User login
Our CHEST year
Greetings. I hope that you are well and are enjoying the summer as best you can during these challenging times. Since the “CHEST year” has drawn to a close recently, I would like to offer my reflections, which were recently shared with the Board of Regents, as well as a glimpse of what is ahead for CHEST. There is just so much great work I want to share.
This past year has posed a number of challenges. COVID-19 has caused us to interact differently on both a social and a business level. CHEST Headquarters has been closed, and we have not had a live-learning course for more than 4 months. But our work has not faltered. We have been extremely productive during this period and have once again demonstrated our resiliency and innovative spirit; in our vernacular, we “Crushed It.”
While COVID-19 has presented us with a number of obstacles, it has presented us with a number of opportunities, and we have taken advantage of them. During this pandemic, CHEST has truly demonstrated its ability to provide a connection at a critical time, giving this phrase new meaning and urgency. We have created a new resource center for clinicians, developed patient education and awareness campaigns to support the public through this crisis, launched a webinar series, developed scientific guidance statements, and more. At the same time, we have invested in our technology and educational infrastructure to grow our capabilities and position CHEST for long-term success.
Prior to COVID-19, we spent a significant amount of time among the CHEST staff, Presidents, and Boards drafting and reviewing a concise strategy statement for CHEST to provide focus and clarity to its efforts and derive and tie together future strategies specific to learning, technology, and more. From this statement, we derived four key areas requiring our continued and explicit focus to achieve this goal:
• People: Ensure we attract, retain, and incentivize the right people (staff, leaders, and volunteers).
• Products: Foster an environment of innovation and product development resulting in overall revenue growth, as well as revenue from new products and services.
• Education: Ensure that CHEST education products and services are robust, differentiated, and scalable..
• Growth: Meet or exceed revenue and margin targets.
As long as the mission and strategy of the organization does not deviate, these goals should not change. However, how we go about executing on achieving these goals each year will depend on the context of our environment and be shaped by the specific initiatives planned affecting our People, Products, Education, and building toward Growth. This consistency is important to sustain a vibrant, aligned, and productive organization.
Beyond this groundwork, I also would like to list a series of things that, together, CHEST accomplished over the last year.
- Reviewed existing contracts and, where appropriate, renegotiated major contracts to ensure terms more favorable for CHEST.
- Hired and on-boarded a Chief Learning Officer to place greater emphasis on expanding CHEST educational programs. Analyzed current educational products and have begun repositioning our educational efforts to better serve our learners.
- Refined the one CHEST concept, realigned responsibilities throughout the organization in general, and the CHEST Foundation, in particular, to enhance resource readiness and productivity. Clarified relationship with industry by continuing to implement our Industry Partnership Guidelines and streamline efforts with our partners.
- Continued rollout and execution of our international event strategy. Successfully developed and held a program for CHEST Congress 2020 Italy with our CHEST Italian Delegation, in a virtual format, due to COVID, while enabling us to build momentum for a rescheduled meeting in 2021. We had over 2,000 virtual registrants from over 100 countries, and there was a thank you given to all attendees by Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, to start off the program – what a success!
- Accelerated our digital transformation with an educational focus on virtual Board Review, CHEST 2020 Annual Meeting, online simulation.
- Forecasting strong financial outlook and improving financial reporting for FY19-20. Successful 2019 annual meeting:
o Total attendance 8,593—the largest attendance to date.
o Simulation Session Registration 979
o Exhibiting companies 160 SOLD OUT
o CHEST Annual Meeting 2019 delivered largest number of APPs and fellows attending in the last 5 years.
- Reintroduced CHEST into the advocacy and health policy arena through the successful acquisition of NAMDRC.
CHEST’s operating financial performance is solid, and well thought out efforts have kept CHEST on a growth trajectory over the last 7 years. During this same period (since 2011/12), our staff headcount has grown from 85 to a projected 121 this year; the new expertise and capabilities we have brought on board, combined with our highly talented and committed staff team, have contributed to this tremendous growth.
Our future is bright. These 2 two years have been very exciting for me both professionally and personally. I am grateful for the opportunity to work with all of you and serve as your CEO/EVP because together, we truly are making a significant difference in moving CHEST forward and crushing lung disease.
I know you are as proud of CHEST’s efforts this year as I am.
Thank you.
Greetings. I hope that you are well and are enjoying the summer as best you can during these challenging times. Since the “CHEST year” has drawn to a close recently, I would like to offer my reflections, which were recently shared with the Board of Regents, as well as a glimpse of what is ahead for CHEST. There is just so much great work I want to share.
This past year has posed a number of challenges. COVID-19 has caused us to interact differently on both a social and a business level. CHEST Headquarters has been closed, and we have not had a live-learning course for more than 4 months. But our work has not faltered. We have been extremely productive during this period and have once again demonstrated our resiliency and innovative spirit; in our vernacular, we “Crushed It.”
While COVID-19 has presented us with a number of obstacles, it has presented us with a number of opportunities, and we have taken advantage of them. During this pandemic, CHEST has truly demonstrated its ability to provide a connection at a critical time, giving this phrase new meaning and urgency. We have created a new resource center for clinicians, developed patient education and awareness campaigns to support the public through this crisis, launched a webinar series, developed scientific guidance statements, and more. At the same time, we have invested in our technology and educational infrastructure to grow our capabilities and position CHEST for long-term success.
Prior to COVID-19, we spent a significant amount of time among the CHEST staff, Presidents, and Boards drafting and reviewing a concise strategy statement for CHEST to provide focus and clarity to its efforts and derive and tie together future strategies specific to learning, technology, and more. From this statement, we derived four key areas requiring our continued and explicit focus to achieve this goal:
• People: Ensure we attract, retain, and incentivize the right people (staff, leaders, and volunteers).
• Products: Foster an environment of innovation and product development resulting in overall revenue growth, as well as revenue from new products and services.
• Education: Ensure that CHEST education products and services are robust, differentiated, and scalable..
• Growth: Meet or exceed revenue and margin targets.
As long as the mission and strategy of the organization does not deviate, these goals should not change. However, how we go about executing on achieving these goals each year will depend on the context of our environment and be shaped by the specific initiatives planned affecting our People, Products, Education, and building toward Growth. This consistency is important to sustain a vibrant, aligned, and productive organization.
Beyond this groundwork, I also would like to list a series of things that, together, CHEST accomplished over the last year.
- Reviewed existing contracts and, where appropriate, renegotiated major contracts to ensure terms more favorable for CHEST.
- Hired and on-boarded a Chief Learning Officer to place greater emphasis on expanding CHEST educational programs. Analyzed current educational products and have begun repositioning our educational efforts to better serve our learners.
- Refined the one CHEST concept, realigned responsibilities throughout the organization in general, and the CHEST Foundation, in particular, to enhance resource readiness and productivity. Clarified relationship with industry by continuing to implement our Industry Partnership Guidelines and streamline efforts with our partners.
