User login
FDA approves generic Advair Diskus
The Food and Drug Administration has approved a generic version of the Advair Diskus, a complex device-drug combination containing fluticasone propionate and salmeterol inhalation powder.
The generic device will be available in three strengths: fluticasone propionate 100 mcg/ salmeterol 50 mcg, fluticasone propionate 250 mcg/ salmeterol 50 mcg and fluticasone propionate 500 mcg/ salmeterol 50 mcg, according to the FDA announcement. It will be marketed by Mylan as Wixela Inhub and will launch in late February, according to a statement from Mylan.
Advair Diskus is among the most commonly used treatments for asthma and for chronic obstructive pulmonary disease (COPD), so it’s hoped this approval will increase access to the therapy, FDA officials said in a statement.
This approval is part of the FDA’s “longstanding commitment to advance access to lower cost, high quality generic alternatives,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a statement. “People living with asthma and COPD know too well the critical importance of having access to the treatment they need to feel better. Today’s approval will bring more competition to the market which will ultimately benefit the patients who rely on this drug.”
Wixela Inhub is indicated for twice-daily treatment of asthma in patients aged 4 years and older who are not adequately controlled by long-term asthma control treatments or whose disease warrants treatment with a combination of inhaled corticosteroids and long-acting beta agonists. It also is indicated for maintenance of COPD and reduction of COPD exacerbations.
The Food and Drug Administration has approved a generic version of the Advair Diskus, a complex device-drug combination containing fluticasone propionate and salmeterol inhalation powder.
The generic device will be available in three strengths: fluticasone propionate 100 mcg/ salmeterol 50 mcg, fluticasone propionate 250 mcg/ salmeterol 50 mcg and fluticasone propionate 500 mcg/ salmeterol 50 mcg, according to the FDA announcement. It will be marketed by Mylan as Wixela Inhub and will launch in late February, according to a statement from Mylan.
Advair Diskus is among the most commonly used treatments for asthma and for chronic obstructive pulmonary disease (COPD), so it’s hoped this approval will increase access to the therapy, FDA officials said in a statement.
This approval is part of the FDA’s “longstanding commitment to advance access to lower cost, high quality generic alternatives,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a statement. “People living with asthma and COPD know too well the critical importance of having access to the treatment they need to feel better. Today’s approval will bring more competition to the market which will ultimately benefit the patients who rely on this drug.”
Wixela Inhub is indicated for twice-daily treatment of asthma in patients aged 4 years and older who are not adequately controlled by long-term asthma control treatments or whose disease warrants treatment with a combination of inhaled corticosteroids and long-acting beta agonists. It also is indicated for maintenance of COPD and reduction of COPD exacerbations.
The Food and Drug Administration has approved a generic version of the Advair Diskus, a complex device-drug combination containing fluticasone propionate and salmeterol inhalation powder.
The generic device will be available in three strengths: fluticasone propionate 100 mcg/ salmeterol 50 mcg, fluticasone propionate 250 mcg/ salmeterol 50 mcg and fluticasone propionate 500 mcg/ salmeterol 50 mcg, according to the FDA announcement. It will be marketed by Mylan as Wixela Inhub and will launch in late February, according to a statement from Mylan.
Advair Diskus is among the most commonly used treatments for asthma and for chronic obstructive pulmonary disease (COPD), so it’s hoped this approval will increase access to the therapy, FDA officials said in a statement.
This approval is part of the FDA’s “longstanding commitment to advance access to lower cost, high quality generic alternatives,” Janet Woodcock, MD, director of the FDA’s Center for Drug Evaluation and Research, said in a statement. “People living with asthma and COPD know too well the critical importance of having access to the treatment they need to feel better. Today’s approval will bring more competition to the market which will ultimately benefit the patients who rely on this drug.”
Wixela Inhub is indicated for twice-daily treatment of asthma in patients aged 4 years and older who are not adequately controlled by long-term asthma control treatments or whose disease warrants treatment with a combination of inhaled corticosteroids and long-acting beta agonists. It also is indicated for maintenance of COPD and reduction of COPD exacerbations.
AHA report highlights CVD burden, declines in smoking, sleep importance
Almost half of U.S. adults now have some form of cardiovascular disease, according to the latest annual statistical update from the American Heart Association.
The prevalence is driven in part by the recently changed definition of hypertension, from 140/90 to 130/80 mm Hg, said authors of the American Heart Association Heart Disease and Stroke Statistics–2019 Update.
Cardiovascular disease (CVD) deaths are up, though smoking rates continue to decline, and adults are getting more exercise (Circulation. 2019;139. doi: 10.1161/CIR.0000000000000659).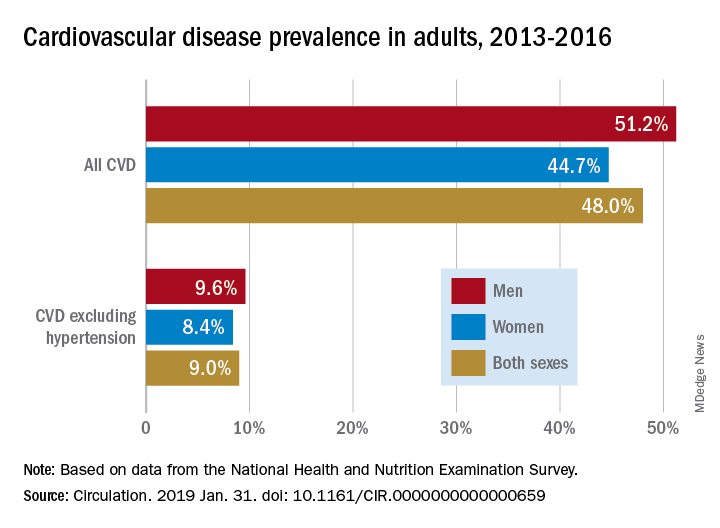
The update includes a new section on sleep and cardiovascular health, an enhanced focus on social determinants of health, and further evidence-based approaches to behavior change, according to the update’s authors, led by chair Emelia J. Benjamin, MD, professor of medicine and epidemiology at Boston University, and vice chair Paul Muntner, PhD, professor of epidemiology at the University of Alabama, Birmingham.
High blood pressure is an “overwhelming presence” that drives heart disease and stroke and can’t be dismissed in the fight against cardiovascular disease, AHA President Ivor J. Benjamin, MD, said in a statement. “Eliminating high blood pressure could have a larger impact on CVD deaths than the elimination of all other risk factors among women, and all except smoking among men.”
Using data from 2013 to 2016, 46% of adults in the United States had hypertension, and in 2016 there were 82,735 deaths attributable primarily to high blood pressure, according to the update.
Total direct costs of hypertension could approach $221 billion by 2035, according to projections in the report.
After decades of decline, U.S. cardiovascular disease deaths increased to 840,678 in 2016, up from 836,546 in 2015, the report says.
Smoking rate declines represent some of the most significant improvements outlined in the report, according to an AHA news release.
Ninety-four percent of adolescents were nonsmokers in the 2015-2016 period, which is up from 76% in 1999-2000, according to the report. The proportion of adult nonsmokers increased to 79% in 2015-2016, up from 73% in 1999-2000.
The new chapter on the importance of sleep cites data from the Centers for Disease Control and Prevention that only 65.2% of Americans have a healthy sleep duration (at least 7 hours), with even lower rates among non-Hispanic blacks, native Hawaiians and Pacific Islanders, and multiracial non-Hispanic individuals.
Short sleep duration is associated with a higher risk of all-cause mortality, total CVD, and coronary heart disease, according to a meta-analysis cited in the report. Long sleep duration, defined as greater than 8 hours, also was associated with higher risk of all-cause mortality, total CVD, coronary heart disease, and stroke.
Members of the statistical update writing group reported disclosures related to the American Heart Association, National Institutes of Health, Amgen, Sanofi, Roche, Abbott, Biogen, Medtronic, and others.
SOURCE: Benjamin EJ et al. Circulation. 2019 Jan 31.
The latest statistics on heart disease and stroke include some metrics that indicate progress, and others that suggest opportunities for improvement.
Tobacco use continues to decline; however, among high school students, e-cigarette use is up to 11.3%, which is concerning.
One bright spot is that the proportion of inactive adults has dropped to 30% in 2016, down from 40% in 2007. Despite that improvement, however, the prevalence of obesity increased significantly over the decade, to the point where nearly 40% of adults are obese and 7.7% are severely obese.
Although 48% of U.S. adults now have cardiovascular disease, according to this latest update, the number drops to just 9% when hypertension is excluded. Even so, 9% represents more than 24.3 million Americans who have coronary artery disease, stroke, or heart failure.
The cost of cardiovascular disease is astronomical, exceeding $351 billion in 2014-1205, with costs projected to increase sharply for older adults over the next few decades.
Starting in 2020, the AHA will begin charting progress in CVD using a metric called health-adjusted life expectancy (HALE), which relies on morbidity and mortality patterns to reflect the number of years a person can expect to live. Patients and the general public may find this metric more understandable than statistics about death rates and cardiovascular risk factors.
Mariell Jessup, MD, is chief science and medical officer for the American Heart Association. Her view on the latest statistical update was derived from a commentary that accompanied the update.
The latest statistics on heart disease and stroke include some metrics that indicate progress, and others that suggest opportunities for improvement.
Tobacco use continues to decline; however, among high school students, e-cigarette use is up to 11.3%, which is concerning.
One bright spot is that the proportion of inactive adults has dropped to 30% in 2016, down from 40% in 2007. Despite that improvement, however, the prevalence of obesity increased significantly over the decade, to the point where nearly 40% of adults are obese and 7.7% are severely obese.
Although 48% of U.S. adults now have cardiovascular disease, according to this latest update, the number drops to just 9% when hypertension is excluded. Even so, 9% represents more than 24.3 million Americans who have coronary artery disease, stroke, or heart failure.
The cost of cardiovascular disease is astronomical, exceeding $351 billion in 2014-1205, with costs projected to increase sharply for older adults over the next few decades.
Starting in 2020, the AHA will begin charting progress in CVD using a metric called health-adjusted life expectancy (HALE), which relies on morbidity and mortality patterns to reflect the number of years a person can expect to live. Patients and the general public may find this metric more understandable than statistics about death rates and cardiovascular risk factors.
Mariell Jessup, MD, is chief science and medical officer for the American Heart Association. Her view on the latest statistical update was derived from a commentary that accompanied the update.
The latest statistics on heart disease and stroke include some metrics that indicate progress, and others that suggest opportunities for improvement.
Tobacco use continues to decline; however, among high school students, e-cigarette use is up to 11.3%, which is concerning.
One bright spot is that the proportion of inactive adults has dropped to 30% in 2016, down from 40% in 2007. Despite that improvement, however, the prevalence of obesity increased significantly over the decade, to the point where nearly 40% of adults are obese and 7.7% are severely obese.
Although 48% of U.S. adults now have cardiovascular disease, according to this latest update, the number drops to just 9% when hypertension is excluded. Even so, 9% represents more than 24.3 million Americans who have coronary artery disease, stroke, or heart failure.
The cost of cardiovascular disease is astronomical, exceeding $351 billion in 2014-1205, with costs projected to increase sharply for older adults over the next few decades.
