org/infographics.) The visual abstracts are available through a number of vehicles: the journal’s website (https://journal.chestnet.org/), the journal’s mobile app (https://journal.chestnet.org/content/mobileaccessinstructions), and social media platforms such as Facebook (https://www.facebook.com/accpchest/) and Twitter (https://twitter.com/accpchest).
“Our goal with the infographics is to promote the exciting research CHEST publishes and to get readers to click through and read the entire article,” says Dr. Carroll. “So far, we’re happy with our results—and we’re looking forward to even greater reach in 2019.”
CHEST Web and Multimedia Section
Editor
Christopher Carroll, MD, MS
Assistant Editors
Yonatan Y. Greenstein, MD, FCCP, Newark, NJ
Roozehra Khan, DO, FCCP, Los Angeles, CA
Dominique J. Pepper, MD, MBChB, MHSc, Bethesda, MD.
###
Five steering committees examine the literature
Airways Disorders
Defining and treating early COPD: Can we make a difference?
There is growing evidence that early COPD—before currently accepted spirometric or symptomatic criteria are present—may be an important clinical entity. The primary pathobiologic mechanisms in early COPD development include both abnormal lung development and accelerated lung aging (Augustí et al. Am J Respir Crit Care Med. 2018 Oct 15;198:8:978).
Martinez and colleagues recently proposed defining early COPD as age <50 with 10+ pack-year smoking history and at least one of the following: (1) early airflow limitation (postbronchodilator FEV1/FVC < lower limit of normal), (2) compatible CT scan abnormalities, (3) rapid decline in FEV1 (≥60 mL/yr) that is accelerated relative to FVC (Martinez et al. Am J Respir Crit Care Med. 2018 Jun 15;197[12]:1540).
A novel multiresolution CT scan imaging protocol described by Koo and coworkers found that substantial loss of small airways— specifically the terminal and transitional bronchioles—occurs in patients with mild-to-moderate COPD even prior to the development of emphysema on CT scan. These findings show that significant destruction of the small airways has occurred prior to the development of mild COPD (Koo et al. Lancet Respir Med. 2018 Aug;6:591).
Pharmacologic treatment for COPD is targeted at the reduction of symptoms and risk of exacerbation, as there remains no conclusive evidence that existing therapies modify long-term decline in lung function. It is unknown if pharmacotherapy for “early COPD” will alter the disease course. While not directly addressing this subset, information may be gleaned from trials on younger, more mild GOLD Stage 1 or Stage 2 patients. The Tie-COPD trial, the largest powered study to date of mild-to-moderate COPD, found that among patients with GOLD stage 1 or 2 COPD treatment with tiotropium compared with placebo for 2 years resulted in significantly higher FEV1 before bronchodilator use (between group difference of 157 mL) and slowed annual decline in FEV1 after bronchodilator use (Zhou et al. N Engl J Med. 2017 Sep 7;377[10]:923).
As our understanding of heterogeneity within COPD increases, striving for improved outcomes from our therapies—an impact on lung function in addition to symptom and exacerbation risk—may need to begin with the study of earlier treatment.
Megan Conroy, MD
Steering Committee Fellow-in-Training
Allen J. Blaivas, DO, FCCP
Steering Committee Vice-Chair
Clinical Pulmonary Medicine
Asthma-COPD overlap: An underappreciated phenotype of obstructive airway disease (OAD)
Asthma-COPD overlap (ACO) is a common yet underappreciated clinical entity within the complex OAD spectrum. Currently, there is no consensus criteria to define ACO; however, a roundtable consensus from an international group (Sin et al. Eur Respir J. 2016 Sep;48:664) suggests using major and minor criteria, with key features being airflow limitation, asthma history, and cigarette or biomass exposure. Several studies have shown that patients with ACO have severe disease, faster lung function decline, greater morbidity and mortality, and lower QoL (Alshabanat et al. PLoS One. 2015 Sep 3;10:e0136065).
There is paucity of data on the pathophysiology, risk factors, and clinical management given exclusion of these patients from clinical trials of asthma and COPD. Indeed, clinicians and researchers now realize that ACO is an umbrella term for multiple subphenotypes, including patients who have predominant asthma with some COPD features and others with predominant COPD with some asthma features. Overall, IgE level, FeNO, sputum, and blood eosinophils are usually higher in ACO than in COPD and relatively similar compared with asthma (Kobayashi et al. Int J Chron Obs Pulmon Dis. 2016 May 26;11:2117).
Most recently, a longitudinal study looked at predictors of ACO among NY firefighters exposed to WTC dust (Singh et al. CHEST. 2018 Dec;154[6]:1301). Pre-exposure low lung function and elevated blood eosinophils and IL4 (T2 inflammatory cytokine) increased risk of developing ACO among those exposed to WTC dust. Further research is required to better understand the interaction of environmental exposure and risk factors in the pathophysiology of ACO. It may be more pragmatic to use the unifying term OAD, as originally proposed in the Dutch hypothesis, and further delineate how several phenotypes of airway disease can be classified by combining traditional approaches with molecular and genomic analysis.
Munish Luthra, MD, FCCP
Steering Committee Member
Samantha D’Annunzio, MD
Steering Committee Member
Critical Care
Mechanical ventilation: One size fits all?
Mechanical ventilation (MV) is a lifesaving intervention in the ICU, but it has been associated with numerous complications ranging from overuse of sedation, atelectasis, and baro or volutrauma.
After 2000, it became well known that using a low tidal volume (VT) strategy (6 mL/kg predicted body weight, PBW) in patients with ARDS produced lower mortality and more ventilator-free days (N Engl J Med. 2000 May 4;342[18]:1301). In addition, a meta-analysis in 2012 demonstrated a lower relative risk of new lung injury, mortality, and pulmonary infections with low VT in non-ARDS patients (Serpa et al. JAMA. 2012 Oct 24/31;308[16]:1651). However, the included studies varied widely in their use of VT (9-12 mL/kg), duration of MV, and in mixed settings (ICU or operating room).
Recently, a large randomized clinical trial compared the effect of low (4-6 mL/kg, PBW) vs intermediate (8-10 mL/kg, PBW) VT ventilation strategy in non-ARDS ICU patients. Interestingly, the study concluded that there is no significant difference in ventilator-free days (21 days in each group), median length ICU and hospital stay, ICU mortality rates, and 28- and 90-day mortality. Also, there was no difference in new-onset ARDS, severe atelectasis, sedation use, and delirium (JAMA. 2018; 320[18]:1872). This study suggests that in non-ARDS patients, MV should be individualized according to each patient’s clinical situation, the nature of the disease, and its effect on lung mechanics, especially in patients who cannot tolerate low tidal volumes.
Margaret A. Disselkamp, MD
Steering Committee Member
Mohammed A. Megri, MD
Fellow-in-Training Steering Committee Member
Home-Based Mechanical Ventilation and Neuromuscular Disease
Improving access to sleep medicine care for patients with NMD
Sleep-disordered breathing (SDB) occurs in up to 5% of children, with adverse implications for growth and development. Children with neuromuscular disease are at significantly higher risk than unaffected children (Chiang et al. Children. 2018;5:e78). Respiratory dysfunction that may present as SDB before daytime impairment in gas exchange is evident. Diagnosing and treating SDB (to include OSA, CSA, and hypoventilation syndromes) early can significantly improve morbidity and mortality.
Unfortunately, diagnostic sleep medicine resources are limited. Children may wait up to a year or more for definitive testing with in-laboratory, attended polysomnography (PSG). Among children with neuromuscular disease, fewer than 10% may undergo a sleep clinic evaluation, and, of those that do, they may have only one visit over a 3-year period of care (Rose et al. Pediatr Pulmonol. 2018 Oct;53:1378). Home sleep testing (HST) has been evaluated as an alternative to PSG given lower cost, availability, and advantage of the child sleeping in his/her own bed. Although HST is indicated in adults with a high pretest probability for moderate to severe OSA, it is not indicated in children, given the potential to underestimate disease severity or to miss the diagnosis entirely (Kirk et al. J Clin Sleep Med. 2017 Oct 15;13[10]:1199). HST lacks electroencephalogram (EEG) and capnography. Technical recording mishaps are more common in children, but in-lab PSG has the advantage of on-site troubleshooting by a technologist.
A recently published study by Fishman and colleagues attempted to compare gold standard in-lab PSG to HST with capnography (Fishman et al. J Clin Sleep Med. 2018 Dec 15;14[12]:2013). Despite a well-designed study with a carefully selected population, HST failed to reliably diagnose SDB. HST underestimated disease severity and, in some cases, missed the diagnosis of SDB entirely. The addition of end tidal CO2 monitoring failed to improve diagnostic accuracy, and HST and PSG-ETco2 values were poorly correlated.
Although children with neuromuscular disease face long wait times for sleep evaluations, HST is clearly not the solution for now. It remains to be seen if innovations in HST with extended monitoring (and transcutaneous CO2) become viable. In the meantime, finding ways to improve access to sleep medicine care for children with neuromuscular disease is a must.
Jacob Collen, MD, FCCP
Steering Committee Member
Interstitial and Diffuse Lung Disease
Idiopathic pneumonias that are not all that idiopathic
Despite being defined as an individual entity for research purposes in 2015 (Fisher et al. Eur Respir J. 2015;46:976), interstitial pneumonias with autoimmune features (IPAF) remain a heterogeneous group of interstitial lung diseases that puzzle the clinician. Since the introduction of the IPAF definition, there have been attempts to validate the diagnostic criteria and study their prognostic implications. Some of these studies showed differential prognosis in patients who met the IPAF criteria (Oldham et al. Eur Respir J. 2016;47:1767).