- Continued rollout and execution of our international event strategy. Successfully developed and held a program for CHEST Congress 2020 Italy with our CHEST Italian Delegation, in a virtual format, due to COVID, while enabling us to build momentum for a rescheduled meeting in 2021. We had over 2,000 virtual registrants from over 100 countries, and there was a thank you given to all attendees by Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, to start off the program – what a success!
- Accelerated our digital transformation with an educational focus on virtual Board Review, CHEST 2020 Annual Meeting, online simulation.
- Forecasting strong financial outlook and improving financial reporting for FY19-20. Successful 2019 annual meeting:
o Total attendance 8,593—the largest attendance to date.
o Simulation Session Registration 979
o Exhibiting companies 160 SOLD OUT
o CHEST Annual Meeting 2019 delivered largest number of APPs and fellows attending in the last 5 years.
- Reintroduced CHEST into the advocacy and health policy arena through the successful acquisition of NAMDRC.
CHEST’s operating financial performance is solid, and well thought out efforts have kept CHEST on a growth trajectory over the last 7 years. During this same period (since 2011/12), our staff headcount has grown from 85 to a projected 121 this year; the new expertise and capabilities we have brought on board, combined with our highly talented and committed staff team, have contributed to this tremendous growth.
Our future is bright. These 2 two years have been very exciting for me both professionally and personally. I am grateful for the opportunity to work with all of you and serve as your CEO/EVP because together, we truly are making a significant difference in moving CHEST forward and crushing lung disease.
I know you are as proud of CHEST’s efforts this year as I am.
Thank you.
Greetings. I hope that you are well and are enjoying the summer as best you can during these challenging times. Since the “CHEST year” has drawn to a close recently, I would like to offer my reflections, which were recently shared with the Board of Regents, as well as a glimpse of what is ahead for CHEST. There is just so much great work I want to share.
This past year has posed a number of challenges. COVID-19 has caused us to interact differently on both a social and a business level. CHEST Headquarters has been closed, and we have not had a live-learning course for more than 4 months. But our work has not faltered. We have been extremely productive during this period and have once again demonstrated our resiliency and innovative spirit; in our vernacular, we “Crushed It.”
While COVID-19 has presented us with a number of obstacles, it has presented us with a number of opportunities, and we have taken advantage of them. During this pandemic, CHEST has truly demonstrated its ability to provide a connection at a critical time, giving this phrase new meaning and urgency. We have created a new resource center for clinicians, developed patient education and awareness campaigns to support the public through this crisis, launched a webinar series, developed scientific guidance statements, and more. At the same time, we have invested in our technology and educational infrastructure to grow our capabilities and position CHEST for long-term success.
Prior to COVID-19, we spent a significant amount of time among the CHEST staff, Presidents, and Boards drafting and reviewing a concise strategy statement for CHEST to provide focus and clarity to its efforts and derive and tie together future strategies specific to learning, technology, and more. From this statement, we derived four key areas requiring our continued and explicit focus to achieve this goal:
• People: Ensure we attract, retain, and incentivize the right people (staff, leaders, and volunteers).
• Products: Foster an environment of innovation and product development resulting in overall revenue growth, as well as revenue from new products and services.
• Education: Ensure that CHEST education products and services are robust, differentiated, and scalable..
• Growth: Meet or exceed revenue and margin targets.
As long as the mission and strategy of the organization does not deviate, these goals should not change. However, how we go about executing on achieving these goals each year will depend on the context of our environment and be shaped by the specific initiatives planned affecting our People, Products, Education, and building toward Growth. This consistency is important to sustain a vibrant, aligned, and productive organization.
Beyond this groundwork, I also would like to list a series of things that, together, CHEST accomplished over the last year.
- Reviewed existing contracts and, where appropriate, renegotiated major contracts to ensure terms more favorable for CHEST.
- Hired and on-boarded a Chief Learning Officer to place greater emphasis on expanding CHEST educational programs. Analyzed current educational products and have begun repositioning our educational efforts to better serve our learners.
- Refined the one CHEST concept, realigned responsibilities throughout the organization in general, and the CHEST Foundation, in particular, to enhance resource readiness and productivity. Clarified relationship with industry by continuing to implement our Industry Partnership Guidelines and streamline efforts with our partners.
- Continued rollout and execution of our international event strategy. Successfully developed and held a program for CHEST Congress 2020 Italy with our CHEST Italian Delegation, in a virtual format, due to COVID, while enabling us to build momentum for a rescheduled meeting in 2021. We had over 2,000 virtual registrants from over 100 countries, and there was a thank you given to all attendees by Dr. Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases, to start off the program – what a success!
- Accelerated our digital transformation with an educational focus on virtual Board Review, CHEST 2020 Annual Meeting, online simulation.
- Forecasting strong financial outlook and improving financial reporting for FY19-20. Successful 2019 annual meeting:
o Total attendance 8,593—the largest attendance to date.
o Simulation Session Registration 979
o Exhibiting companies 160 SOLD OUT
o CHEST Annual Meeting 2019 delivered largest number of APPs and fellows attending in the last 5 years.
- Reintroduced CHEST into the advocacy and health policy arena through the successful acquisition of NAMDRC.
CHEST’s operating financial performance is solid, and well thought out efforts have kept CHEST on a growth trajectory over the last 7 years. During this same period (since 2011/12), our staff headcount has grown from 85 to a projected 121 this year; the new expertise and capabilities we have brought on board, combined with our highly talented and committed staff team, have contributed to this tremendous growth.
Our future is bright. These 2 two years have been very exciting for me both professionally and personally. I am grateful for the opportunity to work with all of you and serve as your CEO/EVP because together, we truly are making a significant difference in moving CHEST forward and crushing lung disease.
I know you are as proud of CHEST’s efforts this year as I am.
Thank you.
President’s report
Dear Colleagues,
We are now near 6 months into living with COVID-19. In Texas, we are experiencing the surge that much of the Northeast saw in March and April. The COVID-19 Task Force led by Dr. Steve Simpson (CHEST President-Elect) and with representation from the Critical Care, Chest Infections, and Disaster Response and Global Health NetWorks continues to meet regularly to keep our members updated on the latest research and rapidly changing clinical management of COVID-19 illness and the sequelae. COVID-19 has put our medical profession and our subspecialty under considerable stress, and CHEST has launched a new longitudinal Wellness Center led by Dr. Alex Niven, from Mayo Clinic, Rochester. These new resources will feature a wellness webinar series focused on mental health and wellness for clinicians during COVID-19 and beyond. CHEST received overwhelming positive feedback from members and attendees to the Women & Pulmonary Virtual Happy Hour that focused on sharing stories and building community. Many leaders have suggested other such topics and efforts that may be useful to the CHEST community. The CHEST Wellness Center will launch on July 15.