Starting in 2020, the AHA will begin charting progress in CVD using a metric called health-adjusted life expectancy (HALE), which relies on morbidity and mortality patterns to reflect the number of years a person can expect to live. Patients and the general public may find this metric more understandable than statistics about death rates and cardiovascular risk factors.
Mariell Jessup, MD, is chief science and medical officer for the American Heart Association. Her view on the latest statistical update was derived from a commentary that accompanied the update.
Almost half of U.S. adults now have some form of cardiovascular disease, according to the latest annual statistical update from the American Heart Association.
The prevalence is driven in part by the recently changed definition of hypertension, from 140/90 to 130/80 mm Hg, said authors of the American Heart Association Heart Disease and Stroke Statistics–2019 Update.
Cardiovascular disease (CVD) deaths are up, though smoking rates continue to decline, and adults are getting more exercise (Circulation. 2019;139. doi: 10.1161/CIR.0000000000000659).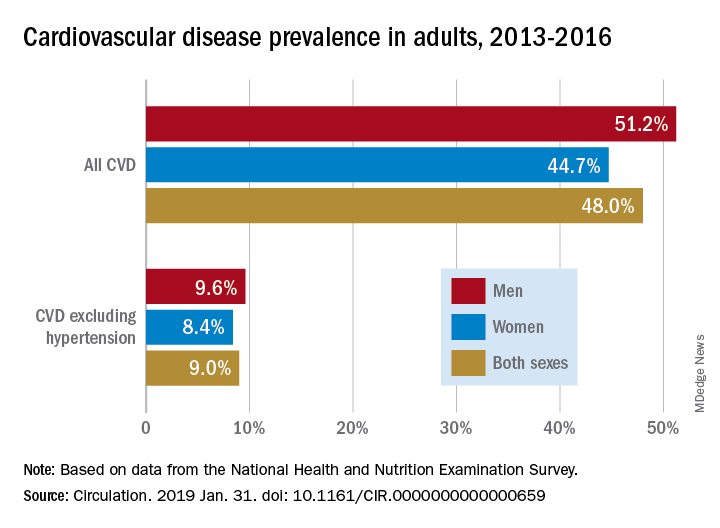
The update includes a new section on sleep and cardiovascular health, an enhanced focus on social determinants of health, and further evidence-based approaches to behavior change, according to the update’s authors, led by chair Emelia J. Benjamin, MD, professor of medicine and epidemiology at Boston University, and vice chair Paul Muntner, PhD, professor of epidemiology at the University of Alabama, Birmingham.
High blood pressure is an “overwhelming presence” that drives heart disease and stroke and can’t be dismissed in the fight against cardiovascular disease, AHA President Ivor J. Benjamin, MD, said in a statement. “Eliminating high blood pressure could have a larger impact on CVD deaths than the elimination of all other risk factors among women, and all except smoking among men.”
Using data from 2013 to 2016, 46% of adults in the United States had hypertension, and in 2016 there were 82,735 deaths attributable primarily to high blood pressure, according to the update.
Total direct costs of hypertension could approach $221 billion by 2035, according to projections in the report.
After decades of decline, U.S. cardiovascular disease deaths increased to 840,678 in 2016, up from 836,546 in 2015, the report says.
Smoking rate declines represent some of the most significant improvements outlined in the report, according to an AHA news release.
Ninety-four percent of adolescents were nonsmokers in the 2015-2016 period, which is up from 76% in 1999-2000, according to the report. The proportion of adult nonsmokers increased to 79% in 2015-2016, up from 73% in 1999-2000.
The new chapter on the importance of sleep cites data from the Centers for Disease Control and Prevention that only 65.2% of Americans have a healthy sleep duration (at least 7 hours), with even lower rates among non-Hispanic blacks, native Hawaiians and Pacific Islanders, and multiracial non-Hispanic individuals.
Short sleep duration is associated with a higher risk of all-cause mortality, total CVD, and coronary heart disease, according to a meta-analysis cited in the report. Long sleep duration, defined as greater than 8 hours, also was associated with higher risk of all-cause mortality, total CVD, coronary heart disease, and stroke.
Members of the statistical update writing group reported disclosures related to the American Heart Association, National Institutes of Health, Amgen, Sanofi, Roche, Abbott, Biogen, Medtronic, and others.
SOURCE: Benjamin EJ et al. Circulation. 2019 Jan 31.
Almost half of U.S. adults now have some form of cardiovascular disease, according to the latest annual statistical update from the American Heart Association.
The prevalence is driven in part by the recently changed definition of hypertension, from 140/90 to 130/80 mm Hg, said authors of the American Heart Association Heart Disease and Stroke Statistics–2019 Update.
Cardiovascular disease (CVD) deaths are up, though smoking rates continue to decline, and adults are getting more exercise (Circulation. 2019;139. doi: 10.1161/CIR.0000000000000659).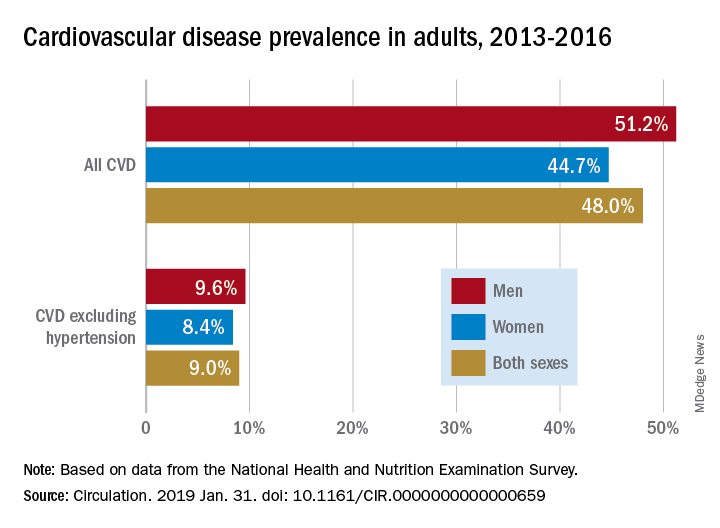
The update includes a new section on sleep and cardiovascular health, an enhanced focus on social determinants of health, and further evidence-based approaches to behavior change, according to the update’s authors, led by chair Emelia J. Benjamin, MD, professor of medicine and epidemiology at Boston University, and vice chair Paul Muntner, PhD, professor of epidemiology at the University of Alabama, Birmingham.
High blood pressure is an “overwhelming presence” that drives heart disease and stroke and can’t be dismissed in the fight against cardiovascular disease, AHA President Ivor J. Benjamin, MD, said in a statement. “Eliminating high blood pressure could have a larger impact on CVD deaths than the elimination of all other risk factors among women, and all except smoking among men.”
Using data from 2013 to 2016, 46% of adults in the United States had hypertension, and in 2016 there were 82,735 deaths attributable primarily to high blood pressure, according to the update.
Total direct costs of hypertension could approach $221 billion by 2035, according to projections in the report.
After decades of decline, U.S. cardiovascular disease deaths increased to 840,678 in 2016, up from 836,546 in 2015, the report says.
Smoking rate declines represent some of the most significant improvements outlined in the report, according to an AHA news release.
Ninety-four percent of adolescents were nonsmokers in the 2015-2016 period, which is up from 76% in 1999-2000, according to the report. The proportion of adult nonsmokers increased to 79% in 2015-2016, up from 73% in 1999-2000.
The new chapter on the importance of sleep cites data from the Centers for Disease Control and Prevention that only 65.2% of Americans have a healthy sleep duration (at least 7 hours), with even lower rates among non-Hispanic blacks, native Hawaiians and Pacific Islanders, and multiracial non-Hispanic individuals.
Short sleep duration is associated with a higher risk of all-cause mortality, total CVD, and coronary heart disease, according to a meta-analysis cited in the report. Long sleep duration, defined as greater than 8 hours, also was associated with higher risk of all-cause mortality, total CVD, coronary heart disease, and stroke.
Members of the statistical update writing group reported disclosures related to the American Heart Association, National Institutes of Health, Amgen, Sanofi, Roche, Abbott, Biogen, Medtronic, and others.
SOURCE: Benjamin EJ et al. Circulation. 2019 Jan 31.
FROM CIRCULATION
Flu activity ticks up for second week in a row
Influenza activity increased for a second straight week after a 2-week drop and by one measure has topped the high reached in late December, according to the Centers for Disease Control and Prevention.
For the week ending Jan. 26, 2019, there were 16 states at level 10 on the CDC’s 1-10 scale of influenza-like illness (ILI) activity, compared with 12 states during the week ending Dec. 29. With another seven states at levels 8 and 9, that makes 23 in the high range for the week ending Jan. 26, again putting it above the 19 reported for Dec. 29, the CDC’s influenza division reported Feb. 1.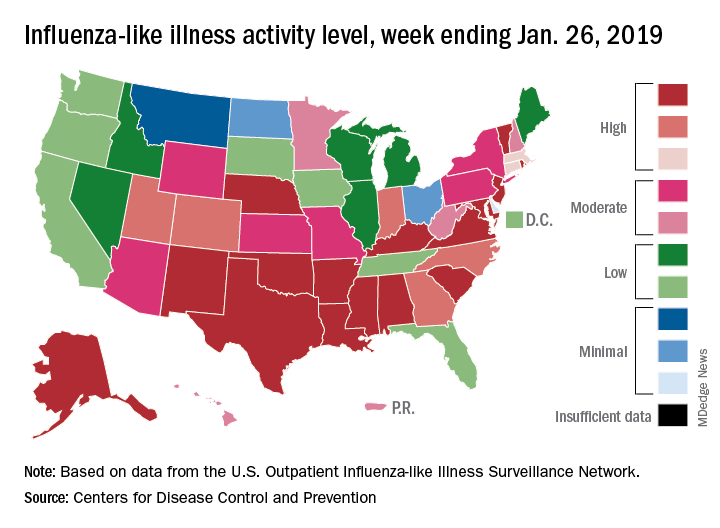
By another measure, however, that December peak in activity remains the seasonal high. The proportion of outpatient visits for ILI that week was 4.0%, compared with the 3.8% reported for Jan. 26. That’s up from 3.3% the week before and 3.1% the week before that, which in turn was the second week of a 2-week decline in activity in early January, CDC data show.
Two flu-related pediatric deaths were reported during the week ending Jan. 26, but both occurred the previous week. For the 2018-2019 flu season so far, a total of 24 pediatric flu deaths have been reported, the CDC said. At the same point in the 2017-2018 flu season, there had been 84 such deaths, according to the CDC’s Influenza-Associated Pediatric Mortality Surveillance System.
There were 143 overall flu-related deaths during the week of Jan. 19, which is the most recent week available. That is down from 189 the week before, but the Jan. 19 reporting is only 75% complete, data from the National Center for Health Statistics show.
Influenza activity increased for a second straight week after a 2-week drop and by one measure has topped the high reached in late December, according to the Centers for Disease Control and Prevention.