Although the implications of the presence of autoimmune antibodies in idiopathic interstitial pneumonias (IIPs) is not fully understood, the treatment often entails immunosuppression, especially in those with non-UIP patterns of disease and/or clinical features of autoimmune disease. The stakes are high when IIPs are associated with antibodies correlated with rapidly progressive disease, such as MDA-5 antibody or antisynthetase antibodies. Pulmonologists often lack the clinical expertise to detect occult autoimmune disorders, though the role of the rheumatologist in facilitating the diagnosis and treatment of IPAF is not well delineated. Most health-care systems are not equipped with collaborative ILD-rheumatology clinics or even easy access to a rheumatologist. There is a need for real-world pragmatic studies to establish the optimal way to evaluate patients with ILD for autoimmune features and identify patients who would benefit most from an early referral to rheumatology to aid with diagnosis, treatment, and sometimes monitoring for extrapulmonary manifestations of autoimmune disorders.
Avanthika Thanushi Wynn, MD
Steering Committee Fellow-in-Training
Airways Disorders
Defining and treating early COPD: Can we make a difference?
There is growing evidence that early COPD—before currently accepted spirometric or symptomatic criteria are present—may be an important clinical entity. The primary pathobiologic mechanisms in early COPD development include both abnormal lung development and accelerated lung aging (Augustí et al. Am J Respir Crit Care Med. 2018 Oct 15;198:8:978).
Martinez and colleagues recently proposed defining early COPD as age <50 with 10+ pack-year smoking history and at least one of the following: (1) early airflow limitation (postbronchodilator FEV1/FVC < lower limit of normal), (2) compatible CT scan abnormalities, (3) rapid decline in FEV1 (≥60 mL/yr) that is accelerated relative to FVC (Martinez et al. Am J Respir Crit Care Med. 2018 Jun 15;197[12]:1540).
A novel multiresolution CT scan imaging protocol described by Koo and coworkers found that substantial loss of small airways— specifically the terminal and transitional bronchioles—occurs in patients with mild-to-moderate COPD even prior to the development of emphysema on CT scan. These findings show that significant destruction of the small airways has occurred prior to the development of mild COPD (Koo et al. Lancet Respir Med. 2018 Aug;6:591).
Pharmacologic treatment for COPD is targeted at the reduction of symptoms and risk of exacerbation, as there remains no conclusive evidence that existing therapies modify long-term decline in lung function. It is unknown if pharmacotherapy for “early COPD” will alter the disease course. While not directly addressing this subset, information may be gleaned from trials on younger, more mild GOLD Stage 1 or Stage 2 patients. The Tie-COPD trial, the largest powered study to date of mild-to-moderate COPD, found that among patients with GOLD stage 1 or 2 COPD treatment with tiotropium compared with placebo for 2 years resulted in significantly higher FEV1 before bronchodilator use (between group difference of 157 mL) and slowed annual decline in FEV1 after bronchodilator use (Zhou et al. N Engl J Med. 2017 Sep 7;377[10]:923).
As our understanding of heterogeneity within COPD increases, striving for improved outcomes from our therapies—an impact on lung function in addition to symptom and exacerbation risk—may need to begin with the study of earlier treatment.
Megan Conroy, MD
Steering Committee Fellow-in-Training
Allen J. Blaivas, DO, FCCP
Steering Committee Vice-Chair
Clinical Pulmonary Medicine
Asthma-COPD overlap: An underappreciated phenotype of obstructive airway disease (OAD)
Asthma-COPD overlap (ACO) is a common yet underappreciated clinical entity within the complex OAD spectrum. Currently, there is no consensus criteria to define ACO; however, a roundtable consensus from an international group (Sin et al. Eur Respir J. 2016 Sep;48:664) suggests using major and minor criteria, with key features being airflow limitation, asthma history, and cigarette or biomass exposure. Several studies have shown that patients with ACO have severe disease, faster lung function decline, greater morbidity and mortality, and lower QoL (Alshabanat et al. PLoS One. 2015 Sep 3;10:e0136065).
There is paucity of data on the pathophysiology, risk factors, and clinical management given exclusion of these patients from clinical trials of asthma and COPD. Indeed, clinicians and researchers now realize that ACO is an umbrella term for multiple subphenotypes, including patients who have predominant asthma with some COPD features and others with predominant COPD with some asthma features. Overall, IgE level, FeNO, sputum, and blood eosinophils are usually higher in ACO than in COPD and relatively similar compared with asthma (Kobayashi et al. Int J Chron Obs Pulmon Dis. 2016 May 26;11:2117).
Most recently, a longitudinal study looked at predictors of ACO among NY firefighters exposed to WTC dust (Singh et al. CHEST. 2018 Dec;154[6]:1301). Pre-exposure low lung function and elevated blood eosinophils and IL4 (T2 inflammatory cytokine) increased risk of developing ACO among those exposed to WTC dust. Further research is required to better understand the interaction of environmental exposure and risk factors in the pathophysiology of ACO. It may be more pragmatic to use the unifying term OAD, as originally proposed in the Dutch hypothesis, and further delineate how several phenotypes of airway disease can be classified by combining traditional approaches with molecular and genomic analysis.
Munish Luthra, MD, FCCP
Steering Committee Member
Samantha D’Annunzio, MD
Steering Committee Member
Critical Care
Mechanical ventilation: One size fits all?
Mechanical ventilation (MV) is a lifesaving intervention in the ICU, but it has been associated with numerous complications ranging from overuse of sedation, atelectasis, and baro or volutrauma.
After 2000, it became well known that using a low tidal volume (VT) strategy (6 mL/kg predicted body weight, PBW) in patients with ARDS produced lower mortality and more ventilator-free days (N Engl J Med. 2000 May 4;342[18]:1301). In addition, a meta-analysis in 2012 demonstrated a lower relative risk of new lung injury, mortality, and pulmonary infections with low VT in non-ARDS patients (Serpa et al. JAMA. 2012 Oct 24/31;308[16]:1651). However, the included studies varied widely in their use of VT (9-12 mL/kg), duration of MV, and in mixed settings (ICU or operating room).
Recently, a large randomized clinical trial compared the effect of low (4-6 mL/kg, PBW) vs intermediate (8-10 mL/kg, PBW) VT ventilation strategy in non-ARDS ICU patients. Interestingly, the study concluded that there is no significant difference in ventilator-free days (21 days in each group), median length ICU and hospital stay, ICU mortality rates, and 28- and 90-day mortality. Also, there was no difference in new-onset ARDS, severe atelectasis, sedation use, and delirium (JAMA. 2018; 320[18]:1872). This study suggests that in non-ARDS patients, MV should be individualized according to each patient’s clinical situation, the nature of the disease, and its effect on lung mechanics, especially in patients who cannot tolerate low tidal volumes.
Margaret A. Disselkamp, MD
Steering Committee Member
Mohammed A. Megri, MD
Fellow-in-Training Steering Committee Member
Home-Based Mechanical Ventilation and Neuromuscular Disease
Improving access to sleep medicine care for patients with NMD
Sleep-disordered breathing (SDB) occurs in up to 5% of children, with adverse implications for growth and development. Children with neuromuscular disease are at significantly higher risk than unaffected children (Chiang et al. Children. 2018;5:e78). Respiratory dysfunction that may present as SDB before daytime impairment in gas exchange is evident. Diagnosing and treating SDB (to include OSA, CSA, and hypoventilation syndromes) early can significantly improve morbidity and mortality.
Unfortunately, diagnostic sleep medicine resources are limited. Children may wait up to a year or more for definitive testing with in-laboratory, attended polysomnography (PSG). Among children with neuromuscular disease, fewer than 10% may undergo a sleep clinic evaluation, and, of those that do, they may have only one visit over a 3-year period of care (Rose et al. Pediatr Pulmonol. 2018 Oct;53:1378). Home sleep testing (HST) has been evaluated as an alternative to PSG given lower cost, availability, and advantage of the child sleeping in his/her own bed. Although HST is indicated in adults with a high pretest probability for moderate to severe OSA, it is not indicated in children, given the potential to underestimate disease severity or to miss the diagnosis entirely (Kirk et al. J Clin Sleep Med. 2017 Oct 15;13[10]:1199). HST lacks electroencephalogram (EEG) and capnography. Technical recording mishaps are more common in children, but in-lab PSG has the advantage of on-site troubleshooting by a technologist.
A recently published study by Fishman and colleagues attempted to compare gold standard in-lab PSG to HST with capnography (Fishman et al. J Clin Sleep Med. 2018 Dec 15;14[12]:2013). Despite a well-designed study with a carefully selected population, HST failed to reliably diagnose SDB. HST underestimated disease severity and, in some cases, missed the diagnosis of SDB entirely. The addition of end tidal CO2 monitoring failed to improve diagnostic accuracy, and HST and PSG-ETco2 values were poorly correlated.
Although children with neuromuscular disease face long wait times for sleep evaluations, HST is clearly not the solution for now. It remains to be seen if innovations in HST with extended monitoring (and transcutaneous CO2) become viable. In the meantime, finding ways to improve access to sleep medicine care for children with neuromuscular disease is a must.
Jacob Collen, MD, FCCP
Steering Committee Member
Interstitial and Diffuse Lung Disease
Idiopathic pneumonias that are not all that idiopathic
Despite being defined as an individual entity for research purposes in 2015 (Fisher et al. Eur Respir J. 2015;46:976), interstitial pneumonias with autoimmune features (IPAF) remain a heterogeneous group of interstitial lung diseases that puzzle the clinician. Since the introduction of the IPAF definition, there have been attempts to validate the diagnostic criteria and study their prognostic implications. Some of these studies showed differential prognosis in patients who met the IPAF criteria (Oldham et al. Eur Respir J. 2016;47:1767).
Although the implications of the presence of autoimmune antibodies in idiopathic interstitial pneumonias (IIPs) is not fully understood, the treatment often entails immunosuppression, especially in those with non-UIP patterns of disease and/or clinical features of autoimmune disease. The stakes are high when IIPs are associated with antibodies correlated with rapidly progressive disease, such as MDA-5 antibody or antisynthetase antibodies. Pulmonologists often lack the clinical expertise to detect occult autoimmune disorders, though the role of the rheumatologist in facilitating the diagnosis and treatment of IPAF is not well delineated. Most health-care systems are not equipped with collaborative ILD-rheumatology clinics or even easy access to a rheumatologist. There is a need for real-world pragmatic studies to establish the optimal way to evaluate patients with ILD for autoimmune features and identify patients who would benefit most from an early referral to rheumatology to aid with diagnosis, treatment, and sometimes monitoring for extrapulmonary manifestations of autoimmune disorders.