In addition to COVID-19 activities, our nation and the world have compelled a new powerful look at race relations, disparities, and diversity. I represented CHEST at a “White Coats for Black Lives” event in San Antonio. Following our nation’s call for racial equality, CHEST released a Statement of Equity that received overwhelmingly positive feedback and response from members via email and on social media. This statement clearly resonated with the CHEST community. We are asking our leadership and members to consider ways in which CHEST might continue to raise awareness and continue with efforts related to diversity and equity. CHEST also hosted an excellent webinar moderated by Dr. Demondes Haynes and Dr. Nneka Sederstrom in late June that offered a direct and meaningful dialogue on issues facing clinicians and patients of color, and the responsibility of those in leadership positions. CHEST leadership stand firm that racism and inequality are public health issues and are working to define how we further our efforts in this arena.
On June 17, CHEST held a 1-day Virtual CHEST Congress in conjunction with our the CHEST Italian Delegation, as COVID-19 prevented us from safely holding the live Congress in Bologna. We had 3,250 registered attendees. I was so impressed at what a virtual platform can deliver, complete with great educational sessions, including much on COVID-19, as well as capturing the CHEST experience with games, bocce, jeopardy etc! This gave CHEST an opportunity to explore further virtual-based education to reach our wider global audience. CHEST will still be holding an in-person Congress in Bologna, June 24-26, 2021.
CHEST will host three entirely virtual Board Review Courses this August in the areas of Pulmonary, Critical Care, and Pediatric Pulmonary Medicine. These courses will include a combination of pre-recorded lectures and live, interactive sessions. Audience response systems and SEEK questions will still be utilized. There’s still time to register, so don’t miss it! With time being a major commodity at present, all attendees will receive year-long access to all material!
I know you have been wondering about CHEST 2020, and as you have heard by now, CHEST 2020 in Chicago will be a virtual meeting. I am sure that this announcement came as no big surprise, but is certainly disappointing. As you can imagine this was a difficult decision, but one that was necessary based upon our new reality. It was compounded by limitations on the convention center venue under the Illinois reopening plan, and the fact that a large number of our faculty, as well as our attendees, are under a travel ban for the remainder of 2020 that will not allow them to travel to Chicago. The abstract and case report deadline closed June 1, and despite these circumstances, we saw our highest number of submissions to date! Late abstracts were due on July 17. We will be presenting standalone and complementary online offerings to ensure seamless delivery of critical education in formats that cater easily to our newly formed habits.
Thanks to our dedicated Scientific Program Committee Chair, Dr. Victor Test, and staff, we had already begun preparing for virtual CHEST Annual Meeting 2020. Here’s what you can expect:
• A memorable experience
• A highly interactive education program that includes audience Q&A, discussion threads, and audience response systems
• Opportunities for one-on-one discussions, networking, and access to faculty
• Industry-sponsored programs and a virtual exhibit hall
• Access to hundreds of narrated poster presentations, case reports, and research abstracts
• Competitive educational gaming where attendees can participate, win, or watch
• Dedicated COVID-19 update sessions
• CME and MOC credits
If you have already registered for CHEST 2020, you will have the option to transfer your registration to this new model. Our main focus is delivering the virtual program with the highest level of service that you have come to expect from CHEST and respect for our member’s time and current situation. I know Dr. Victor Test and the program committee will deliver a superb educational experience in a virtual meeting setting. Thank you for your support and understanding as we continue to evolve our events to meet the needs of our members while adapting to the best delivery methods.
Since so many fellows were unable to hold their live graduation events, and celebrations, we decided to send them off with a virtual event! On June 30 we held a Joint CHEST/ATS Respiratory Community Graduation Ceremony–for graduating fellows, and to welcome new fellows to our profession. The ceremony consisted of a combination of live and recorded messages from key leaders from both organizations. In addition, there was a keynote address from Dr. Rana Awdish, a critical care physician at Henry Ford Hospital in Detroit, who authored the bestselling book “In Shock: My Journey from Death to Recovery and the Redemptive Power of Hope.” I encourage you to watch the video on the Early Career Professionals page on our Chestnet.org website.
The National Association for Medical Direction of Respiratory Care (NAMDRC) merger with CHEST was finalized at the end of May. Look for more advocacy-related actions coming from CHEST. The newly formed Health Policy and Advocacy Committee is helping to set CHEST’s advocacy agendas in the legislative and regulatory arenas, engaging with policymakers and educating CHEST members on governmental affairs relevant to CHEST’s mission. Did you see the inaugural CHEST published, on-line issue of Washington Watchline, a newsletter that aims to keep CHEST members informed about governmental activities that affect physicians who provide clinical care in respiratory, critical care, and sleep medicine? Follow Washington Watchline to learn more about CHEST’s advocacy around regulatory, legislative, and payment issues that relate to the delivery of health care in support of CHEST’s mission. One of the features was Telemedicine, which many of us are now using and is likely to be a part of many of our practices going forward.
With new COVID-19 surges throughout many parts of the United States, CHEST has continued our volunteer matching program for areas of need, including to the Navaho Nations, where CHEST matched 20 volunteers and has had more than a half-dozen inquiries from our members. In addition, in conjunction with the Foundation, CHEST has partnered with American Mask Rally and started a campaign to distribute masks to frontline essential workers in underserved communities. CHEST received a generous donation from AstraZeneca and Glaxo Smith Kline to help in the global fight against COVID-19 to provide current and accurate information and education to frontline clinicians to allow them to provide the best patient outcomes. CHEST also partnered with the American Thoracic Society to launch a joint PSA/ media campaign entitled For My Lung Health Campaign, to provide credible resources for underserved Black and Latino communities, as these communities are disproportionally affected by COVID-19. At the time of this writing, over a million people have seen the related video, featuring tips for taking control of one’s health in these difficult and uncertain times.
So, in closing, thank you all for what you do in these challenging times. 2020 will certainly be a year to remember! Stay safe and stay well!
Stephanie
Dear Colleagues,
We are now near 6 months into living with COVID-19. In Texas, we are experiencing the surge that much of the Northeast saw in March and April. The COVID-19 Task Force led by Dr. Steve Simpson (CHEST President-Elect) and with representation from the Critical Care, Chest Infections, and Disaster Response and Global Health NetWorks continues to meet regularly to keep our members updated on the latest research and rapidly changing clinical management of COVID-19 illness and the sequelae. COVID-19 has put our medical profession and our subspecialty under considerable stress, and CHEST has launched a new longitudinal Wellness Center led by Dr. Alex Niven, from Mayo Clinic, Rochester. These new resources will feature a wellness webinar series focused on mental health and wellness for clinicians during COVID-19 and beyond. CHEST received overwhelming positive feedback from members and attendees to the Women & Pulmonary Virtual Happy Hour that focused on sharing stories and building community. Many leaders have suggested other such topics and efforts that may be useful to the CHEST community. The CHEST Wellness Center will launch on July 15.