For the week ending Jan. 26, 2019, there were 16 states at level 10 on the CDC’s 1-10 scale of influenza-like illness (ILI) activity, compared with 12 states during the week ending Dec. 29. With another seven states at levels 8 and 9, that makes 23 in the high range for the week ending Jan. 26, again putting it above the 19 reported for Dec. 29, the CDC’s influenza division reported Feb. 1.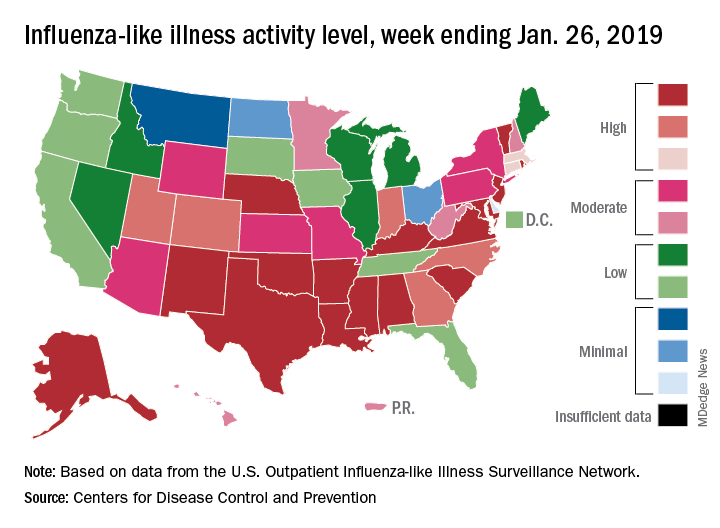
By another measure, however, that December peak in activity remains the seasonal high. The proportion of outpatient visits for ILI that week was 4.0%, compared with the 3.8% reported for Jan. 26. That’s up from 3.3% the week before and 3.1% the week before that, which in turn was the second week of a 2-week decline in activity in early January, CDC data show.
Two flu-related pediatric deaths were reported during the week ending Jan. 26, but both occurred the previous week. For the 2018-2019 flu season so far, a total of 24 pediatric flu deaths have been reported, the CDC said. At the same point in the 2017-2018 flu season, there had been 84 such deaths, according to the CDC’s Influenza-Associated Pediatric Mortality Surveillance System.
There were 143 overall flu-related deaths during the week of Jan. 19, which is the most recent week available. That is down from 189 the week before, but the Jan. 19 reporting is only 75% complete, data from the National Center for Health Statistics show.
Influenza activity increased for a second straight week after a 2-week drop and by one measure has topped the high reached in late December, according to the Centers for Disease Control and Prevention.
For the week ending Jan. 26, 2019, there were 16 states at level 10 on the CDC’s 1-10 scale of influenza-like illness (ILI) activity, compared with 12 states during the week ending Dec. 29. With another seven states at levels 8 and 9, that makes 23 in the high range for the week ending Jan. 26, again putting it above the 19 reported for Dec. 29, the CDC’s influenza division reported Feb. 1.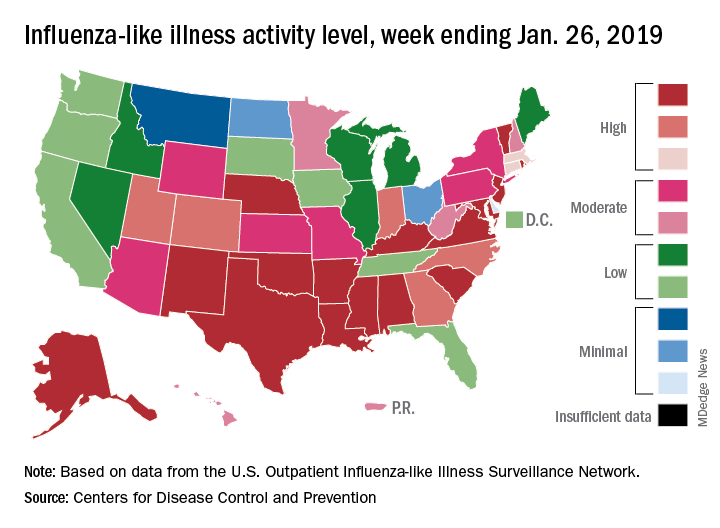
By another measure, however, that December peak in activity remains the seasonal high. The proportion of outpatient visits for ILI that week was 4.0%, compared with the 3.8% reported for Jan. 26. That’s up from 3.3% the week before and 3.1% the week before that, which in turn was the second week of a 2-week decline in activity in early January, CDC data show.
Two flu-related pediatric deaths were reported during the week ending Jan. 26, but both occurred the previous week. For the 2018-2019 flu season so far, a total of 24 pediatric flu deaths have been reported, the CDC said. At the same point in the 2017-2018 flu season, there had been 84 such deaths, according to the CDC’s Influenza-Associated Pediatric Mortality Surveillance System.
There were 143 overall flu-related deaths during the week of Jan. 19, which is the most recent week available. That is down from 189 the week before, but the Jan. 19 reporting is only 75% complete, data from the National Center for Health Statistics show.
Outcomes could improve with Oncology Care Model treatment plans
Treatment plans derived under the Oncology Care Model (OCM) improved performance on some quality measures and patient-reported outcomes, according to a study performed at three cancer centers.
Physicians and care teams at the University of Alabama, Birmingham; University of South Alabama, Monroeville; and AtlantiCare Cancer Care Institute, Egg Harbor Township, N.J., applied for participation in the Oncology Care Model introduced by the Centers for Medicare & Medicaid Services’ Center for Medicare & Medicaid Innovation.
“The goal of OCM is to utilize appropriately aligned financial incentives to enable improved care coordination, appropriateness of care, and access to care for beneficiaries undergoing chemotherapy,” according to CMS. “OCM encourages participating practices to improve care and lower costs through an episode-based payment model that financially incentivizes high-quality, coordinated care.”
Lead author Gabrielle Rocque, MD, assistant professor at the University of Alabama, Birmingham, noted that “these three cancer centers believed that leveraging the OCM requirement of treatment plan delivery would create an opportunity to improve care quality.”
They found that “implementation of OCM [treatment plans] has provided an opportunity to improve performance quality measures,” the authors concluded.
The project engaged 33 clinical providers and 171 women with breast cancer. The intervention group included 74 women aged 18 years and older with stage I to III breast cancer who were either planning on or already receiving chemotherapy; they were compared with a historical control group of 86 patients who received chemotherapy (J Oncol Pract. 2019. doi: 10.1200/JOP.18.00390).
Clinical providers engaged in self-study CME courses on quality standards relevant to human epidermal growth factor receptor 2 (HER2)–positive breast cancer and on psychosocial distress, then prepared patient treatment plans including patient-reported outcomes surveys that were connected to the clinical data platform. Fifteen American Society of Clinical Oncology Quality Oncology Practice Initiative measures were selected to compare the treatment and outcomes of the intervention and control groups.
“Statistically significant differences were found on nine measures, with performance higher among those in the intervention group,” Dr. Rocque and her colleagues noted. “Responses to questions that pertained to management of pain, emotional distress, and documentation of advanced directives had the greatest difference.” The areas that showed improvement aligned with indications linked to performance-based payments.
The study has several limitations. AtlantiCare Cancer Care Institute transitioned from a research phase to standard of care after 12 patients, altering the desired accrual of patients for the study. Additionally, “the quality improvement driver is not known because no manner existed to discern differences on the basis of documentation versus change in practice,” the investigators wrote.
That being said, the study authors stated that “the incorporation of technology solutions to meet requirements for participation in payment reform initiatives may provide a platform to effect patient outcomes.”
The study was supported by grants from the American Cancer Society and Genentech. Dr. Rocque reported support from Genentech and Pfizer.
SOURCE: Rocque G et al. J Oncol Pract. 2019. doi: 10.1200/JOP.18.00390.
Treatment plans derived under the Oncology Care Model (OCM) improved performance on some quality measures and patient-reported outcomes, according to a study performed at three cancer centers.
Physicians and care teams at the University of Alabama, Birmingham; University of South Alabama, Monroeville; and AtlantiCare Cancer Care Institute, Egg Harbor Township, N.J., applied for participation in the Oncology Care Model introduced by the Centers for Medicare & Medicaid Services’ Center for Medicare & Medicaid Innovation.
“The goal of OCM is to utilize appropriately aligned financial incentives to enable improved care coordination, appropriateness of care, and access to care for beneficiaries undergoing chemotherapy,” according to CMS. “OCM encourages participating practices to improve care and lower costs through an episode-based payment model that financially incentivizes high-quality, coordinated care.”
Lead author Gabrielle Rocque, MD, assistant professor at the University of Alabama, Birmingham, noted that “these three cancer centers believed that leveraging the OCM requirement of treatment plan delivery would create an opportunity to improve care quality.”
They found that “implementation of OCM [treatment plans] has provided an opportunity to improve performance quality measures,” the authors concluded.
The project engaged 33 clinical providers and 171 women with breast cancer. The intervention group included 74 women aged 18 years and older with stage I to III breast cancer who were either planning on or already receiving chemotherapy; they were compared with a historical control group of 86 patients who received chemotherapy (J Oncol Pract. 2019. doi: 10.1200/JOP.18.00390).
Clinical providers engaged in self-study CME courses on quality standards relevant to human epidermal growth factor receptor 2 (HER2)–positive breast cancer and on psychosocial distress, then prepared patient treatment plans including patient-reported outcomes surveys that were connected to the clinical data platform. Fifteen American Society of Clinical Oncology Quality Oncology Practice Initiative measures were selected to compare the treatment and outcomes of the intervention and control groups.
“Statistically significant differences were found on nine measures, with performance higher among those in the intervention group,” Dr. Rocque and her colleagues noted. “Responses to questions that pertained to management of pain, emotional distress, and documentation of advanced directives had the greatest difference.” The areas that showed improvement aligned with indications linked to performance-based payments.
The study has several limitations. AtlantiCare Cancer Care Institute transitioned from a research phase to standard of care after 12 patients, altering the desired accrual of patients for the study. Additionally, “the quality improvement driver is not known because no manner existed to discern differences on the basis of documentation versus change in practice,” the investigators wrote.
That being said, the study authors stated that “the incorporation of technology solutions to meet requirements for participation in payment reform initiatives may provide a platform to effect patient outcomes.”
The study was supported by grants from the American Cancer Society and Genentech. Dr. Rocque reported support from Genentech and Pfizer.
SOURCE: Rocque G et al. J Oncol Pract. 2019. doi: 10.1200/JOP.18.00390.
Treatment plans derived under the Oncology Care Model (OCM) improved performance on some quality measures and patient-reported outcomes, according to a study performed at three cancer centers.
Physicians and care teams at the University of Alabama, Birmingham; University of South Alabama, Monroeville; and AtlantiCare Cancer Care Institute, Egg Harbor Township, N.J., applied for participation in the Oncology Care Model introduced by the Centers for Medicare & Medicaid Services’ Center for Medicare & Medicaid Innovation.
“The goal of OCM is to utilize appropriately aligned financial incentives to enable improved care coordination, appropriateness of care, and access to care for beneficiaries undergoing chemotherapy,” according to CMS. “OCM encourages participating practices to improve care and lower costs through an episode-based payment model that financially incentivizes high-quality, coordinated care.”
Lead author Gabrielle Rocque, MD, assistant professor at the University of Alabama, Birmingham, noted that “these three cancer centers believed that leveraging the OCM requirement of treatment plan delivery would create an opportunity to improve care quality.”
They found that “implementation of OCM [treatment plans] has provided an opportunity to improve performance quality measures,” the authors concluded.