Avanthika Thanushi Wynn, MD
Steering Committee Fellow-in-Training
Airways Disorders
Defining and treating early COPD: Can we make a difference?
There is growing evidence that early COPD—before currently accepted spirometric or symptomatic criteria are present—may be an important clinical entity. The primary pathobiologic mechanisms in early COPD development include both abnormal lung development and accelerated lung aging (Augustí et al. Am J Respir Crit Care Med. 2018 Oct 15;198:8:978).
Martinez and colleagues recently proposed defining early COPD as age <50 with 10+ pack-year smoking history and at least one of the following: (1) early airflow limitation (postbronchodilator FEV1/FVC < lower limit of normal), (2) compatible CT scan abnormalities, (3) rapid decline in FEV1 (≥60 mL/yr) that is accelerated relative to FVC (Martinez et al. Am J Respir Crit Care Med. 2018 Jun 15;197[12]:1540).
A novel multiresolution CT scan imaging protocol described by Koo and coworkers found that substantial loss of small airways— specifically the terminal and transitional bronchioles—occurs in patients with mild-to-moderate COPD even prior to the development of emphysema on CT scan. These findings show that significant destruction of the small airways has occurred prior to the development of mild COPD (Koo et al. Lancet Respir Med. 2018 Aug;6:591).
Pharmacologic treatment for COPD is targeted at the reduction of symptoms and risk of exacerbation, as there remains no conclusive evidence that existing therapies modify long-term decline in lung function. It is unknown if pharmacotherapy for “early COPD” will alter the disease course. While not directly addressing this subset, information may be gleaned from trials on younger, more mild GOLD Stage 1 or Stage 2 patients. The Tie-COPD trial, the largest powered study to date of mild-to-moderate COPD, found that among patients with GOLD stage 1 or 2 COPD treatment with tiotropium compared with placebo for 2 years resulted in significantly higher FEV1 before bronchodilator use (between group difference of 157 mL) and slowed annual decline in FEV1 after bronchodilator use (Zhou et al. N Engl J Med. 2017 Sep 7;377[10]:923).
As our understanding of heterogeneity within COPD increases, striving for improved outcomes from our therapies—an impact on lung function in addition to symptom and exacerbation risk—may need to begin with the study of earlier treatment.
Megan Conroy, MD
Steering Committee Fellow-in-Training
Allen J. Blaivas, DO, FCCP
Steering Committee Vice-Chair
Clinical Pulmonary Medicine
Asthma-COPD overlap: An underappreciated phenotype of obstructive airway disease (OAD)
Asthma-COPD overlap (ACO) is a common yet underappreciated clinical entity within the complex OAD spectrum. Currently, there is no consensus criteria to define ACO; however, a roundtable consensus from an international group (Sin et al. Eur Respir J. 2016 Sep;48:664) suggests using major and minor criteria, with key features being airflow limitation, asthma history, and cigarette or biomass exposure. Several studies have shown that patients with ACO have severe disease, faster lung function decline, greater morbidity and mortality, and lower QoL (Alshabanat et al. PLoS One. 2015 Sep 3;10:e0136065).
There is paucity of data on the pathophysiology, risk factors, and clinical management given exclusion of these patients from clinical trials of asthma and COPD. Indeed, clinicians and researchers now realize that ACO is an umbrella term for multiple subphenotypes, including patients who have predominant asthma with some COPD features and others with predominant COPD with some asthma features. Overall, IgE level, FeNO, sputum, and blood eosinophils are usually higher in ACO than in COPD and relatively similar compared with asthma (Kobayashi et al. Int J Chron Obs Pulmon Dis. 2016 May 26;11:2117).
Most recently, a longitudinal study looked at predictors of ACO among NY firefighters exposed to WTC dust (Singh et al. CHEST. 2018 Dec;154[6]:1301). Pre-exposure low lung function and elevated blood eosinophils and IL4 (T2 inflammatory cytokine) increased risk of developing ACO among those exposed to WTC dust. Further research is required to better understand the interaction of environmental exposure and risk factors in the pathophysiology of ACO. It may be more pragmatic to use the unifying term OAD, as originally proposed in the Dutch hypothesis, and further delineate how several phenotypes of airway disease can be classified by combining traditional approaches with molecular and genomic analysis.
Munish Luthra, MD, FCCP
Steering Committee Member
Samantha D’Annunzio, MD
Steering Committee Member
Critical Care
Mechanical ventilation: One size fits all?
Mechanical ventilation (MV) is a lifesaving intervention in the ICU, but it has been associated with numerous complications ranging from overuse of sedation, atelectasis, and baro or volutrauma.
After 2000, it became well known that using a low tidal volume (VT) strategy (6 mL/kg predicted body weight, PBW) in patients with ARDS produced lower mortality and more ventilator-free days (N Engl J Med. 2000 May 4;342[18]:1301). In addition, a meta-analysis in 2012 demonstrated a lower relative risk of new lung injury, mortality, and pulmonary infections with low VT in non-ARDS patients (Serpa et al. JAMA. 2012 Oct 24/31;308[16]:1651). However, the included studies varied widely in their use of VT (9-12 mL/kg), duration of MV, and in mixed settings (ICU or operating room).
Recently, a large randomized clinical trial compared the effect of low (4-6 mL/kg, PBW) vs intermediate (8-10 mL/kg, PBW) VT ventilation strategy in non-ARDS ICU patients. Interestingly, the study concluded that there is no significant difference in ventilator-free days (21 days in each group), median length ICU and hospital stay, ICU mortality rates, and 28- and 90-day mortality. Also, there was no difference in new-onset ARDS, severe atelectasis, sedation use, and delirium (JAMA. 2018; 320[18]:1872). This study suggests that in non-ARDS patients, MV should be individualized according to each patient’s clinical situation, the nature of the disease, and its effect on lung mechanics, especially in patients who cannot tolerate low tidal volumes.
Margaret A. Disselkamp, MD
Steering Committee Member
Mohammed A. Megri, MD
Fellow-in-Training Steering Committee Member
Home-Based Mechanical Ventilation and Neuromuscular Disease
Improving access to sleep medicine care for patients with NMD
Sleep-disordered breathing (SDB) occurs in up to 5% of children, with adverse implications for growth and development. Children with neuromuscular disease are at significantly higher risk than unaffected children (Chiang et al. Children. 2018;5:e78). Respiratory dysfunction that may present as SDB before daytime impairment in gas exchange is evident. Diagnosing and treating SDB (to include OSA, CSA, and hypoventilation syndromes) early can significantly improve morbidity and mortality.
Unfortunately, diagnostic sleep medicine resources are limited. Children may wait up to a year or more for definitive testing with in-laboratory, attended polysomnography (PSG). Among children with neuromuscular disease, fewer than 10% may undergo a sleep clinic evaluation, and, of those that do, they may have only one visit over a 3-year period of care (Rose et al. Pediatr Pulmonol. 2018 Oct;53:1378). Home sleep testing (HST) has been evaluated as an alternative to PSG given lower cost, availability, and advantage of the child sleeping in his/her own bed. Although HST is indicated in adults with a high pretest probability for moderate to severe OSA, it is not indicated in children, given the potential to underestimate disease severity or to miss the diagnosis entirely (Kirk et al. J Clin Sleep Med. 2017 Oct 15;13[10]:1199). HST lacks electroencephalogram (EEG) and capnography. Technical recording mishaps are more common in children, but in-lab PSG has the advantage of on-site troubleshooting by a technologist.
A recently published study by Fishman and colleagues attempted to compare gold standard in-lab PSG to HST with capnography (Fishman et al. J Clin Sleep Med. 2018 Dec 15;14[12]:2013). Despite a well-designed study with a carefully selected population, HST failed to reliably diagnose SDB. HST underestimated disease severity and, in some cases, missed the diagnosis of SDB entirely. The addition of end tidal CO2 monitoring failed to improve diagnostic accuracy, and HST and PSG-ETco2 values were poorly correlated.
Although children with neuromuscular disease face long wait times for sleep evaluations, HST is clearly not the solution for now. It remains to be seen if innovations in HST with extended monitoring (and transcutaneous CO2) become viable. In the meantime, finding ways to improve access to sleep medicine care for children with neuromuscular disease is a must.
Jacob Collen, MD, FCCP
Steering Committee Member
Interstitial and Diffuse Lung Disease
Idiopathic pneumonias that are not all that idiopathic
Despite being defined as an individual entity for research purposes in 2015 (Fisher et al. Eur Respir J. 2015;46:976), interstitial pneumonias with autoimmune features (IPAF) remain a heterogeneous group of interstitial lung diseases that puzzle the clinician. Since the introduction of the IPAF definition, there have been attempts to validate the diagnostic criteria and study their prognostic implications. Some of these studies showed differential prognosis in patients who met the IPAF criteria (Oldham et al. Eur Respir J. 2016;47:1767).
Although the implications of the presence of autoimmune antibodies in idiopathic interstitial pneumonias (IIPs) is not fully understood, the treatment often entails immunosuppression, especially in those with non-UIP patterns of disease and/or clinical features of autoimmune disease. The stakes are high when IIPs are associated with antibodies correlated with rapidly progressive disease, such as MDA-5 antibody or antisynthetase antibodies. Pulmonologists often lack the clinical expertise to detect occult autoimmune disorders, though the role of the rheumatologist in facilitating the diagnosis and treatment of IPAF is not well delineated. Most health-care systems are not equipped with collaborative ILD-rheumatology clinics or even easy access to a rheumatologist. There is a need for real-world pragmatic studies to establish the optimal way to evaluate patients with ILD for autoimmune features and identify patients who would benefit most from an early referral to rheumatology to aid with diagnosis, treatment, and sometimes monitoring for extrapulmonary manifestations of autoimmune disorders.