In addition to COVID-19 activities, our nation and the world have compelled a new powerful look at race relations, disparities, and diversity. I represented CHEST at a “White Coats for Black Lives” event in San Antonio. Following our nation’s call for racial equality, CHEST released a Statement of Equity that received overwhelmingly positive feedback and response from members via email and on social media. This statement clearly resonated with the CHEST community. We are asking our leadership and members to consider ways in which CHEST might continue to raise awareness and continue with efforts related to diversity and equity. CHEST also hosted an excellent webinar moderated by Dr. Demondes Haynes and Dr. Nneka Sederstrom in late June that offered a direct and meaningful dialogue on issues facing clinicians and patients of color, and the responsibility of those in leadership positions. CHEST leadership stand firm that racism and inequality are public health issues and are working to define how we further our efforts in this arena.
On June 17, CHEST held a 1-day Virtual CHEST Congress in conjunction with our the CHEST Italian Delegation, as COVID-19 prevented us from safely holding the live Congress in Bologna. We had 3,250 registered attendees. I was so impressed at what a virtual platform can deliver, complete with great educational sessions, including much on COVID-19, as well as capturing the CHEST experience with games, bocce, jeopardy etc! This gave CHEST an opportunity to explore further virtual-based education to reach our wider global audience. CHEST will still be holding an in-person Congress in Bologna, June 24-26, 2021.
CHEST will host three entirely virtual Board Review Courses this August in the areas of Pulmonary, Critical Care, and Pediatric Pulmonary Medicine. These courses will include a combination of pre-recorded lectures and live, interactive sessions. Audience response systems and SEEK questions will still be utilized. There’s still time to register, so don’t miss it! With time being a major commodity at present, all attendees will receive year-long access to all material!
I know you have been wondering about CHEST 2020, and as you have heard by now, CHEST 2020 in Chicago will be a virtual meeting. I am sure that this announcement came as no big surprise, but is certainly disappointing. As you can imagine this was a difficult decision, but one that was necessary based upon our new reality. It was compounded by limitations on the convention center venue under the Illinois reopening plan, and the fact that a large number of our faculty, as well as our attendees, are under a travel ban for the remainder of 2020 that will not allow them to travel to Chicago. The abstract and case report deadline closed June 1, and despite these circumstances, we saw our highest number of submissions to date! Late abstracts were due on July 17. We will be presenting standalone and complementary online offerings to ensure seamless delivery of critical education in formats that cater easily to our newly formed habits.
Thanks to our dedicated Scientific Program Committee Chair, Dr. Victor Test, and staff, we had already begun preparing for virtual CHEST Annual Meeting 2020. Here’s what you can expect:
• A memorable experience
• A highly interactive education program that includes audience Q&A, discussion threads, and audience response systems
• Opportunities for one-on-one discussions, networking, and access to faculty
• Industry-sponsored programs and a virtual exhibit hall
• Access to hundreds of narrated poster presentations, case reports, and research abstracts
• Competitive educational gaming where attendees can participate, win, or watch
• Dedicated COVID-19 update sessions
• CME and MOC credits
If you have already registered for CHEST 2020, you will have the option to transfer your registration to this new model. Our main focus is delivering the virtual program with the highest level of service that you have come to expect from CHEST and respect for our member’s time and current situation. I know Dr. Victor Test and the program committee will deliver a superb educational experience in a virtual meeting setting. Thank you for your support and understanding as we continue to evolve our events to meet the needs of our members while adapting to the best delivery methods.
Since so many fellows were unable to hold their live graduation events, and celebrations, we decided to send them off with a virtual event! On June 30 we held a Joint CHEST/ATS Respiratory Community Graduation Ceremony–for graduating fellows, and to welcome new fellows to our profession. The ceremony consisted of a combination of live and recorded messages from key leaders from both organizations. In addition, there was a keynote address from Dr. Rana Awdish, a critical care physician at Henry Ford Hospital in Detroit, who authored the bestselling book “In Shock: My Journey from Death to Recovery and the Redemptive Power of Hope.” I encourage you to watch the video on the Early Career Professionals page on our Chestnet.org website.
The National Association for Medical Direction of Respiratory Care (NAMDRC) merger with CHEST was finalized at the end of May. Look for more advocacy-related actions coming from CHEST. The newly formed Health Policy and Advocacy Committee is helping to set CHEST’s advocacy agendas in the legislative and regulatory arenas, engaging with policymakers and educating CHEST members on governmental affairs relevant to CHEST’s mission. Did you see the inaugural CHEST published, on-line issue of Washington Watchline, a newsletter that aims to keep CHEST members informed about governmental activities that affect physicians who provide clinical care in respiratory, critical care, and sleep medicine? Follow Washington Watchline to learn more about CHEST’s advocacy around regulatory, legislative, and payment issues that relate to the delivery of health care in support of CHEST’s mission. One of the features was Telemedicine, which many of us are now using and is likely to be a part of many of our practices going forward.
With new COVID-19 surges throughout many parts of the United States, CHEST has continued our volunteer matching program for areas of need, including to the Navaho Nations, where CHEST matched 20 volunteers and has had more than a half-dozen inquiries from our members. In addition, in conjunction with the Foundation, CHEST has partnered with American Mask Rally and started a campaign to distribute masks to frontline essential workers in underserved communities. CHEST received a generous donation from AstraZeneca and Glaxo Smith Kline to help in the global fight against COVID-19 to provide current and accurate information and education to frontline clinicians to allow them to provide the best patient outcomes. CHEST also partnered with the American Thoracic Society to launch a joint PSA/ media campaign entitled For My Lung Health Campaign, to provide credible resources for underserved Black and Latino communities, as these communities are disproportionally affected by COVID-19. At the time of this writing, over a million people have seen the related video, featuring tips for taking control of one’s health in these difficult and uncertain times.
So, in closing, thank you all for what you do in these challenging times. 2020 will certainly be a year to remember! Stay safe and stay well!
Stephanie
Dear Colleagues,
We are now near 6 months into living with COVID-19. In Texas, we are experiencing the surge that much of the Northeast saw in March and April. The COVID-19 Task Force led by Dr. Steve Simpson (CHEST President-Elect) and with representation from the Critical Care, Chest Infections, and Disaster Response and Global Health NetWorks continues to meet regularly to keep our members updated on the latest research and rapidly changing clinical management of COVID-19 illness and the sequelae. COVID-19 has put our medical profession and our subspecialty under considerable stress, and CHEST has launched a new longitudinal Wellness Center led by Dr. Alex Niven, from Mayo Clinic, Rochester. These new resources will feature a wellness webinar series focused on mental health and wellness for clinicians during COVID-19 and beyond. CHEST received overwhelming positive feedback from members and attendees to the Women & Pulmonary Virtual Happy Hour that focused on sharing stories and building community. Many leaders have suggested other such topics and efforts that may be useful to the CHEST community. The CHEST Wellness Center will launch on July 15.