The project engaged 33 clinical providers and 171 women with breast cancer. The intervention group included 74 women aged 18 years and older with stage I to III breast cancer who were either planning on or already receiving chemotherapy; they were compared with a historical control group of 86 patients who received chemotherapy (J Oncol Pract. 2019. doi: 10.1200/JOP.18.00390).
Clinical providers engaged in self-study CME courses on quality standards relevant to human epidermal growth factor receptor 2 (HER2)–positive breast cancer and on psychosocial distress, then prepared patient treatment plans including patient-reported outcomes surveys that were connected to the clinical data platform. Fifteen American Society of Clinical Oncology Quality Oncology Practice Initiative measures were selected to compare the treatment and outcomes of the intervention and control groups.
“Statistically significant differences were found on nine measures, with performance higher among those in the intervention group,” Dr. Rocque and her colleagues noted. “Responses to questions that pertained to management of pain, emotional distress, and documentation of advanced directives had the greatest difference.” The areas that showed improvement aligned with indications linked to performance-based payments.
The study has several limitations. AtlantiCare Cancer Care Institute transitioned from a research phase to standard of care after 12 patients, altering the desired accrual of patients for the study. Additionally, “the quality improvement driver is not known because no manner existed to discern differences on the basis of documentation versus change in practice,” the investigators wrote.
That being said, the study authors stated that “the incorporation of technology solutions to meet requirements for participation in payment reform initiatives may provide a platform to effect patient outcomes.”
The study was supported by grants from the American Cancer Society and Genentech. Dr. Rocque reported support from Genentech and Pfizer.
SOURCE: Rocque G et al. J Oncol Pract. 2019. doi: 10.1200/JOP.18.00390.
FROM JOURNAL OF ONCOLOGY PRACTICE
Key clinical point: The CMS Oncology Care Model is showing promise to improve care.
Major finding: Intervention group saw statistically significant improvement in 9 of 15 quality measures, most notably those pertaining to pain management, emotional distress, and documentation of advanced directives.
Study details: A quality improvement project involving 171 breast cancer patients and 33 clinical providers.
Disclosures: The study was supported by grants from the American Cancer Society and Genentech. Dr. Rocque reported support from Genentech and Pfizer.
Source: Rocque G et al. J Oncol Pract. 2019. doi: 10. 1200/JOP.18.00390.
Elective hernia repair preferable in patients with chronic liver disease
Elective hernia repair in patients with chronic liver disease was far safer than emergent repair and carried an acceptable level of morbidity and mortality, according to an analysis of all cases performed at the Cleveland Clinic from 2001-2015.
In a chart review of 253 patients with chronic liver disease (CLD) who underwent hernia repair between January 2001 and December 2015, the rate of postoperative 30-day morbidity and mortality was 27% for nonemergent repairs, compared with 60% in emergent repairs.
The 90-day mortality rate also was higher for emergent repairs (10%) than for nonemergent repairs (3.7%), reported Clayton C. Petro, MD, of the Cleveland Clinic, and his coauthors.
Thirty-day morbidity and mortality was defined as incidence of surgical-site infection (SSI), wound dehiscence, bacterial peritonitis, decompensated liver failure, postoperative admission to the intensive care unit, unplanned hospital readmission, unplanned reoperation, and 30-day mortality. CLD severity was determined using the Charlson Comorbidity Index (CCI), age-adjusted CCI, Child-Turcott-Pugh Score, laboratory values, and Model for End-Stage Liver Disease (MELD) Score.
Of the 253 patients, 186 (74%) had nonemergent repairs and 67 (26%) had emergent repairs; 91 patients (36%) experienced a total of 159 morbidity and mortality events, Dr. Petro and coauthors said.
Emergent repairs had significantly higher rates of postoperative ICU admission than nonemergent repairs (27% vs. 5%; P less than .0001). Emergent repairs also had higher rates of bacterial peritonitis (10% vs 3%; P = .02), unplanned reoperation (9% vs 1%; P = .005), and unplanned readmission (27% vs 14%, P = .02).
“This large single-center cohort of 253 CLD patients suggests that non-emergent hernia repairs have relatively acceptable rates of [morbidity and mortality], even with advanced liver disease,” the authors wrote. “The dramatic increase in postoperative complications and 90-day mortality in the emergent setting supports the practice of elective repair when possible.”
No disclosures or conflicts of interest were reported.
SOURCE: Petro C et al. Am J Surg. 2019:217;59-65.
Elective hernia repair in patients with chronic liver disease was far safer than emergent repair and carried an acceptable level of morbidity and mortality, according to an analysis of all cases performed at the Cleveland Clinic from 2001-2015.
In a chart review of 253 patients with chronic liver disease (CLD) who underwent hernia repair between January 2001 and December 2015, the rate of postoperative 30-day morbidity and mortality was 27% for nonemergent repairs, compared with 60% in emergent repairs.
The 90-day mortality rate also was higher for emergent repairs (10%) than for nonemergent repairs (3.7%), reported Clayton C. Petro, MD, of the Cleveland Clinic, and his coauthors.
Thirty-day morbidity and mortality was defined as incidence of surgical-site infection (SSI), wound dehiscence, bacterial peritonitis, decompensated liver failure, postoperative admission to the intensive care unit, unplanned hospital readmission, unplanned reoperation, and 30-day mortality. CLD severity was determined using the Charlson Comorbidity Index (CCI), age-adjusted CCI, Child-Turcott-Pugh Score, laboratory values, and Model for End-Stage Liver Disease (MELD) Score.
Of the 253 patients, 186 (74%) had nonemergent repairs and 67 (26%) had emergent repairs; 91 patients (36%) experienced a total of 159 morbidity and mortality events, Dr. Petro and coauthors said.
Emergent repairs had significantly higher rates of postoperative ICU admission than nonemergent repairs (27% vs. 5%; P less than .0001). Emergent repairs also had higher rates of bacterial peritonitis (10% vs 3%; P = .02), unplanned reoperation (9% vs 1%; P = .005), and unplanned readmission (27% vs 14%, P = .02).
“This large single-center cohort of 253 CLD patients suggests that non-emergent hernia repairs have relatively acceptable rates of [morbidity and mortality], even with advanced liver disease,” the authors wrote. “The dramatic increase in postoperative complications and 90-day mortality in the emergent setting supports the practice of elective repair when possible.”
No disclosures or conflicts of interest were reported.
SOURCE: Petro C et al. Am J Surg. 2019:217;59-65.
Elective hernia repair in patients with chronic liver disease was far safer than emergent repair and carried an acceptable level of morbidity and mortality, according to an analysis of all cases performed at the Cleveland Clinic from 2001-2015.
In a chart review of 253 patients with chronic liver disease (CLD) who underwent hernia repair between January 2001 and December 2015, the rate of postoperative 30-day morbidity and mortality was 27% for nonemergent repairs, compared with 60% in emergent repairs.
The 90-day mortality rate also was higher for emergent repairs (10%) than for nonemergent repairs (3.7%), reported Clayton C. Petro, MD, of the Cleveland Clinic, and his coauthors.
Thirty-day morbidity and mortality was defined as incidence of surgical-site infection (SSI), wound dehiscence, bacterial peritonitis, decompensated liver failure, postoperative admission to the intensive care unit, unplanned hospital readmission, unplanned reoperation, and 30-day mortality. CLD severity was determined using the Charlson Comorbidity Index (CCI), age-adjusted CCI, Child-Turcott-Pugh Score, laboratory values, and Model for End-Stage Liver Disease (MELD) Score.
Of the 253 patients, 186 (74%) had nonemergent repairs and 67 (26%) had emergent repairs; 91 patients (36%) experienced a total of 159 morbidity and mortality events, Dr. Petro and coauthors said.
Emergent repairs had significantly higher rates of postoperative ICU admission than nonemergent repairs (27% vs. 5%; P less than .0001). Emergent repairs also had higher rates of bacterial peritonitis (10% vs 3%; P = .02), unplanned reoperation (9% vs 1%; P = .005), and unplanned readmission (27% vs 14%, P = .02).
“This large single-center cohort of 253 CLD patients suggests that non-emergent hernia repairs have relatively acceptable rates of [morbidity and mortality], even with advanced liver disease,” the authors wrote. “The dramatic increase in postoperative complications and 90-day mortality in the emergent setting supports the practice of elective repair when possible.”
No disclosures or conflicts of interest were reported.
SOURCE: Petro C et al. Am J Surg. 2019:217;59-65.
FROM THE AMERICAN JOURNAL OF SURGERY
Key clinical point: Emergent hernia repairs had higher morbidity and mortality than nonemergent repairs in patients with chronic liver disease.
Major finding: The rate of postoperative 30-day morbidity and mortality was 27% for nonemergent repairs, compared with 60% in emergent repairs.
Study details: Chart review of 253 CLD patients who underwent hernia repair between January 2001 and December 2015.
Disclosures: No disclosures or conflicts of interest were reported.
Source: Petro C et al. Am J Surg. 2019:217;59-65.
The blinding lies of depression
Numb and empty, I continued to drive home in a daze. My mind focused only on the light ahead changing from yellow to red. “Remember to step on the brake,” commanded the internal boss to my stunned mind. No tears, I continued to drive as green blinked its eye.
Earlier that afternoon as I stepped out of my second outpatient appointment of the day, the office administrator’s assistant gingerly informed me, “The guy who answered the phone for your no-show said she passed.”
“Passed? Like … died?” I asked in shock.
She nodded. “I looked her up in the system. She passed away 2 Saturdays ago.”
That was only 2 days after the last time I met with her when we celebrated her progress.
“Too soon, too soon in your career,” my attending bemoaned as I shared the news.
Gathering my scattered wit, I smoothed my furrowed brow and forced a smile back into my eyes. I had other patients to see.
Continue to: Soothed by the hum of my car...
Soothed by the hum of my car, my mind replayed our last meeting where hope and active plans had replaced broken hopelessness. For the past 2 weeks, I had erroneously dismissed her no-shows as her volatile borderline personality’s decision to fire me. I was wrong.
Holding things together until a silly domestic dispute unleashed the brewing tornado inside, I stormed upstairs to contain the pain. Behind locked doors, my body shuddered from uncontrollable tears that blinded my eyes. She was the first patient I helped through psychotherapy and the first I lost through suicide.
The news of her death triggered anguish from past suicides of dear friends. Chopper, who blew off his face during our sophomore y
A few years later, another classmate, Aaron, sank into depression. He, too, shot himself. Just months before I’d received the call requesting my presence at his funeral, he had asked me if I would be his Valentine. Jokingly, I agreed, knowing our paths would never cross after our graduation. At his funeral, his parents insisted that I sat as a member of his immediate family.
Oh … the blinding lies of depression. Those who have fallen prey to suicide never knew the truth: Their lives and their deaths matter.
Even strangers weep.
Numb and empty, I continued to drive home in a daze. My mind focused only on the light ahead changing from yellow to red. “Remember to step on the brake,” commanded the internal boss to my stunned mind. No tears, I continued to drive as green blinked its eye.
Earlier that afternoon as I stepped out of my second outpatient appointment of the day, the office administrator’s assistant gingerly informed me, “The guy who answered the phone for your no-show said she passed.”
“Passed? Like … died?” I asked in shock.