Avanthika Thanushi Wynn, MD
Steering Committee Fellow-in-Training
Renal replacement therapy in the ICU: Vexed questions and team dynamics
More than 5 million patients are admitted to ICUs each year in the United States, and approximately 2% to 10% of these patients develop acute kidney injury requiring renal replacement therapy (AKI-RRT). AKI-RRT carries high morbidity and mortality (Hoste EA, et al. Intensive Care Med. 2015;41:1411) and is associated with renal and systemic complications, such as cardiovascular disease. RRT, frequently provided by nephrologists and/or intensivists, is a supportive therapy that can be life-saving when provided to the right patient at the right time. However, several questions related to the provision of RRT still remain, including the optimal timing of RRT initiation, the development of quality metrics for optimal RRT deliverables and monitoring, and the optimal strategy of RRT de-escalation and risk-stratification of renal recovery. Overall, there is paucity of randomized trials and standardized risk-stratification tools that can guide RRT in the ICU.
Current vexed questions of RRT deliverables in the ICU
There is ongoing research aiming to answer critical questions that can potentially improve current standards of RRT.
What is the optimal time of RRT initiation for critically ill patients with AKI?
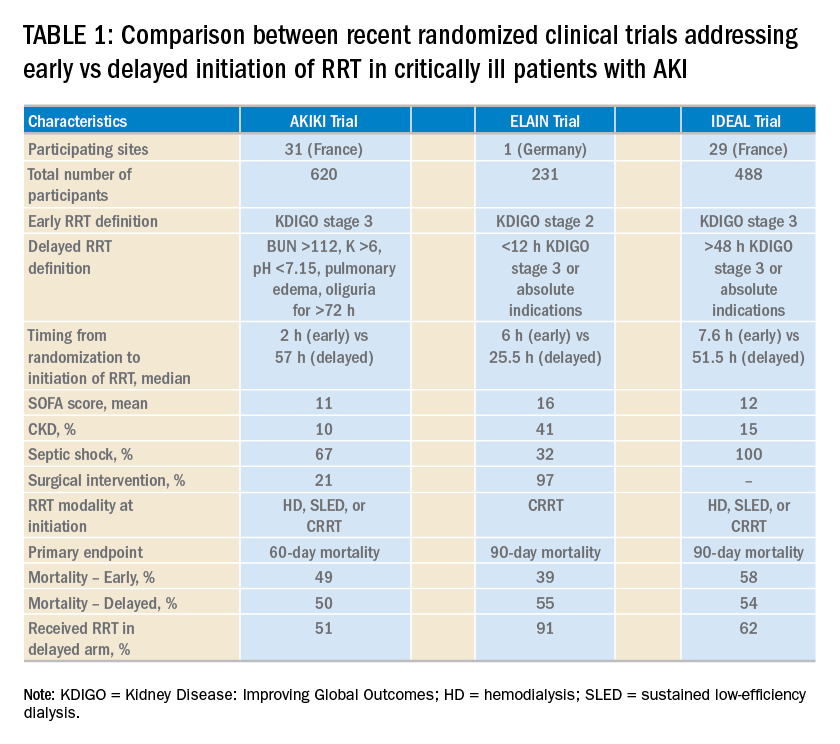
Over the last 2 years, three randomized clinical trials have attempted to address this important question involving heterogeneous ICU populations and distinct research hypotheses and study designs. Two of these studies, AKIKI (Gaudry S, et al. N Engl J Med. 2016;375:122) and IDEAL-ICU (Barbar SD, et al. N Engl J Med. 2018;379:1431) yielded no significant difference in the primary outcome of 60-day and 90-day all-cause mortality between the early vs delayed RRT initiation strategies, respectively (Table 1). Further, AKIKI showed no difference in RRT dependence at 60 days and higher catheter-related infections and hypophosphatemia in the early initiation arm. It is important to note that IDEAL-ICU was stopped early for futility after the second planned interim analysis with only 56% of patients enrolled (
How can RRT deliverables in the ICU be effectively and systematically monitored?
The provision of RRT to ICU patients with AKI requires an iterative adjustment of the RRT prescription and goals of therapy to accommodate changes in the clinical status with emphasis in hemodynamics, multiorgan failure, and fluid overload (Neyra JA. Clin Nephrol. 2018;90:1). The utilization of static and functional tests or point-of-care ultrasonography to assess hemodynamic variables can be useful. Furthermore, the implementation of customized and automated flowsheets in the electronic health record can facilitate remote monitoring. It is, therefore, essential that the multidisciplinary ICU team develops a process to monitor and ensure RRT deliverables. In this context, the standardization and monitoring of quality metrics (dose, modality, anticoagulation, filter life, downtime, etc) and the development of effective quality management systems are critically important. However, big multicenter data are direly needed to provide insight in this arena.
How can renal recovery be assessed and RRT effectively de-escalated?
The continuous examination of renal recovery in ICU patients with AKI-RRT is mostly based on urine output trend and, if feasible, interdialytic solute control. Sometimes, the transition from continuous RRT to intermittent modalities is necessary in the context of multiorgan recovery and de-escalation of care. However, clinical risk-prediction tools that identify patients who can potentially recover or already exhibit early signs of renal function recovery are needed. Current advances in clinical informatics can help to incorporate time-varying clinical parameters that may be informative for risk-prediction models. In addition, incorporating novel biomarkers of AKI repair and functional tests (eg, furosemide stress test, functional MRI) into these models may further inform these tools and aid the development of clinical decision support systems that enhance interventions to promote AKI recovery (Neyra JA, et al. Nephron. 2018;140: 99).
Is post-AKI outpatient care beneficial for ICU survivors who suffered from AKI-RRT?
Specialized AKI survivor clinics have been implemented in some centers. In general, this outpatient follow-up model includes survivors who suffered from AKI stage 2 or 3, some of them requiring RRT, and tailors individualized interventions for post-AKI complications (preventing recurrent AKI, attenuating incident or progressive CKD). However, the value of this outpatient model needs to be further evaluated with emphasis on clinical outcomes (eg, recurrent AKI, CKD, readmissions, or death) and elements that impact quality of life. This is an area of evolving research and a great opportunity for the nephrology and critical care communities to integrate and enhance post-ICU outpatient care and research collaboration.
Interdisciplinary communication among acute care team members
Two essential elements to provide effective RRT to ICU patients with AKI are: (1) the dynamics of the ICU team (intensivists, nephrologists, pharmacists, nurses, nutritionists, physical therapists, etc) to enhance the delivery of personalized therapy (RRT candidacy, timing of initiation, goals for solute control and fluid removal/regulation, renal recovery evaluation, RRT de-escalation, etc.) and (2) the frequent assessment and adjustment of RRT goals according to the clinical status of the patient. Therefore, effective RRT provision in the ICU requires the development of optimal channels of communication among all members of the acute care team and the systematic monitoring of the clinical status of the patient and RRT-specific goals and deliverables.
Perspective from a nurse and quality improvement officer for the provision of RRT in the ICU
The provision of continuous RRT (CRRT) to critically ill patients requires close communication between the bedside nurse and the rest of the ICU team. The physician typically prescribes CRRT and determines the specific goals of therapy. The pharmacist works closely with the nephrologist/intensivist and bedside nurse, especially in regards to customized CRRT solutions (when indicated) and medication dosing. Because CRRT can alter drug pharmacokinetics, the pharmacist closely and constantly monitors the patient’s clinical status, CRRT prescription, and all active medications. CRRT can also affect the nutritional and metabolic status of critically ill patients; therefore, the input of the nutritionist is necessary. The syndrome of ICU-acquired weakness is commonly encountered in ICU patients and is related to physical immobility. While ICU patients with AKI are already at risk for decreased mobility, the continuous connection to an immobile extracorporeal machine for the provision of CRRT may further contribute to immobilization and can also preclude the provision of optimal physical therapy. Therefore, the bedside nurse should assist the physical therapist for the timely and effective delivery of physical therapy according to the clinical status of the patient.
The clinical scenarios discussed above provide a small glimpse into the importance of developing an interdisciplinary ICU team caring for critically ill patients receiving CRRT. In the context of how integral the specific role of each team member is, it becomes clear that the bedside nurse’s role is not only to deliver hands-on patient care but also the orchestration of collaborative communication among all health-care providers for the effective provision of CRRT to critically ill patients in the ICU.
Dr. Neyra and Ms. Hauschild are with the Department of Internal Medicine; Division of Nephrology; Bone and Mineral Metabolism; University of Kentucky; Lexington, Kentucky.
More than 5 million patients are admitted to ICUs each year in the United States, and approximately 2% to 10% of these patients develop acute kidney injury requiring renal replacement therapy (AKI-RRT). AKI-RRT carries high morbidity and mortality (Hoste EA, et al. Intensive Care Med. 2015;41:1411) and is associated with renal and systemic complications, such as cardiovascular disease. RRT, frequently provided by nephrologists and/or intensivists, is a supportive therapy that can be life-saving when provided to the right patient at the right time. However, several questions related to the provision of RRT still remain, including the optimal timing of RRT initiation, the development of quality metrics for optimal RRT deliverables and monitoring, and the optimal strategy of RRT de-escalation and risk-stratification of renal recovery. Overall, there is paucity of randomized trials and standardized risk-stratification tools that can guide RRT in the ICU.
Current vexed questions of RRT deliverables in the ICU
There is ongoing research aiming to answer critical questions that can potentially improve current standards of RRT.
What is the optimal time of RRT initiation for critically ill patients with AKI?