In addition to COVID-19 activities, our nation and the world have compelled a new powerful look at race relations, disparities, and diversity. I represented CHEST at a “White Coats for Black Lives” event in San Antonio. Following our nation’s call for racial equality, CHEST released a Statement of Equity that received overwhelmingly positive feedback and response from members via email and on social media. This statement clearly resonated with the CHEST community. We are asking our leadership and members to consider ways in which CHEST might continue to raise awareness and continue with efforts related to diversity and equity. CHEST also hosted an excellent webinar moderated by Dr. Demondes Haynes and Dr. Nneka Sederstrom in late June that offered a direct and meaningful dialogue on issues facing clinicians and patients of color, and the responsibility of those in leadership positions. CHEST leadership stand firm that racism and inequality are public health issues and are working to define how we further our efforts in this arena.
On June 17, CHEST held a 1-day Virtual CHEST Congress in conjunction with our the CHEST Italian Delegation, as COVID-19 prevented us from safely holding the live Congress in Bologna. We had 3,250 registered attendees. I was so impressed at what a virtual platform can deliver, complete with great educational sessions, including much on COVID-19, as well as capturing the CHEST experience with games, bocce, jeopardy etc! This gave CHEST an opportunity to explore further virtual-based education to reach our wider global audience. CHEST will still be holding an in-person Congress in Bologna, June 24-26, 2021.
CHEST will host three entirely virtual Board Review Courses this August in the areas of Pulmonary, Critical Care, and Pediatric Pulmonary Medicine. These courses will include a combination of pre-recorded lectures and live, interactive sessions. Audience response systems and SEEK questions will still be utilized. There’s still time to register, so don’t miss it! With time being a major commodity at present, all attendees will receive year-long access to all material!
I know you have been wondering about CHEST 2020, and as you have heard by now, CHEST 2020 in Chicago will be a virtual meeting. I am sure that this announcement came as no big surprise, but is certainly disappointing. As you can imagine this was a difficult decision, but one that was necessary based upon our new reality. It was compounded by limitations on the convention center venue under the Illinois reopening plan, and the fact that a large number of our faculty, as well as our attendees, are under a travel ban for the remainder of 2020 that will not allow them to travel to Chicago. The abstract and case report deadline closed June 1, and despite these circumstances, we saw our highest number of submissions to date! Late abstracts were due on July 17. We will be presenting standalone and complementary online offerings to ensure seamless delivery of critical education in formats that cater easily to our newly formed habits.
Thanks to our dedicated Scientific Program Committee Chair, Dr. Victor Test, and staff, we had already begun preparing for virtual CHEST Annual Meeting 2020. Here’s what you can expect:
• A memorable experience
• A highly interactive education program that includes audience Q&A, discussion threads, and audience response systems
• Opportunities for one-on-one discussions, networking, and access to faculty
• Industry-sponsored programs and a virtual exhibit hall
• Access to hundreds of narrated poster presentations, case reports, and research abstracts
• Competitive educational gaming where attendees can participate, win, or watch
• Dedicated COVID-19 update sessions
• CME and MOC credits
If you have already registered for CHEST 2020, you will have the option to transfer your registration to this new model. Our main focus is delivering the virtual program with the highest level of service that you have come to expect from CHEST and respect for our member’s time and current situation. I know Dr. Victor Test and the program committee will deliver a superb educational experience in a virtual meeting setting. Thank you for your support and understanding as we continue to evolve our events to meet the needs of our members while adapting to the best delivery methods.
Since so many fellows were unable to hold their live graduation events, and celebrations, we decided to send them off with a virtual event! On June 30 we held a Joint CHEST/ATS Respiratory Community Graduation Ceremony–for graduating fellows, and to welcome new fellows to our profession. The ceremony consisted of a combination of live and recorded messages from key leaders from both organizations. In addition, there was a keynote address from Dr. Rana Awdish, a critical care physician at Henry Ford Hospital in Detroit, who authored the bestselling book “In Shock: My Journey from Death to Recovery and the Redemptive Power of Hope.” I encourage you to watch the video on the Early Career Professionals page on our Chestnet.org website.
The National Association for Medical Direction of Respiratory Care (NAMDRC) merger with CHEST was finalized at the end of May. Look for more advocacy-related actions coming from CHEST. The newly formed Health Policy and Advocacy Committee is helping to set CHEST’s advocacy agendas in the legislative and regulatory arenas, engaging with policymakers and educating CHEST members on governmental affairs relevant to CHEST’s mission. Did you see the inaugural CHEST published, on-line issue of Washington Watchline, a newsletter that aims to keep CHEST members informed about governmental activities that affect physicians who provide clinical care in respiratory, critical care, and sleep medicine? Follow Washington Watchline to learn more about CHEST’s advocacy around regulatory, legislative, and payment issues that relate to the delivery of health care in support of CHEST’s mission. One of the features was Telemedicine, which many of us are now using and is likely to be a part of many of our practices going forward.
With new COVID-19 surges throughout many parts of the United States, CHEST has continued our volunteer matching program for areas of need, including to the Navaho Nations, where CHEST matched 20 volunteers and has had more than a half-dozen inquiries from our members. In addition, in conjunction with the Foundation, CHEST has partnered with American Mask Rally and started a campaign to distribute masks to frontline essential workers in underserved communities. CHEST received a generous donation from AstraZeneca and Glaxo Smith Kline to help in the global fight against COVID-19 to provide current and accurate information and education to frontline clinicians to allow them to provide the best patient outcomes. CHEST also partnered with the American Thoracic Society to launch a joint PSA/ media campaign entitled For My Lung Health Campaign, to provide credible resources for underserved Black and Latino communities, as these communities are disproportionally affected by COVID-19. At the time of this writing, over a million people have seen the related video, featuring tips for taking control of one’s health in these difficult and uncertain times.
So, in closing, thank you all for what you do in these challenging times. 2020 will certainly be a year to remember! Stay safe and stay well!
Stephanie
Socioeconomic status key factor in CPAP adherence in older adults
The benefits of continuous positive airway pressure therapy for patients with obstructive sleep apnea are well documented, but it only works if patients can adhere to the therapy.
A large national study of older Medicare patients with obstructive sleep apnea (OSA) has identified lower socioeconomic status and comorbidities as independent risk factors for nonadherence to continuous positive airway pressure (CPAP) therapy.
“[The] present results represent the largest study to date of rates and predictors of CPAP adherence among older adults in the United States. In our national sample of Medicare beneficiaries, adherence rates were generally lower than previously reported in smaller, clinic-based studies,” Emerson M. Wickwire, PhD, of the Sleep Disorders Center and division of pulmonary and critical care medicine at the University of Maryland, Baltimore, and colleagues wrote in Sleep.
Dr. Wickwire and colleagues estimated CPAP machine adherence using a 5% sample of Medicare claims data, identifying 3,229 Medicare beneficiaries with OSA who began CPAP therapy between 2009 and 2011. Individuals in the sample were aged at least 65 years with a new diagnosis of OSA, 88.1% of beneficiaries were white, and 52.3% were male.
The researchers applied objective adherence criteria set by the Centers for Medicare & Medicaid Services, which defines CPAP adherence as a patient using CPAP for at least 4 hours on 70% of nights, or CPAP use for 21 of 30 consecutive days within 90 days after beginning therapy.