She nodded. “I looked her up in the system. She passed away 2 Saturdays ago.”
That was only 2 days after the last time I met with her when we celebrated her progress.
“Too soon, too soon in your career,” my attending bemoaned as I shared the news.
Gathering my scattered wit, I smoothed my furrowed brow and forced a smile back into my eyes. I had other patients to see.
Continue to: Soothed by the hum of my car...
Soothed by the hum of my car, my mind replayed our last meeting where hope and active plans had replaced broken hopelessness. For the past 2 weeks, I had erroneously dismissed her no-shows as her volatile borderline personality’s decision to fire me. I was wrong.
Holding things together until a silly domestic dispute unleashed the brewing tornado inside, I stormed upstairs to contain the pain. Behind locked doors, my body shuddered from uncontrollable tears that blinded my eyes. She was the first patient I helped through psychotherapy and the first I lost through suicide.
The news of her death triggered anguish from past suicides of dear friends. Chopper, who blew off his face during our sophomore y
A few years later, another classmate, Aaron, sank into depression. He, too, shot himself. Just months before I’d received the call requesting my presence at his funeral, he had asked me if I would be his Valentine. Jokingly, I agreed, knowing our paths would never cross after our graduation. At his funeral, his parents insisted that I sat as a member of his immediate family.
Oh … the blinding lies of depression. Those who have fallen prey to suicide never knew the truth: Their lives and their deaths matter.
Even strangers weep.
Numb and empty, I continued to drive home in a daze. My mind focused only on the light ahead changing from yellow to red. “Remember to step on the brake,” commanded the internal boss to my stunned mind. No tears, I continued to drive as green blinked its eye.
Earlier that afternoon as I stepped out of my second outpatient appointment of the day, the office administrator’s assistant gingerly informed me, “The guy who answered the phone for your no-show said she passed.”
“Passed? Like … died?” I asked in shock.
She nodded. “I looked her up in the system. She passed away 2 Saturdays ago.”
That was only 2 days after the last time I met with her when we celebrated her progress.
“Too soon, too soon in your career,” my attending bemoaned as I shared the news.
Gathering my scattered wit, I smoothed my furrowed brow and forced a smile back into my eyes. I had other patients to see.
Continue to: Soothed by the hum of my car...
Soothed by the hum of my car, my mind replayed our last meeting where hope and active plans had replaced broken hopelessness. For the past 2 weeks, I had erroneously dismissed her no-shows as her volatile borderline personality’s decision to fire me. I was wrong.
Holding things together until a silly domestic dispute unleashed the brewing tornado inside, I stormed upstairs to contain the pain. Behind locked doors, my body shuddered from uncontrollable tears that blinded my eyes. She was the first patient I helped through psychotherapy and the first I lost through suicide.
The news of her death triggered anguish from past suicides of dear friends. Chopper, who blew off his face during our sophomore y
A few years later, another classmate, Aaron, sank into depression. He, too, shot himself. Just months before I’d received the call requesting my presence at his funeral, he had asked me if I would be his Valentine. Jokingly, I agreed, knowing our paths would never cross after our graduation. At his funeral, his parents insisted that I sat as a member of his immediate family.
Oh … the blinding lies of depression. Those who have fallen prey to suicide never knew the truth: Their lives and their deaths matter.
Even strangers weep.
Consider timing and technique before hernia repair in patients with cirrhosis
but only when accompanied by careful selection of patients, operative timing, and technique, according to a literature review of studies on hernia management in cirrhosis.

“Hernia management in cirrhosis continues to be restricted by lack of high-quality evidence and heterogeneity in expert opinion,” wrote lead author Sara P. Myers, MD, of the University of Pittsburgh, and her coauthors, adding that “there is, however, convincing evidence to advocate for elective ventral, umbilical, or inguinal hernia repair in compensated cirrhosis.” The study was published in the Journal of Surgical Research.
After reviewing 51 articles – including 7 prospective observational studies, 26 retrospective observational studies, 2 randomized controlled trials, 15 review articles, and 1 case report – Dr. Myers and her colleagues organized their data into three categories: preoperative, intraoperative, or postoperative considerations.
From a preoperative standpoint, decompensated cirrhosis was recognized as a “harbinger of poor outcomes.” Signs of decompensated cirrhosis include ascites, variceal bleeding, spontaneous bacterial peritonitis, hepatic encephalopathy, and hepatorenal syndrome. A 2006 study found that patients with decompensated cirrhosis survive for a median of less than 2 years, while those with compensated cirrhosis has a median survival of more than 12 years.
Intraoperative considerations leaned on studies of cholecystectomy; the evidence suggested that patients with mild to moderate cirrhosis can undergo laparoscopic surgery, even showing decreased risk of mortality, pneumonia, sepsis, and reoperation as a result. And although most laparoscopic procedures involve an intraperitoneal onlay mesh repair and the “use of mesh for hernia repair in patients with cirrhosis has been debated,” a 2007 study showed that synthetic mesh is safe for elective herniorrhaphy.
Finally, they shared specific postoperative risks, including encephalopathy and ascites, along with the fact that cirrhosis itself “precipitates immune dysfunction and deficiency and promotes systemic inflammation.” At the same time, they highlighted a 2008 study in which a cohort of 32 patients with cirrhosis underwent elective Lichtenstein repair with no major complications and an overall improved quality of life.
The coauthors noted that, although many surgeons will avoid hernia repair in patients with severe liver disease because of the associations with high morbidity and mortality, dissent fades when an emergency means abstaining will lead to a prognosis worse than intervention. That said, when it comes to preemptive elective repair there are also “no clear guidelines with regard to severity of cirrhosis and thresholds that would preclude herniorrhaphy.” Regardless of the choices made, “recognizing and managing complications in cirrhotic patients who have undergone hernia repair is crucial,” they wrote.
The authors reported no conflicts of interest.
SOURCE: Myers SP et al. J Surg Res. 2018 Oct 23. doi: doi: 10.1016/j.jss.2018.09.052.
but only when accompanied by careful selection of patients, operative timing, and technique, according to a literature review of studies on hernia management in cirrhosis.

“Hernia management in cirrhosis continues to be restricted by lack of high-quality evidence and heterogeneity in expert opinion,” wrote lead author Sara P. Myers, MD, of the University of Pittsburgh, and her coauthors, adding that “there is, however, convincing evidence to advocate for elective ventral, umbilical, or inguinal hernia repair in compensated cirrhosis.” The study was published in the Journal of Surgical Research.
After reviewing 51 articles – including 7 prospective observational studies, 26 retrospective observational studies, 2 randomized controlled trials, 15 review articles, and 1 case report – Dr. Myers and her colleagues organized their data into three categories: preoperative, intraoperative, or postoperative considerations.
From a preoperative standpoint, decompensated cirrhosis was recognized as a “harbinger of poor outcomes.” Signs of decompensated cirrhosis include ascites, variceal bleeding, spontaneous bacterial peritonitis, hepatic encephalopathy, and hepatorenal syndrome. A 2006 study found that patients with decompensated cirrhosis survive for a median of less than 2 years, while those with compensated cirrhosis has a median survival of more than 12 years.
Intraoperative considerations leaned on studies of cholecystectomy; the evidence suggested that patients with mild to moderate cirrhosis can undergo laparoscopic surgery, even showing decreased risk of mortality, pneumonia, sepsis, and reoperation as a result. And although most laparoscopic procedures involve an intraperitoneal onlay mesh repair and the “use of mesh for hernia repair in patients with cirrhosis has been debated,” a 2007 study showed that synthetic mesh is safe for elective herniorrhaphy.
Finally, they shared specific postoperative risks, including encephalopathy and ascites, along with the fact that cirrhosis itself “precipitates immune dysfunction and deficiency and promotes systemic inflammation.” At the same time, they highlighted a 2008 study in which a cohort of 32 patients with cirrhosis underwent elective Lichtenstein repair with no major complications and an overall improved quality of life.
The coauthors noted that, although many surgeons will avoid hernia repair in patients with severe liver disease because of the associations with high morbidity and mortality, dissent fades when an emergency means abstaining will lead to a prognosis worse than intervention. That said, when it comes to preemptive elective repair there are also “no clear guidelines with regard to severity of cirrhosis and thresholds that would preclude herniorrhaphy.” Regardless of the choices made, “recognizing and managing complications in cirrhotic patients who have undergone hernia repair is crucial,” they wrote.
The authors reported no conflicts of interest.
SOURCE: Myers SP et al. J Surg Res. 2018 Oct 23. doi: doi: 10.1016/j.jss.2018.09.052.
but only when accompanied by careful selection of patients, operative timing, and technique, according to a literature review of studies on hernia management in cirrhosis.

“Hernia management in cirrhosis continues to be restricted by lack of high-quality evidence and heterogeneity in expert opinion,” wrote lead author Sara P. Myers, MD, of the University of Pittsburgh, and her coauthors, adding that “there is, however, convincing evidence to advocate for elective ventral, umbilical, or inguinal hernia repair in compensated cirrhosis.” The study was published in the Journal of Surgical Research.
After reviewing 51 articles – including 7 prospective observational studies, 26 retrospective observational studies, 2 randomized controlled trials, 15 review articles, and 1 case report – Dr. Myers and her colleagues organized their data into three categories: preoperative, intraoperative, or postoperative considerations.
From a preoperative standpoint, decompensated cirrhosis was recognized as a “harbinger of poor outcomes.” Signs of decompensated cirrhosis include ascites, variceal bleeding, spontaneous bacterial peritonitis, hepatic encephalopathy, and hepatorenal syndrome. A 2006 study found that patients with decompensated cirrhosis survive for a median of less than 2 years, while those with compensated cirrhosis has a median survival of more than 12 years.
Intraoperative considerations leaned on studies of cholecystectomy; the evidence suggested that patients with mild to moderate cirrhosis can undergo laparoscopic surgery, even showing decreased risk of mortality, pneumonia, sepsis, and reoperation as a result. And although most laparoscopic procedures involve an intraperitoneal onlay mesh repair and the “use of mesh for hernia repair in patients with cirrhosis has been debated,” a 2007 study showed that synthetic mesh is safe for elective herniorrhaphy.
Finally, they shared specific postoperative risks, including encephalopathy and ascites, along with the fact that cirrhosis itself “precipitates immune dysfunction and deficiency and promotes systemic inflammation.” At the same time, they highlighted a 2008 study in which a cohort of 32 patients with cirrhosis underwent elective Lichtenstein repair with no major complications and an overall improved quality of life.
The coauthors noted that, although many surgeons will avoid hernia repair in patients with severe liver disease because of the associations with high morbidity and mortality, dissent fades when an emergency means abstaining will lead to a prognosis worse than intervention. That said, when it comes to preemptive elective repair there are also “no clear guidelines with regard to severity of cirrhosis and thresholds that would preclude herniorrhaphy.” Regardless of the choices made, “recognizing and managing complications in cirrhotic patients who have undergone hernia repair is crucial,” they wrote.
The authors reported no conflicts of interest.
SOURCE: Myers SP et al. J Surg Res. 2018 Oct 23. doi: doi: 10.1016/j.jss.2018.09.052.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: With careful selection of patients, operative timing, and technique, herniorrhaphy may be appropriate in patients with cirrhosis.