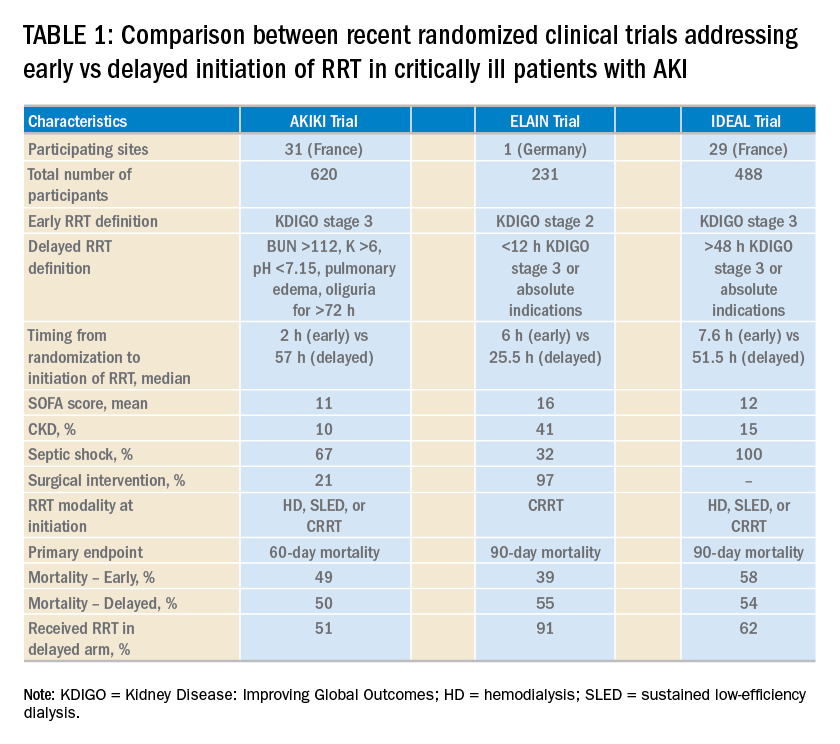
Over the last 2 years, three randomized clinical trials have attempted to address this important question involving heterogeneous ICU populations and distinct research hypotheses and study designs. Two of these studies, AKIKI (Gaudry S, et al. N Engl J Med. 2016;375:122) and IDEAL-ICU (Barbar SD, et al. N Engl J Med. 2018;379:1431) yielded no significant difference in the primary outcome of 60-day and 90-day all-cause mortality between the early vs delayed RRT initiation strategies, respectively (Table 1). Further, AKIKI showed no difference in RRT dependence at 60 days and higher catheter-related infections and hypophosphatemia in the early initiation arm. It is important to note that IDEAL-ICU was stopped early for futility after the second planned interim analysis with only 56% of patients enrolled (
How can RRT deliverables in the ICU be effectively and systematically monitored?
The provision of RRT to ICU patients with AKI requires an iterative adjustment of the RRT prescription and goals of therapy to accommodate changes in the clinical status with emphasis in hemodynamics, multiorgan failure, and fluid overload (Neyra JA. Clin Nephrol. 2018;90:1). The utilization of static and functional tests or point-of-care ultrasonography to assess hemodynamic variables can be useful. Furthermore, the implementation of customized and automated flowsheets in the electronic health record can facilitate remote monitoring. It is, therefore, essential that the multidisciplinary ICU team develops a process to monitor and ensure RRT deliverables. In this context, the standardization and monitoring of quality metrics (dose, modality, anticoagulation, filter life, downtime, etc) and the development of effective quality management systems are critically important. However, big multicenter data are direly needed to provide insight in this arena.
How can renal recovery be assessed and RRT effectively de-escalated?
The continuous examination of renal recovery in ICU patients with AKI-RRT is mostly based on urine output trend and, if feasible, interdialytic solute control. Sometimes, the transition from continuous RRT to intermittent modalities is necessary in the context of multiorgan recovery and de-escalation of care. However, clinical risk-prediction tools that identify patients who can potentially recover or already exhibit early signs of renal function recovery are needed. Current advances in clinical informatics can help to incorporate time-varying clinical parameters that may be informative for risk-prediction models. In addition, incorporating novel biomarkers of AKI repair and functional tests (eg, furosemide stress test, functional MRI) into these models may further inform these tools and aid the development of clinical decision support systems that enhance interventions to promote AKI recovery (Neyra JA, et al. Nephron. 2018;140: 99).
Is post-AKI outpatient care beneficial for ICU survivors who suffered from AKI-RRT?
Specialized AKI survivor clinics have been implemented in some centers. In general, this outpatient follow-up model includes survivors who suffered from AKI stage 2 or 3, some of them requiring RRT, and tailors individualized interventions for post-AKI complications (preventing recurrent AKI, attenuating incident or progressive CKD). However, the value of this outpatient model needs to be further evaluated with emphasis on clinical outcomes (eg, recurrent AKI, CKD, readmissions, or death) and elements that impact quality of life. This is an area of evolving research and a great opportunity for the nephrology and critical care communities to integrate and enhance post-ICU outpatient care and research collaboration.
Interdisciplinary communication among acute care team members
Two essential elements to provide effective RRT to ICU patients with AKI are: (1) the dynamics of the ICU team (intensivists, nephrologists, pharmacists, nurses, nutritionists, physical therapists, etc) to enhance the delivery of personalized therapy (RRT candidacy, timing of initiation, goals for solute control and fluid removal/regulation, renal recovery evaluation, RRT de-escalation, etc.) and (2) the frequent assessment and adjustment of RRT goals according to the clinical status of the patient. Therefore, effective RRT provision in the ICU requires the development of optimal channels of communication among all members of the acute care team and the systematic monitoring of the clinical status of the patient and RRT-specific goals and deliverables.
Perspective from a nurse and quality improvement officer for the provision of RRT in the ICU
The provision of continuous RRT (CRRT) to critically ill patients requires close communication between the bedside nurse and the rest of the ICU team. The physician typically prescribes CRRT and determines the specific goals of therapy. The pharmacist works closely with the nephrologist/intensivist and bedside nurse, especially in regards to customized CRRT solutions (when indicated) and medication dosing. Because CRRT can alter drug pharmacokinetics, the pharmacist closely and constantly monitors the patient’s clinical status, CRRT prescription, and all active medications. CRRT can also affect the nutritional and metabolic status of critically ill patients; therefore, the input of the nutritionist is necessary. The syndrome of ICU-acquired weakness is commonly encountered in ICU patients and is related to physical immobility. While ICU patients with AKI are already at risk for decreased mobility, the continuous connection to an immobile extracorporeal machine for the provision of CRRT may further contribute to immobilization and can also preclude the provision of optimal physical therapy. Therefore, the bedside nurse should assist the physical therapist for the timely and effective delivery of physical therapy according to the clinical status of the patient.
The clinical scenarios discussed above provide a small glimpse into the importance of developing an interdisciplinary ICU team caring for critically ill patients receiving CRRT. In the context of how integral the specific role of each team member is, it becomes clear that the bedside nurse’s role is not only to deliver hands-on patient care but also the orchestration of collaborative communication among all health-care providers for the effective provision of CRRT to critically ill patients in the ICU.
Dr. Neyra and Ms. Hauschild are with the Department of Internal Medicine; Division of Nephrology; Bone and Mineral Metabolism; University of Kentucky; Lexington, Kentucky.
More than 5 million patients are admitted to ICUs each year in the United States, and approximately 2% to 10% of these patients develop acute kidney injury requiring renal replacement therapy (AKI-RRT). AKI-RRT carries high morbidity and mortality (Hoste EA, et al. Intensive Care Med. 2015;41:1411) and is associated with renal and systemic complications, such as cardiovascular disease. RRT, frequently provided by nephrologists and/or intensivists, is a supportive therapy that can be life-saving when provided to the right patient at the right time. However, several questions related to the provision of RRT still remain, including the optimal timing of RRT initiation, the development of quality metrics for optimal RRT deliverables and monitoring, and the optimal strategy of RRT de-escalation and risk-stratification of renal recovery. Overall, there is paucity of randomized trials and standardized risk-stratification tools that can guide RRT in the ICU.
Current vexed questions of RRT deliverables in the ICU
There is ongoing research aiming to answer critical questions that can potentially improve current standards of RRT.
What is the optimal time of RRT initiation for critically ill patients with AKI?
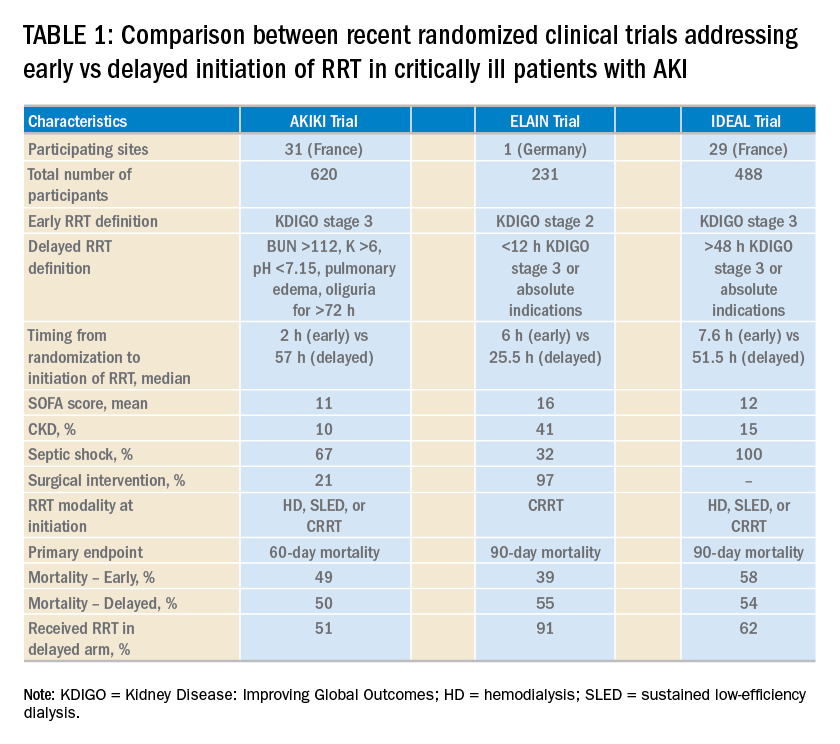
Over the last 2 years, three randomized clinical trials have attempted to address this important question involving heterogeneous ICU populations and distinct research hypotheses and study designs. Two of these studies, AKIKI (Gaudry S, et al. N Engl J Med. 2016;375:122) and IDEAL-ICU (Barbar SD, et al. N Engl J Med. 2018;379:1431) yielded no significant difference in the primary outcome of 60-day and 90-day all-cause mortality between the early vs delayed RRT initiation strategies, respectively (Table 1). Further, AKIKI showed no difference in RRT dependence at 60 days and higher catheter-related infections and hypophosphatemia in the early initiation arm. It is important to note that IDEAL-ICU was stopped early for futility after the second planned interim analysis with only 56% of patients enrolled (
How can RRT deliverables in the ICU be effectively and systematically monitored?