Using CPAP machine charges as a measure of who adhered to therapy, they found 1,420 of 3,229 individuals (44%) achieved adherence under these criteria, which included making 13 monthly payments during their CPAP machine’s “rent-to-own” period. Partial adherence was found in 997 individuals (30.9%) who made between 4-12 payments on their CPAP machine, while 812 individuals (25.2%) made 4 payments or fewer on their CPAP machines, which the researchers classified as nonadherence. Nonadherers tended to be slightly younger (mean, 72.5 years vs. 79.2 years; P < .001) and had a higher number of comorbidities (35.2% vs. 30.4%; P = .002), compared with individuals with high adherence. Anxiety (odds ratio, 1.34; 95% confidence interval, 1.12-1.61), anemia (OR, 1.16; 95% CI, 1.02-1.32), fibromyalgia (OR, 1.19; 95% CI, 1.03-1.38), traumatic brain injury (OR, 1.58; 95% CI, 1.21-2.07), and Medicaid eligibility (OR, 1.48; 95% CI, 1.24-1.75) were all independently associated with lower CPAP adherence. Medicaid eligibility was considered an indicator of lower socioeconomic status.
Krishna M. Sundar, MD, FCCP, director at the Sleep-Wake Center in the University of Utah pulmonary division in Salt Lake City and CHEST Physician editorial board member, said in an interview that studies have shown early signs of adherence within the first few weeks are an important indicator of overall adherence to CPAP therapy. However, the use of CPAP machine payments in the study by Dr. Wickwire and colleagues was a novel way to track adherence.
Some of the issues with nonadherence may be related to challenges in using the technology, but it is the clinician’s role to communicate with patients about the effectiveness of CPAP and identifying reasons for nonadherence while also attempting to tease out the subtle socioeconomic factors related to nonadherence, Dr. Sundar noted. “We need to alter our practice to make sure that we communicate with these patients and better understand what are the social factors in getting the CPAP or utilizing CPAP, and also following these patients more closely, especially in the first month of starting CPAP therapy.
“Just because somebody has severe sleep apnea and other comorbid conditions does not mean that they’re going to wear the CPAP,” he said. “So, the fact that socioeconomic factors play an equal if not more important role in terms of predicting CPAP adherence. That is an important takeaway.”
Octavian C. Ioachimescu, MD, FCCP, of Emory University, Atlanta, and the Atlanta Veteran Affairs Administration and CHEST Physician editorial board member, said in an interview that the study raises a major question of what is next. “What can we offer to these patients, and what is the real-world compliance to that ‘next-best’ modality?” Dr. Ioachimescu said. “What are the outcomes of these individuals in the point-of-care environment, or ‘real world?’ ”
The analysis by the authors adds the perspective of a “real-world depiction of clinical care for patients with OSA,” Dr. Ioachimescu said. “One major lesson of such an analysis is that the health care goal setting that is referential to initial, randomized, well-controlled studies on highly selected patient populations need to be reassessed periodically from the point of view of actual results in the clinics.”
Clinicians may need to borrow ideas from other therapeutic fields to help improve patient adherence, he said. “[W]e may be able to develop and implement in the future peer involvement, behavioral and cognitive approaches, motivational enhancement interventions, as well as elements of acceptance and commitment techniques, all in the larger context of more integrated and in the same time individualized approaches to therapy.”
The investigators concluded that, “relative to Medicare-only beneficiaries, those eligible for both Medicare and Medicaid were significantly less likely to adhere to CPAP. Future research should seek to develop a deeper understanding of the mechanisms through which [socioeconomic status] and other social determinants impact patient experience throughout the OSA diagnostic and treatment process, including receiving, acclimating, and adhering to CPAP therapy.”
Dr. Sundar concurred with this assessment and said more research is needed on factors impacting adherence such as poverty, homelessness, and home support systems. “It’s not just coordinating with the patient. Clearly, more work is needed in understanding the social aspects of CPAP adherence.”
This study was funded in part by an investigator-initiated grant provided by ResMed to Dr. Wickmire’s institution, the University of Maryland, Baltimore. Dr. Wickmire reported being a scientific consultant to DayZz, Eisai, Merck, and Purdue and holds shares in WellTap. Dr. Oldstone is a ResMed employee and shareholder. Dr. Sundar reported being a cofounder of Hypnoscure, which creates software for population management of sleep apnea, and an investigator in trials where ResMed and Respironics devices were used. Dr. Ioachimescu reported no relevant financial disclosures.
SOURCE: Wickwire EM et al. Sleep. 2020 Jun 23. doi: 10.1093/sleep/zsaa122.
The benefits of continuous positive airway pressure therapy for patients with obstructive sleep apnea are well documented, but it only works if patients can adhere to the therapy.
A large national study of older Medicare patients with obstructive sleep apnea (OSA) has identified lower socioeconomic status and comorbidities as independent risk factors for nonadherence to continuous positive airway pressure (CPAP) therapy.
“[The] present results represent the largest study to date of rates and predictors of CPAP adherence among older adults in the United States. In our national sample of Medicare beneficiaries, adherence rates were generally lower than previously reported in smaller, clinic-based studies,” Emerson M. Wickwire, PhD, of the Sleep Disorders Center and division of pulmonary and critical care medicine at the University of Maryland, Baltimore, and colleagues wrote in Sleep.
Dr. Wickwire and colleagues estimated CPAP machine adherence using a 5% sample of Medicare claims data, identifying 3,229 Medicare beneficiaries with OSA who began CPAP therapy between 2009 and 2011. Individuals in the sample were aged at least 65 years with a new diagnosis of OSA, 88.1% of beneficiaries were white, and 52.3% were male.
The researchers applied objective adherence criteria set by the Centers for Medicare & Medicaid Services, which defines CPAP adherence as a patient using CPAP for at least 4 hours on 70% of nights, or CPAP use for 21 of 30 consecutive days within 90 days after beginning therapy.
Using CPAP machine charges as a measure of who adhered to therapy, they found 1,420 of 3,229 individuals (44%) achieved adherence under these criteria, which included making 13 monthly payments during their CPAP machine’s “rent-to-own” period. Partial adherence was found in 997 individuals (30.9%) who made between 4-12 payments on their CPAP machine, while 812 individuals (25.2%) made 4 payments or fewer on their CPAP machines, which the researchers classified as nonadherence. Nonadherers tended to be slightly younger (mean, 72.5 years vs. 79.2 years; P < .001) and had a higher number of comorbidities (35.2% vs. 30.4%; P = .002), compared with individuals with high adherence. Anxiety (odds ratio, 1.34; 95% confidence interval, 1.12-1.61), anemia (OR, 1.16; 95% CI, 1.02-1.32), fibromyalgia (OR, 1.19; 95% CI, 1.03-1.38), traumatic brain injury (OR, 1.58; 95% CI, 1.21-2.07), and Medicaid eligibility (OR, 1.48; 95% CI, 1.24-1.75) were all independently associated with lower CPAP adherence. Medicaid eligibility was considered an indicator of lower socioeconomic status.