Major finding: Patients with decompensated cirrhosis survived for a median of less than 2 years while those with compensated cirrhosis had a median survival of more than 12 years.
Study details: A literature review of 51 conference abstracts, review articles, randomized clinical trials, and observational studies.
Disclosures: The authors reported no conflicts of interest.
Source: Myers SP et al. J Surg Res. 2018 Oct 23. doi: 10.1016/j.jss.2018.09.052.
Aerobic exercise may mitigate age-related cognitive decline
published in Neurology.
“The effect of aerobic exercise on executive function was more pronounced as age increased, suggesting that it may mitigate age-related declines,” wrote Yaakov Stern, PhD, chief of cognitive neuroscience in the department of neurology at Columbia University, New York, and his research colleagues.
Research indicates that aerobic exercise provides cognitive benefits across the lifespan, but controlled exercise studies have been limited to elderly individuals, the researchers wrote. To examine the effects of aerobic exercise on cognitive function in younger, healthy adults, they conducted a randomized, parallel-group, observer-masked, community-based clinical trial. The investigators enrolled 132 cognitively normal people aged 20-67 years with aerobic capacity below the median. About 70% were women, and participants’ mean age was about 40 years.
“We hypothesized that aerobic exercise would have cognitive benefits, even in this younger age range, but that age might moderate the nature or degree of the benefit,” Dr. Stern and his colleagues wrote.
Participants were nonsmoking, habitual nonexercisers with below-average fitness by American Heart Association standards. The investigators used baseline aerobic capacity testing to establish safe exercise measures and heart rate targets.
The investigators randomly assigned participants to a group that performed aerobic exercise or to a control group that performed stretching and toning four times per week for 6 months. Outcome measures included domains of cognitive function (such as executive function, episodic memory, processing speed, language, and attention), everyday function, aerobic capacity, body mass index, and cortical thickness.
During a 2-week run-in period, participants went to their choice of five YMCA of New York City fitness centers three times per week. They had to attend at least five of these sessions to stay in the study. In both study arms, training sessions consisted of 10-15 minutes of warm-up and cooldown and 30-40 minutes of workout. Coaches contacted participants weekly to monitor their progress, and participants wore heart rate monitors during each session. Exercises in the control group were designed to promote flexibility and improve core strength. In the aerobic exercise group, participants had a choice of exercises such as walking on a treadmill, cycling on a stationary bike, or using an elliptical machine, and they gradually increased their exercise intensity to 75% of maximum heart rate by week 5. A total of 94 participants – 50 in the control group and 44 in the aerobic exercise group – completed the 6-month trial.
Executive function, but not other cognitive measures, improved significantly in the aerobic exercise group. The effect on executive function was greater in older participants. For example, at age 40 years, the executive function measure increased by 0.228 standard deviation units from baseline; at age 60, it increased by 0.596 standard deviation units.
In addition, cortical thickness increased significantly in the aerobic exercise group in the left caudal middle frontal cortex Brodmann area; this effect did not differ by age. Improvement on executive function in the aerobic exercise group was greater among participants without an APOE E4 allele, contrasting with the findings of prior studies.
“Since a difference of 0.5 standard deviations is equivalent to 20 years of age-related difference in performance on these tests, the people who exercised were testing as if they were about 10 years younger at age 40 and about 20 years younger at age 60,” Dr. Stern said in a press release. “Since thinking skills at the start of the study were poorer for participants who were older, our findings suggest that aerobic exercise is more likely to improve age-related declines in thinking skills rather than improve performance in those without a decline.”
Furthermore, aerobic exercise significantly increased aerobic capacity and significantly decreased body mass index, whereas stretching and toning did not.
“Participants in this trial scheduled their exercise sessions on their own and exercised by themselves,” the authors noted. “In addition, they were allowed to choose whatever aerobic exercise modality they preferred, so long as they reached target heart rates, enhancing the flexibility of the intervention.” Limitations of the study include its relatively small sample size and the large number of participants who dropped out of the study between consenting to participate and randomization.
The trial was funded by the National Institutes of Health. Dr. Stern reported receiving a grant from the California Walnut Commission and consulting with Eli Lilly, Axovant Sciences, Takeda, and AbbVie. A coauthor reported grant support from AposTherapy, LIH Medical, and the Everest Foundation.
SOURCE: Stern Y et al. Neurology. 2019 Jan 30. doi: 10.1212/WNL.0000000000007003.
published in Neurology.
“The effect of aerobic exercise on executive function was more pronounced as age increased, suggesting that it may mitigate age-related declines,” wrote Yaakov Stern, PhD, chief of cognitive neuroscience in the department of neurology at Columbia University, New York, and his research colleagues.
Research indicates that aerobic exercise provides cognitive benefits across the lifespan, but controlled exercise studies have been limited to elderly individuals, the researchers wrote. To examine the effects of aerobic exercise on cognitive function in younger, healthy adults, they conducted a randomized, parallel-group, observer-masked, community-based clinical trial. The investigators enrolled 132 cognitively normal people aged 20-67 years with aerobic capacity below the median. About 70% were women, and participants’ mean age was about 40 years.
“We hypothesized that aerobic exercise would have cognitive benefits, even in this younger age range, but that age might moderate the nature or degree of the benefit,” Dr. Stern and his colleagues wrote.
Participants were nonsmoking, habitual nonexercisers with below-average fitness by American Heart Association standards. The investigators used baseline aerobic capacity testing to establish safe exercise measures and heart rate targets.
The investigators randomly assigned participants to a group that performed aerobic exercise or to a control group that performed stretching and toning four times per week for 6 months. Outcome measures included domains of cognitive function (such as executive function, episodic memory, processing speed, language, and attention), everyday function, aerobic capacity, body mass index, and cortical thickness.
During a 2-week run-in period, participants went to their choice of five YMCA of New York City fitness centers three times per week. They had to attend at least five of these sessions to stay in the study. In both study arms, training sessions consisted of 10-15 minutes of warm-up and cooldown and 30-40 minutes of workout. Coaches contacted participants weekly to monitor their progress, and participants wore heart rate monitors during each session. Exercises in the control group were designed to promote flexibility and improve core strength. In the aerobic exercise group, participants had a choice of exercises such as walking on a treadmill, cycling on a stationary bike, or using an elliptical machine, and they gradually increased their exercise intensity to 75% of maximum heart rate by week 5. A total of 94 participants – 50 in the control group and 44 in the aerobic exercise group – completed the 6-month trial.
Executive function, but not other cognitive measures, improved significantly in the aerobic exercise group. The effect on executive function was greater in older participants. For example, at age 40 years, the executive function measure increased by 0.228 standard deviation units from baseline; at age 60, it increased by 0.596 standard deviation units.
In addition, cortical thickness increased significantly in the aerobic exercise group in the left caudal middle frontal cortex Brodmann area; this effect did not differ by age. Improvement on executive function in the aerobic exercise group was greater among participants without an APOE E4 allele, contrasting with the findings of prior studies.
“Since a difference of 0.5 standard deviations is equivalent to 20 years of age-related difference in performance on these tests, the people who exercised were testing as if they were about 10 years younger at age 40 and about 20 years younger at age 60,” Dr. Stern said in a press release. “Since thinking skills at the start of the study were poorer for participants who were older, our findings suggest that aerobic exercise is more likely to improve age-related declines in thinking skills rather than improve performance in those without a decline.”
Furthermore, aerobic exercise significantly increased aerobic capacity and significantly decreased body mass index, whereas stretching and toning did not.
“Participants in this trial scheduled their exercise sessions on their own and exercised by themselves,” the authors noted. “In addition, they were allowed to choose whatever aerobic exercise modality they preferred, so long as they reached target heart rates, enhancing the flexibility of the intervention.” Limitations of the study include its relatively small sample size and the large number of participants who dropped out of the study between consenting to participate and randomization.
The trial was funded by the National Institutes of Health. Dr. Stern reported receiving a grant from the California Walnut Commission and consulting with Eli Lilly, Axovant Sciences, Takeda, and AbbVie. A coauthor reported grant support from AposTherapy, LIH Medical, and the Everest Foundation.
SOURCE: Stern Y et al. Neurology. 2019 Jan 30. doi: 10.1212/WNL.0000000000007003.
published in Neurology.
“The effect of aerobic exercise on executive function was more pronounced as age increased, suggesting that it may mitigate age-related declines,” wrote Yaakov Stern, PhD, chief of cognitive neuroscience in the department of neurology at Columbia University, New York, and his research colleagues.
Research indicates that aerobic exercise provides cognitive benefits across the lifespan, but controlled exercise studies have been limited to elderly individuals, the researchers wrote. To examine the effects of aerobic exercise on cognitive function in younger, healthy adults, they conducted a randomized, parallel-group, observer-masked, community-based clinical trial. The investigators enrolled 132 cognitively normal people aged 20-67 years with aerobic capacity below the median. About 70% were women, and participants’ mean age was about 40 years.
“We hypothesized that aerobic exercise would have cognitive benefits, even in this younger age range, but that age might moderate the nature or degree of the benefit,” Dr. Stern and his colleagues wrote.
Participants were nonsmoking, habitual nonexercisers with below-average fitness by American Heart Association standards. The investigators used baseline aerobic capacity testing to establish safe exercise measures and heart rate targets.
The investigators randomly assigned participants to a group that performed aerobic exercise or to a control group that performed stretching and toning four times per week for 6 months. Outcome measures included domains of cognitive function (such as executive function, episodic memory, processing speed, language, and attention), everyday function, aerobic capacity, body mass index, and cortical thickness.
During a 2-week run-in period, participants went to their choice of five YMCA of New York City fitness centers three times per week. They had to attend at least five of these sessions to stay in the study. In both study arms, training sessions consisted of 10-15 minutes of warm-up and cooldown and 30-40 minutes of workout. Coaches contacted participants weekly to monitor their progress, and participants wore heart rate monitors during each session. Exercises in the control group were designed to promote flexibility and improve core strength. In the aerobic exercise group, participants had a choice of exercises such as walking on a treadmill, cycling on a stationary bike, or using an elliptical machine, and they gradually increased their exercise intensity to 75% of maximum heart rate by week 5. A total of 94 participants – 50 in the control group and 44 in the aerobic exercise group – completed the 6-month trial.
Executive function, but not other cognitive measures, improved significantly in the aerobic exercise group. The effect on executive function was greater in older participants. For example, at age 40 years, the executive function measure increased by 0.228 standard deviation units from baseline; at age 60, it increased by 0.596 standard deviation units.
In addition, cortical thickness increased significantly in the aerobic exercise group in the left caudal middle frontal cortex Brodmann area; this effect did not differ by age. Improvement on executive function in the aerobic exercise group was greater among participants without an APOE E4 allele, contrasting with the findings of prior studies.
“Since a difference of 0.5 standard deviations is equivalent to 20 years of age-related difference in performance on these tests, the people who exercised were testing as if they were about 10 years younger at age 40 and about 20 years younger at age 60,” Dr. Stern said in a press release. “Since thinking skills at the start of the study were poorer for participants who were older, our findings suggest that aerobic exercise is more likely to improve age-related declines in thinking skills rather than improve performance in those without a decline.”
Furthermore, aerobic exercise significantly increased aerobic capacity and significantly decreased body mass index, whereas stretching and toning did not.