The provision of RRT to ICU patients with AKI requires an iterative adjustment of the RRT prescription and goals of therapy to accommodate changes in the clinical status with emphasis in hemodynamics, multiorgan failure, and fluid overload (Neyra JA. Clin Nephrol. 2018;90:1). The utilization of static and functional tests or point-of-care ultrasonography to assess hemodynamic variables can be useful. Furthermore, the implementation of customized and automated flowsheets in the electronic health record can facilitate remote monitoring. It is, therefore, essential that the multidisciplinary ICU team develops a process to monitor and ensure RRT deliverables. In this context, the standardization and monitoring of quality metrics (dose, modality, anticoagulation, filter life, downtime, etc) and the development of effective quality management systems are critically important. However, big multicenter data are direly needed to provide insight in this arena.
How can renal recovery be assessed and RRT effectively de-escalated?
The continuous examination of renal recovery in ICU patients with AKI-RRT is mostly based on urine output trend and, if feasible, interdialytic solute control. Sometimes, the transition from continuous RRT to intermittent modalities is necessary in the context of multiorgan recovery and de-escalation of care. However, clinical risk-prediction tools that identify patients who can potentially recover or already exhibit early signs of renal function recovery are needed. Current advances in clinical informatics can help to incorporate time-varying clinical parameters that may be informative for risk-prediction models. In addition, incorporating novel biomarkers of AKI repair and functional tests (eg, furosemide stress test, functional MRI) into these models may further inform these tools and aid the development of clinical decision support systems that enhance interventions to promote AKI recovery (Neyra JA, et al. Nephron. 2018;140: 99).
Is post-AKI outpatient care beneficial for ICU survivors who suffered from AKI-RRT?
Specialized AKI survivor clinics have been implemented in some centers. In general, this outpatient follow-up model includes survivors who suffered from AKI stage 2 or 3, some of them requiring RRT, and tailors individualized interventions for post-AKI complications (preventing recurrent AKI, attenuating incident or progressive CKD). However, the value of this outpatient model needs to be further evaluated with emphasis on clinical outcomes (eg, recurrent AKI, CKD, readmissions, or death) and elements that impact quality of life. This is an area of evolving research and a great opportunity for the nephrology and critical care communities to integrate and enhance post-ICU outpatient care and research collaboration.
Interdisciplinary communication among acute care team members
Two essential elements to provide effective RRT to ICU patients with AKI are: (1) the dynamics of the ICU team (intensivists, nephrologists, pharmacists, nurses, nutritionists, physical therapists, etc) to enhance the delivery of personalized therapy (RRT candidacy, timing of initiation, goals for solute control and fluid removal/regulation, renal recovery evaluation, RRT de-escalation, etc.) and (2) the frequent assessment and adjustment of RRT goals according to the clinical status of the patient. Therefore, effective RRT provision in the ICU requires the development of optimal channels of communication among all members of the acute care team and the systematic monitoring of the clinical status of the patient and RRT-specific goals and deliverables.
Perspective from a nurse and quality improvement officer for the provision of RRT in the ICU
The provision of continuous RRT (CRRT) to critically ill patients requires close communication between the bedside nurse and the rest of the ICU team. The physician typically prescribes CRRT and determines the specific goals of therapy. The pharmacist works closely with the nephrologist/intensivist and bedside nurse, especially in regards to customized CRRT solutions (when indicated) and medication dosing. Because CRRT can alter drug pharmacokinetics, the pharmacist closely and constantly monitors the patient’s clinical status, CRRT prescription, and all active medications. CRRT can also affect the nutritional and metabolic status of critically ill patients; therefore, the input of the nutritionist is necessary. The syndrome of ICU-acquired weakness is commonly encountered in ICU patients and is related to physical immobility. While ICU patients with AKI are already at risk for decreased mobility, the continuous connection to an immobile extracorporeal machine for the provision of CRRT may further contribute to immobilization and can also preclude the provision of optimal physical therapy. Therefore, the bedside nurse should assist the physical therapist for the timely and effective delivery of physical therapy according to the clinical status of the patient.
The clinical scenarios discussed above provide a small glimpse into the importance of developing an interdisciplinary ICU team caring for critically ill patients receiving CRRT. In the context of how integral the specific role of each team member is, it becomes clear that the bedside nurse’s role is not only to deliver hands-on patient care but also the orchestration of collaborative communication among all health-care providers for the effective provision of CRRT to critically ill patients in the ICU.
Dr. Neyra and Ms. Hauschild are with the Department of Internal Medicine; Division of Nephrology; Bone and Mineral Metabolism; University of Kentucky; Lexington, Kentucky.
An update on chronic thromboembolic pulmonary hypertension
The “fixable” form of PH that you don’t want to miss
Chronic thromboembolic pulmonary hypertension (CTEPH) is an elevation in pulmonary vascular resistance (PVR) resulting from chronic, “scarred-in” thromboembolic material partially occluding the pulmonary arteries. This vascular obstruction, over time, results in failure of the right ventricle and early mortality.
CTEPH was first characterized in an autopsy series from the Massachusetts General Hospital in 1931. On these postmortem examinations, it was noted that the affected patients had large pulmonary artery vascular obstruction, but also normal pulmonary parenchyma distal to this vascular obstruction and extensive bronchial collateral blood flow (Means J. Ann Intern Med. 1931;5:417). Although this observation set the groundwork for the theory that surgically removing the vascular obstruction to this preserved lung tissue could improve the condition of these patients, it would take until the mid-20th century until imaging and cardiac catheterization techniques allowed the recognition of the disease in real time.
CTEPH is thought to begin with an acute pulmonary embolus, but in approximately 3.4% of patients, rather than resolving over time, the thrombus will organize and incorporate into the pulmonary artery intimal layer (Simonneau G, et al. Eur Respir Rev. 2017;26:160112) A history of venous thromboembolism in a patient with persistent dyspnea should spur a screening evaluation for CTEPH; 75% of patients with CTEPH have a history of prior known acute pulmonary embolus and 56% of patients report a prior diagnosis of deep venous thrombosis. An acute pulmonary embolus will fibrinolyse early with the vast majority of the vascular obstruction resolving by the third month. Therefore, if the patient continues to report a significant exercise limitation after 3 months of therapeutic anticoagulation therapy, or has concerning physical exam signs, a workup should be pursued. The initial evaluation for CTEPH begins with a transthoracic echocardiogram (TTE) and ventilation/perfusion (V/Q) scintigraphy. A retrospective study comparing V/Q scan and multidetector CT scan revealed that V/Q scanning had a sensitivity and specificity of 97% and 95% for CTEPH, while CTPA had good specificity at 99% but only 51% sensitivity (Tunariu N, et al. J Nuc Med. 2007;48(5):680). If these are abnormal, then right-sided heart catheterization and invasive biplane digital subtraction pulmonary angiography are recommended. These studies confirm the diagnosis, grade its severity, and allow an evaluation for surgically accessible vs distal disease. Some CTEPH centers utilize additional imaging techniques, such as magnetic resonance angiography, optical resonance imaging, spectral CT scanning with iodine perfusion images, and intravascular ultrasound. These modalities and their place in the diagnostic algorithm are under investigation.
The goal of the initial evaluation process is to determine if the patient can undergo surgical pulmonary thromboendarterectomy (PTE), because in experienced hands, this procedure ensures the best long-term outcome for the patient. The first pulmonary thromboendarterectomy was performed at the University of California San Diego in 1970. Because the disease involves the intimal layer of the pulmonary artery, the surgery had to involve not just removal of the intravascular obstruction but also a pulmonary artery intimectomy. Surgical mortality rates were high in the initial experience. In 1984, a review of 85 worldwide cases reported an average mortality rate of 22%, and as high as 40% in some centers (Chitwood WR, Jr, et al. Clin Chest Med. 1984;5(3):507).
Over the ensuing years, refinements in surgical technique, the utilization of deep hypothermia and cardiac arrest during the procedure, development of new surgical instruments, and standardization of surgical selection and postoperative care have improved surgical mortality to <5% in experienced centers. Long-term outcomes of successful PTE surgery remain good, with 90% 3-year survival vs 70% for those who do not undergo surgery and are medically treated. Importantly, 90% of postoperative patients report functional class I or II symptoms at 1 year (Condliffe R, et al. Am J Reslpir Crit Care Med. 2008:177(10);1122). Because of this difference in early mortality and symptoms, PTE surgery remains the treatment of choice for CTEPH.
Despite the advances in PTE surgery, some patients are not operative candidates either due to surgically inaccessible disease or due to comorbidities. In 2001, Feinstein and colleagues described a series of 18 CTEPH cases treated with balloon pulmonary angioplasty (BPA). Promising hemodynamics effects were reported; however, the procedure had an unacceptable complication rate in which 11 patients developed reperfusion lung injury, 3 patients required mechanical ventilation, and 1 patient died. In the ensuing years, Japanese and Norwegian groups have independently developed and improved techniques for BPA. The procedure is done in a series of sessions (average four to six), 1 to 4 weeks apart, where small (2-3 mm) balloons are directed toward distal, diseased pulmonary vessels. Common complications include reperfusion injury, vessel injury, hemoptysis, and, more rarely, respiratory failure. Still, early experience suggests this procedure decreases pulmonary vascular resistance over time, improves right ventricular function, and improves patients’ symptoms (Andreassen A, et al. Heart. 2013;99(19):1415). The experience with this procedure is limited but growing in the United States, with only a handful of centers currently performing BPAs and collecting data.