Krishna M. Sundar, MD, FCCP, director at the Sleep-Wake Center in the University of Utah pulmonary division in Salt Lake City and CHEST Physician editorial board member, said in an interview that studies have shown early signs of adherence within the first few weeks are an important indicator of overall adherence to CPAP therapy. However, the use of CPAP machine payments in the study by Dr. Wickwire and colleagues was a novel way to track adherence.
Some of the issues with nonadherence may be related to challenges in using the technology, but it is the clinician’s role to communicate with patients about the effectiveness of CPAP and identifying reasons for nonadherence while also attempting to tease out the subtle socioeconomic factors related to nonadherence, Dr. Sundar noted. “We need to alter our practice to make sure that we communicate with these patients and better understand what are the social factors in getting the CPAP or utilizing CPAP, and also following these patients more closely, especially in the first month of starting CPAP therapy.
“Just because somebody has severe sleep apnea and other comorbid conditions does not mean that they’re going to wear the CPAP,” he said. “So, the fact that socioeconomic factors play an equal if not more important role in terms of predicting CPAP adherence. That is an important takeaway.”
Octavian C. Ioachimescu, MD, FCCP, of Emory University, Atlanta, and the Atlanta Veteran Affairs Administration and CHEST Physician editorial board member, said in an interview that the study raises a major question of what is next. “What can we offer to these patients, and what is the real-world compliance to that ‘next-best’ modality?” Dr. Ioachimescu said. “What are the outcomes of these individuals in the point-of-care environment, or ‘real world?’ ”
The analysis by the authors adds the perspective of a “real-world depiction of clinical care for patients with OSA,” Dr. Ioachimescu said. “One major lesson of such an analysis is that the health care goal setting that is referential to initial, randomized, well-controlled studies on highly selected patient populations need to be reassessed periodically from the point of view of actual results in the clinics.”
Clinicians may need to borrow ideas from other therapeutic fields to help improve patient adherence, he said. “[W]e may be able to develop and implement in the future peer involvement, behavioral and cognitive approaches, motivational enhancement interventions, as well as elements of acceptance and commitment techniques, all in the larger context of more integrated and in the same time individualized approaches to therapy.”
The investigators concluded that, “relative to Medicare-only beneficiaries, those eligible for both Medicare and Medicaid were significantly less likely to adhere to CPAP. Future research should seek to develop a deeper understanding of the mechanisms through which [socioeconomic status] and other social determinants impact patient experience throughout the OSA diagnostic and treatment process, including receiving, acclimating, and adhering to CPAP therapy.”
Dr. Sundar concurred with this assessment and said more research is needed on factors impacting adherence such as poverty, homelessness, and home support systems. “It’s not just coordinating with the patient. Clearly, more work is needed in understanding the social aspects of CPAP adherence.”
This study was funded in part by an investigator-initiated grant provided by ResMed to Dr. Wickmire’s institution, the University of Maryland, Baltimore. Dr. Wickmire reported being a scientific consultant to DayZz, Eisai, Merck, and Purdue and holds shares in WellTap. Dr. Oldstone is a ResMed employee and shareholder. Dr. Sundar reported being a cofounder of Hypnoscure, which creates software for population management of sleep apnea, and an investigator in trials where ResMed and Respironics devices were used. Dr. Ioachimescu reported no relevant financial disclosures.
SOURCE: Wickwire EM et al. Sleep. 2020 Jun 23. doi: 10.1093/sleep/zsaa122.
The benefits of continuous positive airway pressure therapy for patients with obstructive sleep apnea are well documented, but it only works if patients can adhere to the therapy.
A large national study of older Medicare patients with obstructive sleep apnea (OSA) has identified lower socioeconomic status and comorbidities as independent risk factors for nonadherence to continuous positive airway pressure (CPAP) therapy.
“[The] present results represent the largest study to date of rates and predictors of CPAP adherence among older adults in the United States. In our national sample of Medicare beneficiaries, adherence rates were generally lower than previously reported in smaller, clinic-based studies,” Emerson M. Wickwire, PhD, of the Sleep Disorders Center and division of pulmonary and critical care medicine at the University of Maryland, Baltimore, and colleagues wrote in Sleep.
Dr. Wickwire and colleagues estimated CPAP machine adherence using a 5% sample of Medicare claims data, identifying 3,229 Medicare beneficiaries with OSA who began CPAP therapy between 2009 and 2011. Individuals in the sample were aged at least 65 years with a new diagnosis of OSA, 88.1% of beneficiaries were white, and 52.3% were male.
The researchers applied objective adherence criteria set by the Centers for Medicare & Medicaid Services, which defines CPAP adherence as a patient using CPAP for at least 4 hours on 70% of nights, or CPAP use for 21 of 30 consecutive days within 90 days after beginning therapy.
Using CPAP machine charges as a measure of who adhered to therapy, they found 1,420 of 3,229 individuals (44%) achieved adherence under these criteria, which included making 13 monthly payments during their CPAP machine’s “rent-to-own” period. Partial adherence was found in 997 individuals (30.9%) who made between 4-12 payments on their CPAP machine, while 812 individuals (25.2%) made 4 payments or fewer on their CPAP machines, which the researchers classified as nonadherence. Nonadherers tended to be slightly younger (mean, 72.5 years vs. 79.2 years; P < .001) and had a higher number of comorbidities (35.2% vs. 30.4%; P = .002), compared with individuals with high adherence. Anxiety (odds ratio, 1.34; 95% confidence interval, 1.12-1.61), anemia (OR, 1.16; 95% CI, 1.02-1.32), fibromyalgia (OR, 1.19; 95% CI, 1.03-1.38), traumatic brain injury (OR, 1.58; 95% CI, 1.21-2.07), and Medicaid eligibility (OR, 1.48; 95% CI, 1.24-1.75) were all independently associated with lower CPAP adherence. Medicaid eligibility was considered an indicator of lower socioeconomic status.
Krishna M. Sundar, MD, FCCP, director at the Sleep-Wake Center in the University of Utah pulmonary division in Salt Lake City and CHEST Physician editorial board member, said in an interview that studies have shown early signs of adherence within the first few weeks are an important indicator of overall adherence to CPAP therapy. However, the use of CPAP machine payments in the study by Dr. Wickwire and colleagues was a novel way to track adherence.
Some of the issues with nonadherence may be related to challenges in using the technology, but it is the clinician’s role to communicate with patients about the effectiveness of CPAP and identifying reasons for nonadherence while also attempting to tease out the subtle socioeconomic factors related to nonadherence, Dr. Sundar noted. “We need to alter our practice to make sure that we communicate with these patients and better understand what are the social factors in getting the CPAP or utilizing CPAP, and also following these patients more closely, especially in the first month of starting CPAP therapy.
“Just because somebody has severe sleep apnea and other comorbid conditions does not mean that they’re going to wear the CPAP,” he said. “So, the fact that socioeconomic factors play an equal if not more important role in terms of predicting CPAP adherence. That is an important takeaway.”