“Participants in this trial scheduled their exercise sessions on their own and exercised by themselves,” the authors noted. “In addition, they were allowed to choose whatever aerobic exercise modality they preferred, so long as they reached target heart rates, enhancing the flexibility of the intervention.” Limitations of the study include its relatively small sample size and the large number of participants who dropped out of the study between consenting to participate and randomization.
The trial was funded by the National Institutes of Health. Dr. Stern reported receiving a grant from the California Walnut Commission and consulting with Eli Lilly, Axovant Sciences, Takeda, and AbbVie. A coauthor reported grant support from AposTherapy, LIH Medical, and the Everest Foundation.
SOURCE: Stern Y et al. Neurology. 2019 Jan 30. doi: 10.1212/WNL.0000000000007003.
FROM NEUROLOGY
Key clinical point: Among adults with below-average fitness, a 6-month aerobic exercise program significantly improves executive function.
Major finding: The effect is more pronounced as age increases.
Study details: A randomized, parallel-group, observer-masked, community-based clinical trial of 132 cognitively normal adults aged 20-67 years.
Disclosures: The study was funded by the National Institutes of Health. Dr. Stern reported receiving a grant from the California Walnut Commission and consulted with Eli Lilly, Axovant Sciences, Takeda, and AbbVie. Another reported grant support from AposTherapy, LIH Medical, and the Everest Foundation.
Source: Stern Y et al. Neurology. 2019 Jan 30. doi: 10.1212/WNL.0000000000007003.
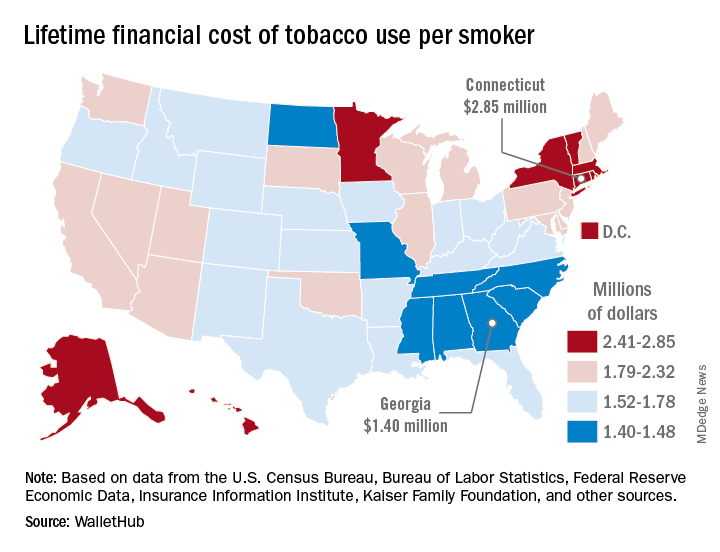
Lifetime cost of tobacco use tops $1.9 million per smoker
according to the personal financial website WalletHub.
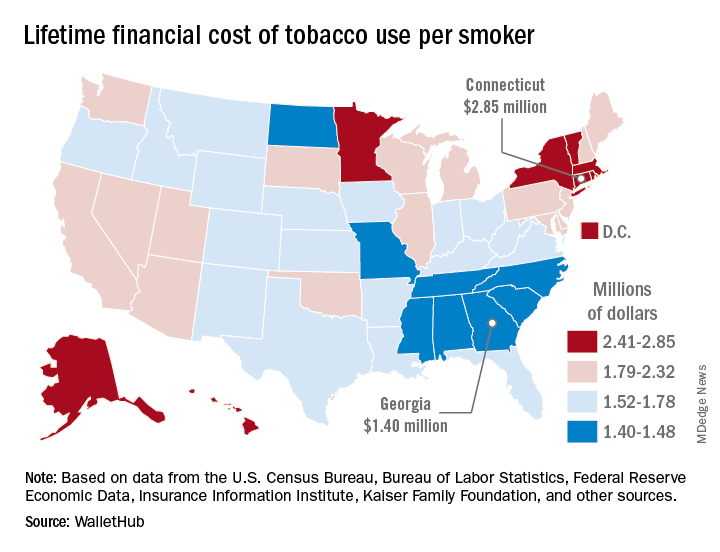
Economic and societal losses related to 37.8 million U.S. tobacco users – including out-of-pocket spending for cigarettes, health care expenses, and lost income – top $300 billion annually, but those costs vary considerably by state, WalletHub said in a recent report.
The state with the highest lifetime cost per smoker is Connecticut, with an estimated total of $2.85 million. That works out to just under $56,000 a year for 51 years because lifetime use was defined as one pack a day starting at age 18 years and continuing until age 69 years. New York has the second-highest lifetime cost, which also rounds off to $2.85 million, followed by the District of Columbia ($2.81 million), Massachusetts ($2.76 million), and Rhode Island ($2.68 million), WalletHub said.
Georgia has the lowest lifetime cost of any state – $1.40 million per smoker – followed by Missouri at $1.41 million, North Carolina at $1.42 million, Mississippi at $1.43 million, and South Carolina at $1.44 million, according to the report.
WalletHub’s formula for total lifetime cost has five components: out-of-pocket cost (one pack of cigarettes per day for 51 years), financial opportunity cost (defined as “the amount of return a person would have earned by instead investing that money in the stock market”), health care cost (spending on treatment for smoking-related health complications), income loss (an average 8% decrease caused by absenteeism and lost productivity), and other costs (loss of a homeowner’s insurance credit and costs of secondhand exposure).
The analysis was based on data from the U.S. Census Bureau, Bureau of Labor Statistics, Centers for Disease Control and Prevention, Insurance Information Institute, Campaign for Tobacco-Free Kids, NYsmokefree.com, Federal Reserve Economic Data, Kaiser Family Foundation, and the Independent Insurance Agents & Brokers of America.
according to the personal financial website WalletHub.
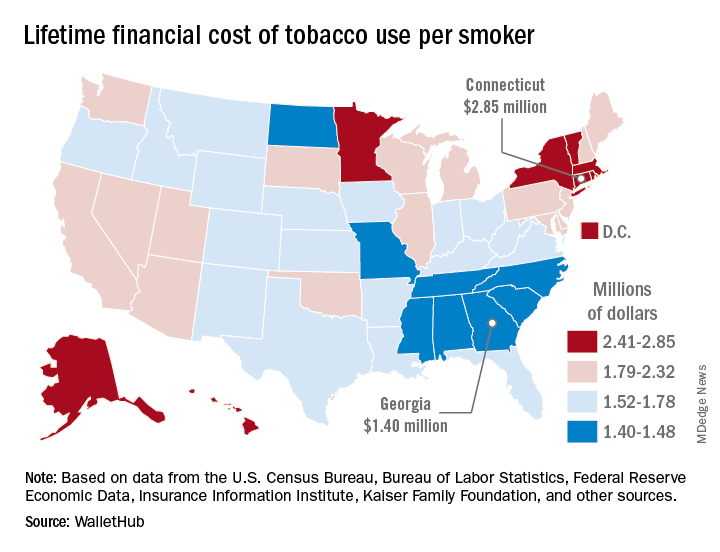
Economic and societal losses related to 37.8 million U.S. tobacco users – including out-of-pocket spending for cigarettes, health care expenses, and lost income – top $300 billion annually, but those costs vary considerably by state, WalletHub said in a recent report.
The state with the highest lifetime cost per smoker is Connecticut, with an estimated total of $2.85 million. That works out to just under $56,000 a year for 51 years because lifetime use was defined as one pack a day starting at age 18 years and continuing until age 69 years. New York has the second-highest lifetime cost, which also rounds off to $2.85 million, followed by the District of Columbia ($2.81 million), Massachusetts ($2.76 million), and Rhode Island ($2.68 million), WalletHub said.
Georgia has the lowest lifetime cost of any state – $1.40 million per smoker – followed by Missouri at $1.41 million, North Carolina at $1.42 million, Mississippi at $1.43 million, and South Carolina at $1.44 million, according to the report.
WalletHub’s formula for total lifetime cost has five components: out-of-pocket cost (one pack of cigarettes per day for 51 years), financial opportunity cost (defined as “the amount of return a person would have earned by instead investing that money in the stock market”), health care cost (spending on treatment for smoking-related health complications), income loss (an average 8% decrease caused by absenteeism and lost productivity), and other costs (loss of a homeowner’s insurance credit and costs of secondhand exposure).
The analysis was based on data from the U.S. Census Bureau, Bureau of Labor Statistics, Centers for Disease Control and Prevention, Insurance Information Institute, Campaign for Tobacco-Free Kids, NYsmokefree.com, Federal Reserve Economic Data, Kaiser Family Foundation, and the Independent Insurance Agents & Brokers of America.
according to the personal financial website WalletHub.
Economic and societal losses related to 37.8 million U.S. tobacco users – including out-of-pocket spending for cigarettes, health care expenses, and lost income – top $300 billion annually, but those costs vary considerably by state, WalletHub said in a recent report.
The state with the highest lifetime cost per smoker is Connecticut, with an estimated total of $2.85 million. That works out to just under $56,000 a year for 51 years because lifetime use was defined as one pack a day starting at age 18 years and continuing until age 69 years. New York has the second-highest lifetime cost, which also rounds off to $2.85 million, followed by the District of Columbia ($2.81 million), Massachusetts ($2.76 million), and Rhode Island ($2.68 million), WalletHub said.
Georgia has the lowest lifetime cost of any state – $1.40 million per smoker – followed by Missouri at $1.41 million, North Carolina at $1.42 million, Mississippi at $1.43 million, and South Carolina at $1.44 million, according to the report.
WalletHub’s formula for total lifetime cost has five components: out-of-pocket cost (one pack of cigarettes per day for 51 years), financial opportunity cost (defined as “the amount of return a person would have earned by instead investing that money in the stock market”), health care cost (spending on treatment for smoking-related health complications), income loss (an average 8% decrease caused by absenteeism and lost productivity), and other costs (loss of a homeowner’s insurance credit and costs of secondhand exposure).
The analysis was based on data from the U.S. Census Bureau, Bureau of Labor Statistics, Centers for Disease Control and Prevention, Insurance Information Institute, Campaign for Tobacco-Free Kids, NYsmokefree.com, Federal Reserve Economic Data, Kaiser Family Foundation, and the Independent Insurance Agents & Brokers of America.
Pulmonary hypertension linked to complications after head and neck procedures
SAN DIEGO – Patients with , compared with their counterparts who do not have the condition. They also face an increase in total charges and length of stay.
The findings come from what is believed to be the first study of its kind to investigate the impact of pulmonary hypertension (PHTN) on major head and neck procedures. “PHTN is a common condition which affects the caliber of lung vasculature, with varied symptom presentation from shortness of breath to syncope, with an estimated prevalence of 2.5 to 7.1 million new cases each year worldwide,” one of the study authors, Nirali M. Patel, said at the Triological Society’s Combined Sections Meeting. “Due to improved therapeutic options, there is an enhanced survival of PHTN patients and higher prevalence of this disease. PHTN has some significant systemic implications. Therefore, cardiopulmonary clearance and a clear understanding of postoperative complications are very important.”