Lifelong anticoagulation, oxygen, and diuretics for right-sided heart failure are recommended for patients with CTEPH. The first successful large phase III medication study for CTEPH was the CHEST-1 trial published in 2013. This was a multicenter, randomized, placebo-controlled trial of the soluble guanylate cyclase stimulator riociguat. The study enrolled 261 patients with inoperable CTEPH or persistent pulmonary hypertension after surgery. The primary end point was 6-minute walk distance at 12 weeks. The treatment group showed a 46 m improvement (P<.001). Secondary end points of pulmonary vascular resistance, NT-proBNP level, and functional class also improved. This pivotal trial led to the FDA approval of riociguat for inoperable or persistent postoperative CTEPH.
MERIT-1, a phase II, randomized placebo-controlled double trial of macitentan (an oral endothelin receptor antagonist) was recently completed. It enrolled 80 patients with inoperable CTEPH. The primary endpoint was pulmonary vascular resistance at week 16, expressed as a percentage of baseline. At week 16, the patients in the treatment arm had a PVR 73% of baseline vs 87.2% in the treatment group. This medication is not yet FDA-approved for the treatment of inoperable CTEPH (Ghofrani H, et al. Lancet Respir Med. 2017;5(10):785-794).
Pulmonary hypertension medication has been postulated as a possible way to “pretreat” patients before pulmonary thromboendarterectomy surgery, perhaps lowering preoperative pulmonary vascular resistance and surgical risk. However, there are currently no convincing data to support this practice, and medical treatment has been associated with a possible counterproductive delay in surgery. A phase II study including CTEPH patients with high PVR for preoperative treatment with riociguat vs placebo is currently enrolling to determine if “induction” treatment with medication prior to surgery reduces risk or delays definitive surgery. Occasionally, patients are found who have persistent thrombus but not pulmonary hypertension. Chronic thromboembolic disease (CTED) is a recently coined term describing patients who have chronic thromboembolism on imaging but have normal resting hemodynamics. Whether CTED represents simply unresolved clot that will never progress to CTEPH or is an early point on the continuum of disease not well-defined and a controversial topic among experts. At many centers, patients with CTED and symptoms will undergo exercise testing to look for exercise -induced pulmonary hypertension or an increase in dead space ventilation as a cause of their symptoms. A retrospective series of carefully chosen CTED patients who underwent PTE surgery reported improvements in symptoms and overall quality of life, without increased complications (Taboada D, et al. Eur Respir J. 2014 44(6):1635). The operation carries risk, however, and further work into the epidemiology and prognosis of CTED is required before operative intervention can be recommended.
In conclusion, CTEPH is a disease that rarely occurs after an acute PE but when undiagnosed and untreated portends a poor prognosis. The definitive treatment for this disease is surgical PTE, but to achieve the best outcomes, this procedure needs to be performed at expert centers with multidisciplinary team experience. Patients who are poor operative candidates or with surgically inaccessible disease may be considered for balloon pulmonary angioplasty. For patients without more curative options, medication improves exercise tolerance. The field of CTEPH has been rapidly expanding over the last decade, leading to better patient outcomes and more treatment options.
Dr. Bartolome is Associate Professor, Pulmonary and Critical Care Medicine; Director, CTEPH Program; and Associate Director, PH Program; UT Southwestern Medical Center, Dallas, Texas.
The “fixable” form of PH that you don’t want to miss
The “fixable” form of PH that you don’t want to miss
Chronic thromboembolic pulmonary hypertension (CTEPH) is an elevation in pulmonary vascular resistance (PVR) resulting from chronic, “scarred-in” thromboembolic material partially occluding the pulmonary arteries. This vascular obstruction, over time, results in failure of the right ventricle and early mortality.
CTEPH was first characterized in an autopsy series from the Massachusetts General Hospital in 1931. On these postmortem examinations, it was noted that the affected patients had large pulmonary artery vascular obstruction, but also normal pulmonary parenchyma distal to this vascular obstruction and extensive bronchial collateral blood flow (Means J. Ann Intern Med. 1931;5:417). Although this observation set the groundwork for the theory that surgically removing the vascular obstruction to this preserved lung tissue could improve the condition of these patients, it would take until the mid-20th century until imaging and cardiac catheterization techniques allowed the recognition of the disease in real time.
CTEPH is thought to begin with an acute pulmonary embolus, but in approximately 3.4% of patients, rather than resolving over time, the thrombus will organize and incorporate into the pulmonary artery intimal layer (Simonneau G, et al. Eur Respir Rev. 2017;26:160112) A history of venous thromboembolism in a patient with persistent dyspnea should spur a screening evaluation for CTEPH; 75% of patients with CTEPH have a history of prior known acute pulmonary embolus and 56% of patients report a prior diagnosis of deep venous thrombosis. An acute pulmonary embolus will fibrinolyse early with the vast majority of the vascular obstruction resolving by the third month. Therefore, if the patient continues to report a significant exercise limitation after 3 months of therapeutic anticoagulation therapy, or has concerning physical exam signs, a workup should be pursued. The initial evaluation for CTEPH begins with a transthoracic echocardiogram (TTE) and ventilation/perfusion (V/Q) scintigraphy. A retrospective study comparing V/Q scan and multidetector CT scan revealed that V/Q scanning had a sensitivity and specificity of 97% and 95% for CTEPH, while CTPA had good specificity at 99% but only 51% sensitivity (Tunariu N, et al. J Nuc Med. 2007;48(5):680). If these are abnormal, then right-sided heart catheterization and invasive biplane digital subtraction pulmonary angiography are recommended. These studies confirm the diagnosis, grade its severity, and allow an evaluation for surgically accessible vs distal disease. Some CTEPH centers utilize additional imaging techniques, such as magnetic resonance angiography, optical resonance imaging, spectral CT scanning with iodine perfusion images, and intravascular ultrasound. These modalities and their place in the diagnostic algorithm are under investigation.
The goal of the initial evaluation process is to determine if the patient can undergo surgical pulmonary thromboendarterectomy (PTE), because in experienced hands, this procedure ensures the best long-term outcome for the patient. The first pulmonary thromboendarterectomy was performed at the University of California San Diego in 1970. Because the disease involves the intimal layer of the pulmonary artery, the surgery had to involve not just removal of the intravascular obstruction but also a pulmonary artery intimectomy. Surgical mortality rates were high in the initial experience. In 1984, a review of 85 worldwide cases reported an average mortality rate of 22%, and as high as 40% in some centers (Chitwood WR, Jr, et al. Clin Chest Med. 1984;5(3):507).
Over the ensuing years, refinements in surgical technique, the utilization of deep hypothermia and cardiac arrest during the procedure, development of new surgical instruments, and standardization of surgical selection and postoperative care have improved surgical mortality to <5% in experienced centers. Long-term outcomes of successful PTE surgery remain good, with 90% 3-year survival vs 70% for those who do not undergo surgery and are medically treated. Importantly, 90% of postoperative patients report functional class I or II symptoms at 1 year (Condliffe R, et al. Am J Reslpir Crit Care Med. 2008:177(10);1122). Because of this difference in early mortality and symptoms, PTE surgery remains the treatment of choice for CTEPH.
Despite the advances in PTE surgery, some patients are not operative candidates either due to surgically inaccessible disease or due to comorbidities. In 2001, Feinstein and colleagues described a series of 18 CTEPH cases treated with balloon pulmonary angioplasty (BPA). Promising hemodynamics effects were reported; however, the procedure had an unacceptable complication rate in which 11 patients developed reperfusion lung injury, 3 patients required mechanical ventilation, and 1 patient died. In the ensuing years, Japanese and Norwegian groups have independently developed and improved techniques for BPA. The procedure is done in a series of sessions (average four to six), 1 to 4 weeks apart, where small (2-3 mm) balloons are directed toward distal, diseased pulmonary vessels. Common complications include reperfusion injury, vessel injury, hemoptysis, and, more rarely, respiratory failure. Still, early experience suggests this procedure decreases pulmonary vascular resistance over time, improves right ventricular function, and improves patients’ symptoms (Andreassen A, et al. Heart. 2013;99(19):1415). The experience with this procedure is limited but growing in the United States, with only a handful of centers currently performing BPAs and collecting data.
Lifelong anticoagulation, oxygen, and diuretics for right-sided heart failure are recommended for patients with CTEPH. The first successful large phase III medication study for CTEPH was the CHEST-1 trial published in 2013. This was a multicenter, randomized, placebo-controlled trial of the soluble guanylate cyclase stimulator riociguat. The study enrolled 261 patients with inoperable CTEPH or persistent pulmonary hypertension after surgery. The primary end point was 6-minute walk distance at 12 weeks. The treatment group showed a 46 m improvement (P<.001). Secondary end points of pulmonary vascular resistance, NT-proBNP level, and functional class also improved. This pivotal trial led to the FDA approval of riociguat for inoperable or persistent postoperative CTEPH.
MERIT-1, a phase II, randomized placebo-controlled double trial of macitentan (an oral endothelin receptor antagonist) was recently completed. It enrolled 80 patients with inoperable CTEPH. The primary endpoint was pulmonary vascular resistance at week 16, expressed as a percentage of baseline. At week 16, the patients in the treatment arm had a PVR 73% of baseline vs 87.2% in the treatment group. This medication is not yet FDA-approved for the treatment of inoperable CTEPH (Ghofrani H, et al. Lancet Respir Med. 2017;5(10):785-794).
Pulmonary hypertension medication has been postulated as a possible way to “pretreat” patients before pulmonary thromboendarterectomy surgery, perhaps lowering preoperative pulmonary vascular resistance and surgical risk. However, there are currently no convincing data to support this practice, and medical treatment has been associated with a possible counterproductive delay in surgery. A phase II study including CTEPH patients with high PVR for preoperative treatment with riociguat vs placebo is currently enrolling to determine if “induction” treatment with medication prior to surgery reduces risk or delays definitive surgery. Occasionally, patients are found who have persistent thrombus but not pulmonary hypertension. Chronic thromboembolic disease (CTED) is a recently coined term describing patients who have chronic thromboembolism on imaging but have normal resting hemodynamics. Whether CTED represents simply unresolved clot that will never progress to CTEPH or is an early point on the continuum of disease not well-defined and a controversial topic among experts. At many centers, patients with CTED and symptoms will undergo exercise testing to look for exercise -induced pulmonary hypertension or an increase in dead space ventilation as a cause of their symptoms. A retrospective series of carefully chosen CTED patients who underwent PTE surgery reported improvements in symptoms and overall quality of life, without increased complications (Taboada D, et al. Eur Respir J. 2014 44(6):1635). The operation carries risk, however, and further work into the epidemiology and prognosis of CTED is required before operative intervention can be recommended.
In conclusion, CTEPH is a disease that rarely occurs after an acute PE but when undiagnosed and untreated portends a poor prognosis. The definitive treatment for this disease is surgical PTE, but to achieve the best outcomes, this procedure needs to be performed at expert centers with multidisciplinary team experience. Patients who are poor operative candidates or with surgically inaccessible disease may be considered for balloon pulmonary angioplasty. For patients without more curative options, medication improves exercise tolerance. The field of CTEPH has been rapidly expanding over the last decade, leading to better patient outcomes and more treatment options.
Dr. Bartolome is Associate Professor, Pulmonary and Critical Care Medicine; Director, CTEPH Program; and Associate Director, PH Program; UT Southwestern Medical Center, Dallas, Texas.
Chronic thromboembolic pulmonary hypertension (CTEPH) is an elevation in pulmonary vascular resistance (PVR) resulting from chronic, “scarred-in” thromboembolic material partially occluding the pulmonary arteries. This vascular obstruction, over time, results in failure of the right ventricle and early mortality.
CTEPH was first characterized in an autopsy series from the Massachusetts General Hospital in 1931. On these postmortem examinations, it was noted that the affected patients had large pulmonary artery vascular obstruction, but also normal pulmonary parenchyma distal to this vascular obstruction and extensive bronchial collateral blood flow (Means J. Ann Intern Med. 1931;5:417). Although this observation set the groundwork for the theory that surgically removing the vascular obstruction to this preserved lung tissue could improve the condition of these patients, it would take until the mid-20th century until imaging and cardiac catheterization techniques allowed the recognition of the disease in real time.
CTEPH is thought to begin with an acute pulmonary embolus, but in approximately 3.4% of patients, rather than resolving over time, the thrombus will organize and incorporate into the pulmonary artery intimal layer (Simonneau G, et al. Eur Respir Rev. 2017;26:160112) A history of venous thromboembolism in a patient with persistent dyspnea should spur a screening evaluation for CTEPH; 75% of patients with CTEPH have a history of prior known acute pulmonary embolus and 56% of patients report a prior diagnosis of deep venous thrombosis. An acute pulmonary embolus will fibrinolyse early with the vast majority of the vascular obstruction resolving by the third month. Therefore, if the patient continues to report a significant exercise limitation after 3 months of therapeutic anticoagulation therapy, or has concerning physical exam signs, a workup should be pursued. The initial evaluation for CTEPH begins with a transthoracic echocardiogram (TTE) and ventilation/perfusion (V/Q) scintigraphy. A retrospective study comparing V/Q scan and multidetector CT scan revealed that V/Q scanning had a sensitivity and specificity of 97% and 95% for CTEPH, while CTPA had good specificity at 99% but only 51% sensitivity (Tunariu N, et al. J Nuc Med. 2007;48(5):680). If these are abnormal, then right-sided heart catheterization and invasive biplane digital subtraction pulmonary angiography are recommended. These studies confirm the diagnosis, grade its severity, and allow an evaluation for surgically accessible vs distal disease. Some CTEPH centers utilize additional imaging techniques, such as magnetic resonance angiography, optical resonance imaging, spectral CT scanning with iodine perfusion images, and intravascular ultrasound. These modalities and their place in the diagnostic algorithm are under investigation.
The goal of the initial evaluation process is to determine if the patient can undergo surgical pulmonary thromboendarterectomy (PTE), because in experienced hands, this procedure ensures the best long-term outcome for the patient. The first pulmonary thromboendarterectomy was performed at the University of California San Diego in 1970. Because the disease involves the intimal layer of the pulmonary artery, the surgery had to involve not just removal of the intravascular obstruction but also a pulmonary artery intimectomy. Surgical mortality rates were high in the initial experience. In 1984, a review of 85 worldwide cases reported an average mortality rate of 22%, and as high as 40% in some centers (Chitwood WR, Jr, et al. Clin Chest Med. 1984;5(3):507).
Over the ensuing years, refinements in surgical technique, the utilization of deep hypothermia and cardiac arrest during the procedure, development of new surgical instruments, and standardization of surgical selection and postoperative care have improved surgical mortality to <5% in experienced centers. Long-term outcomes of successful PTE surgery remain good, with 90% 3-year survival vs 70% for those who do not undergo surgery and are medically treated. Importantly, 90% of postoperative patients report functional class I or II symptoms at 1 year (Condliffe R, et al. Am J Reslpir Crit Care Med. 2008:177(10);1122). Because of this difference in early mortality and symptoms, PTE surgery remains the treatment of choice for CTEPH.
Despite the advances in PTE surgery, some patients are not operative candidates either due to surgically inaccessible disease or due to comorbidities. In 2001, Feinstein and colleagues described a series of 18 CTEPH cases treated with balloon pulmonary angioplasty (BPA). Promising hemodynamics effects were reported; however, the procedure had an unacceptable complication rate in which 11 patients developed reperfusion lung injury, 3 patients required mechanical ventilation, and 1 patient died. In the ensuing years, Japanese and Norwegian groups have independently developed and improved techniques for BPA. The procedure is done in a series of sessions (average four to six), 1 to 4 weeks apart, where small (2-3 mm) balloons are directed toward distal, diseased pulmonary vessels. Common complications include reperfusion injury, vessel injury, hemoptysis, and, more rarely, respiratory failure. Still, early experience suggests this procedure decreases pulmonary vascular resistance over time, improves right ventricular function, and improves patients’ symptoms (Andreassen A, et al. Heart. 2013;99(19):1415). The experience with this procedure is limited but growing in the United States, with only a handful of centers currently performing BPAs and collecting data.
Lifelong anticoagulation, oxygen, and diuretics for right-sided heart failure are recommended for patients with CTEPH. The first successful large phase III medication study for CTEPH was the CHEST-1 trial published in 2013. This was a multicenter, randomized, placebo-controlled trial of the soluble guanylate cyclase stimulator riociguat. The study enrolled 261 patients with inoperable CTEPH or persistent pulmonary hypertension after surgery. The primary end point was 6-minute walk distance at 12 weeks. The treatment group showed a 46 m improvement (P<.001). Secondary end points of pulmonary vascular resistance, NT-proBNP level, and functional class also improved. This pivotal trial led to the FDA approval of riociguat for inoperable or persistent postoperative CTEPH.
MERIT-1, a phase II, randomized placebo-controlled double trial of macitentan (an oral endothelin receptor antagonist) was recently completed. It enrolled 80 patients with inoperable CTEPH. The primary endpoint was pulmonary vascular resistance at week 16, expressed as a percentage of baseline. At week 16, the patients in the treatment arm had a PVR 73% of baseline vs 87.2% in the treatment group. This medication is not yet FDA-approved for the treatment of inoperable CTEPH (Ghofrani H, et al. Lancet Respir Med. 2017;5(10):785-794).
Pulmonary hypertension medication has been postulated as a possible way to “pretreat” patients before pulmonary thromboendarterectomy surgery, perhaps lowering preoperative pulmonary vascular resistance and surgical risk. However, there are currently no convincing data to support this practice, and medical treatment has been associated with a possible counterproductive delay in surgery. A phase II study including CTEPH patients with high PVR for preoperative treatment with riociguat vs placebo is currently enrolling to determine if “induction” treatment with medication prior to surgery reduces risk or delays definitive surgery. Occasionally, patients are found who have persistent thrombus but not pulmonary hypertension. Chronic thromboembolic disease (CTED) is a recently coined term describing patients who have chronic thromboembolism on imaging but have normal resting hemodynamics. Whether CTED represents simply unresolved clot that will never progress to CTEPH or is an early point on the continuum of disease not well-defined and a controversial topic among experts. At many centers, patients with CTED and symptoms will undergo exercise testing to look for exercise -induced pulmonary hypertension or an increase in dead space ventilation as a cause of their symptoms. A retrospective series of carefully chosen CTED patients who underwent PTE surgery reported improvements in symptoms and overall quality of life, without increased complications (Taboada D, et al. Eur Respir J. 2014 44(6):1635). The operation carries risk, however, and further work into the epidemiology and prognosis of CTED is required before operative intervention can be recommended.
In conclusion, CTEPH is a disease that rarely occurs after an acute PE but when undiagnosed and untreated portends a poor prognosis. The definitive treatment for this disease is surgical PTE, but to achieve the best outcomes, this procedure needs to be performed at expert centers with multidisciplinary team experience. Patients who are poor operative candidates or with surgically inaccessible disease may be considered for balloon pulmonary angioplasty. For patients without more curative options, medication improves exercise tolerance. The field of CTEPH has been rapidly expanding over the last decade, leading to better patient outcomes and more treatment options.
Dr. Bartolome is Associate Professor, Pulmonary and Critical Care Medicine; Director, CTEPH Program; and Associate Director, PH Program; UT Southwestern Medical Center, Dallas, Texas.