Previous studies have shown PHTN to be an independent predictor of morbidity and mortality in noncardiac procedures, said Ms. Patel, a fourth-year medical student at New Jersey Medical School, Newark. Furthermore, the rate of pulmonary complications is reported to be between 11% and 44.8% following radical head and neck cancer resection. “Despite these findings, there is currently a lack of information regarding perioperative morbidity and mortality of patients with PHTN undergoing major head and neck procedures,” she said.
The researchers queried the National Inpatient Survey from 2002 to 2013 for all cases of major head and neck surgery based on the ICD-9 codes for esophagectomy, glossectomy, laryngectomy, mandibulectomy, and pharyngectomy. They divided patients into two groups: those who had PHTN and those who did not, and performed demographic analyses as well as univariate and multivariate regression analyses.
Ms. Patel reported findings from a cohort of 46,311 patients. Of these, 46,073 had PHTN and 238 did not. The two groups were similar in age (a mean of 69 vs. 60 years in those with and without PHTN, respectively) and race (80% white vs. 79% white, respectively), but there were significantly fewer male patients in the PHTN group (57% vs. 70%; P less than .0001).
Several patient comorbidities were increased in the PHTN group, compared with the non-PHTN group, including coagulopathy (8.4% vs. 3.1%; P less than .0001), chronic heart failure (22.4% vs. 4.1%; P less than .0001), complicated diabetes (4.6% vs. 1.2%; P less than .0001), fluid and electrolyte disorders (30% vs. 18.3%; P less than .0001), and hypertension (63.3% vs. 43.7%; P less than .0001).
Postoperatively, patients with PHTN had a longer length of stay (a mean of 15.80 vs. 11.50 days, respectively; P less than .0001) as well as significantly higher total charges (a mean of $162,021.06 vs. $107,309.46, respectively; P less than .0001). When the researchers evaluated postoperative outcomes between the two cohorts, patients with PHTN had significantly higher rates of cardiac complications (9.2% vs. 3.5%; P less than .0001), iatrogenic pulmonary embolism (2.1% vs. 0.3%; P = .001), pulmonary edema (2.1% vs. 0.4%; P = .003), venous thrombotic events (4.6% vs. 1%; P less than. 0001), pulmonary insufficiency (17.2% vs. 9.7%; P less than .0001), and pneumonia (9.7% vs. 6%; P = .027), as well as higher rates of postoperative tracheostomy (8.4% vs. 4.5%; P = .007).
Multivariate analysis revealed that the following factors predicted in-hospital mortality: coagulopathy, chronic heart failure, fluid and electrolyte disorders, hyperlipidemia, hypertension, hypothyroidism, liver disease, obesity, paralysis, and renal failure. Despite these findings, there was no significant change in overall hospital mortality for those with PHTN, with an odds ratio of 1.055.
“Our study is not without its limitations, many of which are inherent to the use of a database, which is subject to errors in coding and sampling,” Ms. Patel noted at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. “Despite these limitations, the study provides valuable information on the impact of PHTN on major head and neck procedures.
She reported having no financial disclosures.
SOURCE: Patel N et al. Triological CSM, Abstracts.
SAN DIEGO – Patients with , compared with their counterparts who do not have the condition. They also face an increase in total charges and length of stay.
The findings come from what is believed to be the first study of its kind to investigate the impact of pulmonary hypertension (PHTN) on major head and neck procedures. “PHTN is a common condition which affects the caliber of lung vasculature, with varied symptom presentation from shortness of breath to syncope, with an estimated prevalence of 2.5 to 7.1 million new cases each year worldwide,” one of the study authors, Nirali M. Patel, said at the Triological Society’s Combined Sections Meeting. “Due to improved therapeutic options, there is an enhanced survival of PHTN patients and higher prevalence of this disease. PHTN has some significant systemic implications. Therefore, cardiopulmonary clearance and a clear understanding of postoperative complications are very important.”
Previous studies have shown PHTN to be an independent predictor of morbidity and mortality in noncardiac procedures, said Ms. Patel, a fourth-year medical student at New Jersey Medical School, Newark. Furthermore, the rate of pulmonary complications is reported to be between 11% and 44.8% following radical head and neck cancer resection. “Despite these findings, there is currently a lack of information regarding perioperative morbidity and mortality of patients with PHTN undergoing major head and neck procedures,” she said.
The researchers queried the National Inpatient Survey from 2002 to 2013 for all cases of major head and neck surgery based on the ICD-9 codes for esophagectomy, glossectomy, laryngectomy, mandibulectomy, and pharyngectomy. They divided patients into two groups: those who had PHTN and those who did not, and performed demographic analyses as well as univariate and multivariate regression analyses.
Ms. Patel reported findings from a cohort of 46,311 patients. Of these, 46,073 had PHTN and 238 did not. The two groups were similar in age (a mean of 69 vs. 60 years in those with and without PHTN, respectively) and race (80% white vs. 79% white, respectively), but there were significantly fewer male patients in the PHTN group (57% vs. 70%; P less than .0001).
Several patient comorbidities were increased in the PHTN group, compared with the non-PHTN group, including coagulopathy (8.4% vs. 3.1%; P less than .0001), chronic heart failure (22.4% vs. 4.1%; P less than .0001), complicated diabetes (4.6% vs. 1.2%; P less than .0001), fluid and electrolyte disorders (30% vs. 18.3%; P less than .0001), and hypertension (63.3% vs. 43.7%; P less than .0001).
Postoperatively, patients with PHTN had a longer length of stay (a mean of 15.80 vs. 11.50 days, respectively; P less than .0001) as well as significantly higher total charges (a mean of $162,021.06 vs. $107,309.46, respectively; P less than .0001). When the researchers evaluated postoperative outcomes between the two cohorts, patients with PHTN had significantly higher rates of cardiac complications (9.2% vs. 3.5%; P less than .0001), iatrogenic pulmonary embolism (2.1% vs. 0.3%; P = .001), pulmonary edema (2.1% vs. 0.4%; P = .003), venous thrombotic events (4.6% vs. 1%; P less than. 0001), pulmonary insufficiency (17.2% vs. 9.7%; P less than .0001), and pneumonia (9.7% vs. 6%; P = .027), as well as higher rates of postoperative tracheostomy (8.4% vs. 4.5%; P = .007).
Multivariate analysis revealed that the following factors predicted in-hospital mortality: coagulopathy, chronic heart failure, fluid and electrolyte disorders, hyperlipidemia, hypertension, hypothyroidism, liver disease, obesity, paralysis, and renal failure. Despite these findings, there was no significant change in overall hospital mortality for those with PHTN, with an odds ratio of 1.055.
“Our study is not without its limitations, many of which are inherent to the use of a database, which is subject to errors in coding and sampling,” Ms. Patel noted at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. “Despite these limitations, the study provides valuable information on the impact of PHTN on major head and neck procedures.
She reported having no financial disclosures.
SOURCE: Patel N et al. Triological CSM, Abstracts.
SAN DIEGO – Patients with , compared with their counterparts who do not have the condition. They also face an increase in total charges and length of stay.
The findings come from what is believed to be the first study of its kind to investigate the impact of pulmonary hypertension (PHTN) on major head and neck procedures. “PHTN is a common condition which affects the caliber of lung vasculature, with varied symptom presentation from shortness of breath to syncope, with an estimated prevalence of 2.5 to 7.1 million new cases each year worldwide,” one of the study authors, Nirali M. Patel, said at the Triological Society’s Combined Sections Meeting. “Due to improved therapeutic options, there is an enhanced survival of PHTN patients and higher prevalence of this disease. PHTN has some significant systemic implications. Therefore, cardiopulmonary clearance and a clear understanding of postoperative complications are very important.”
Previous studies have shown PHTN to be an independent predictor of morbidity and mortality in noncardiac procedures, said Ms. Patel, a fourth-year medical student at New Jersey Medical School, Newark. Furthermore, the rate of pulmonary complications is reported to be between 11% and 44.8% following radical head and neck cancer resection. “Despite these findings, there is currently a lack of information regarding perioperative morbidity and mortality of patients with PHTN undergoing major head and neck procedures,” she said.
The researchers queried the National Inpatient Survey from 2002 to 2013 for all cases of major head and neck surgery based on the ICD-9 codes for esophagectomy, glossectomy, laryngectomy, mandibulectomy, and pharyngectomy. They divided patients into two groups: those who had PHTN and those who did not, and performed demographic analyses as well as univariate and multivariate regression analyses.
Ms. Patel reported findings from a cohort of 46,311 patients. Of these, 46,073 had PHTN and 238 did not. The two groups were similar in age (a mean of 69 vs. 60 years in those with and without PHTN, respectively) and race (80% white vs. 79% white, respectively), but there were significantly fewer male patients in the PHTN group (57% vs. 70%; P less than .0001).
Several patient comorbidities were increased in the PHTN group, compared with the non-PHTN group, including coagulopathy (8.4% vs. 3.1%; P less than .0001), chronic heart failure (22.4% vs. 4.1%; P less than .0001), complicated diabetes (4.6% vs. 1.2%; P less than .0001), fluid and electrolyte disorders (30% vs. 18.3%; P less than .0001), and hypertension (63.3% vs. 43.7%; P less than .0001).
Postoperatively, patients with PHTN had a longer length of stay (a mean of 15.80 vs. 11.50 days, respectively; P less than .0001) as well as significantly higher total charges (a mean of $162,021.06 vs. $107,309.46, respectively; P less than .0001). When the researchers evaluated postoperative outcomes between the two cohorts, patients with PHTN had significantly higher rates of cardiac complications (9.2% vs. 3.5%; P less than .0001), iatrogenic pulmonary embolism (2.1% vs. 0.3%; P = .001), pulmonary edema (2.1% vs. 0.4%; P = .003), venous thrombotic events (4.6% vs. 1%; P less than. 0001), pulmonary insufficiency (17.2% vs. 9.7%; P less than .0001), and pneumonia (9.7% vs. 6%; P = .027), as well as higher rates of postoperative tracheostomy (8.4% vs. 4.5%; P = .007).
Multivariate analysis revealed that the following factors predicted in-hospital mortality: coagulopathy, chronic heart failure, fluid and electrolyte disorders, hyperlipidemia, hypertension, hypothyroidism, liver disease, obesity, paralysis, and renal failure. Despite these findings, there was no significant change in overall hospital mortality for those with PHTN, with an odds ratio of 1.055.
“Our study is not without its limitations, many of which are inherent to the use of a database, which is subject to errors in coding and sampling,” Ms. Patel noted at the meeting, which was jointly sponsored by the Triological Society and the American College of Surgeons. “Despite these limitations, the study provides valuable information on the impact of PHTN on major head and neck procedures.
She reported having no financial disclosures.
SOURCE: Patel N et al. Triological CSM, Abstracts.
REPORTING FROM THE TRIOLOGICAL CSM
Key clinical point: Pulmonary hypertension (PHTN) is linked with certain head and neck surgical complications.
Major finding: For patients undergoing head and neck surgery, PHTN is associated with an increased risk of cardiac complications (9.2% vs. 3.5%) and iatrogenic pulmonary embolism (2.1% vs. 0.3%).
Study details: A retrospective analysis of 46,311 patient records from the National Inpatient Survey.
Disclosures: The researchers reported having no financial disclosures.
Source: Patel N et al. Triological CSM, Abstracts.