Octavian C. Ioachimescu, MD, FCCP, of Emory University, Atlanta, and the Atlanta Veteran Affairs Administration and CHEST Physician editorial board member, said in an interview that the study raises a major question of what is next. “What can we offer to these patients, and what is the real-world compliance to that ‘next-best’ modality?” Dr. Ioachimescu said. “What are the outcomes of these individuals in the point-of-care environment, or ‘real world?’ ”
The analysis by the authors adds the perspective of a “real-world depiction of clinical care for patients with OSA,” Dr. Ioachimescu said. “One major lesson of such an analysis is that the health care goal setting that is referential to initial, randomized, well-controlled studies on highly selected patient populations need to be reassessed periodically from the point of view of actual results in the clinics.”
Clinicians may need to borrow ideas from other therapeutic fields to help improve patient adherence, he said. “[W]e may be able to develop and implement in the future peer involvement, behavioral and cognitive approaches, motivational enhancement interventions, as well as elements of acceptance and commitment techniques, all in the larger context of more integrated and in the same time individualized approaches to therapy.”
The investigators concluded that, “relative to Medicare-only beneficiaries, those eligible for both Medicare and Medicaid were significantly less likely to adhere to CPAP. Future research should seek to develop a deeper understanding of the mechanisms through which [socioeconomic status] and other social determinants impact patient experience throughout the OSA diagnostic and treatment process, including receiving, acclimating, and adhering to CPAP therapy.”
Dr. Sundar concurred with this assessment and said more research is needed on factors impacting adherence such as poverty, homelessness, and home support systems. “It’s not just coordinating with the patient. Clearly, more work is needed in understanding the social aspects of CPAP adherence.”
This study was funded in part by an investigator-initiated grant provided by ResMed to Dr. Wickmire’s institution, the University of Maryland, Baltimore. Dr. Wickmire reported being a scientific consultant to DayZz, Eisai, Merck, and Purdue and holds shares in WellTap. Dr. Oldstone is a ResMed employee and shareholder. Dr. Sundar reported being a cofounder of Hypnoscure, which creates software for population management of sleep apnea, and an investigator in trials where ResMed and Respironics devices were used. Dr. Ioachimescu reported no relevant financial disclosures.
SOURCE: Wickwire EM et al. Sleep. 2020 Jun 23. doi: 10.1093/sleep/zsaa122.
FROM SLEEP
A guide to managing disorders of the ear pinna and canal
Which antibiotics are most useful for infection following ear piercing? When is it safe to attempt removal of a foreign body from the ear canal, and which cerumenolytic agent may be best for ear wax? This review covers common ailments of the outer ear, which are often readily diagnosed given a patient’s history and thorough physical examination. We also address more complicated matters such as deciding when to refer for treatment of suspected malignant otitis externa, and which lab markers to follow when managing it yourself.
A (very) brief review of ear anatomy
Understanding the unique embryology and intricate anatomy of the external ear informs our understanding of predictable infections, growths, and malformations.
The external ear is composed of the external auditory canal and auricle. The external auditory canal has a lateral (external) cartilaginous portion and a medial (internal) bony portion. The auricular structure is complex and formed by the helix, antihelix (crura; scaphoid fossa), tragus, antitragus, conchae, and lobule. The auricle is composed of elastic cartilage covered by skin. The lobule is composed of skin, adipose tissue, and connective tissue.
Embryologically, the auricle, auditory canal, and middle ear form from ectoderm of the first 2 branchial arches during early gestation. The auricle forms from the fusion of soft-tissue swellings (hillocks). Three hillocks arise from the first branchial arch and 3 from the second branchial arch during the fifth and sixth weeks of gestation. Tissues from the second branchial arch comprise the lobule, antihelix, and caudal helix. The cartilage of the tragus forms from the first branchial arch. The ear canal forms from an epithelial invagination of the first branchial arch that also occurs during the fifth week of gestation.1
Infections
Perichondritis
Inflammation or infection of the connective tissue layer surrounding the auricular cartilage (perichondrium) results in perichondritis. Further extension of infection can lead to an auricular abscess. Both of these conditions can have serious consequences.
What you’ll see. The most common risk factor for perichondritis is the popular practice of cosmetic transcartilaginous piercing.2 Piercing of the helix, scapha, or anti-helix (often referred to as “high” ear piercing) causes localized trauma that can strip the adjacent perichondrium, decrease blood supply, create cartilaginous microfractures, and lead to devascularization. Rates of infection as high as 35% have been reported with high-ear piercing.3
The most common microbes associated with perichondritis and pinna abscess formation are Pseudomonas and Staphylococcus species.2 P
Continue to: How to treat
How to treat. The cornerstone of treatment is early detection and antimicrobial coverage with antipseudomonal antibiotics. Ciprofloxacin is the oral antibiotic of choice because of its ability to penetrate the tissue.4 Other options include clindamycin and third- or fourth-generation cephalosporins. If the wound becomes abscessed, perform (or refer for) early surgical incision and drainage.5 A failure to promptly recognize perichondritis or to mistakenly prescribe non-antipseudomonal antibiotics contributes to increased rates of hospitalization.2 Cosmetic deformity is the most common complication of perichondritis. This may require reconstructive surgery.
Otitis externa
Acute otitis externa (AOE; “swimmer’s ear”) is cellulitis of the skin and subdermis of the external ear canal. It is most prevalent in warm, moist climates and almost always associated with acute bacterial infection, most commonly P aeruginosa or S aureus.6 There is also an increased association with poor water quality (containing higher bacterial loads). Anything breaching the integrity of the ear canal can potentially predispose to the development of AOE. This includes trauma from cleaning, cerumen removal, scratching due to allergic conditions, and placement of hearing-aid devices.6
What you’ll see. Suspect AOE when signs or symptoms of ear canal inflammation have appeared rapidly (generally within 2 days) over the past 3 weeks.7 Findings include otalgia, itching, fullness, tragal tenderness, ear canal edema, erythema with or without otorrhea, lymphadenitis, or cellulitis of the pinna or adjacent skin.7 AOE must be distinguished from other causes of otalgia and otorrhea, including dermatitis and viral infection.
How to treat. Topical therapy is recommended for the initial treatment of uncomplicated AOE, usually given over 7 days. Multiple topical preparations are available, such as ciprofloxacin 0.2%/hydrocortisone 1.0%; neomycin/polymyxin B/hydrocortisone; ofloxacin 0.3%; or acetic acid 2.0%.7 Avoid these agents, though, if you suspect tympanic membrane rupture. Quinolone drops are the only topical antimicrobials approved for middle ear use.7
Systemic antibiotics are not recommended for the initial treatment of AOE. Topical agents deliver a much higher concentration of medication than can be achieved systemically. Consider systemic antibiotics if there is extension outside the ear canal, a concern for necrotizing otitis externa (more on this in a bit), or the patient is immunodeficient.8
Continue to: Patient (or parent) education...
Patient (or parent) education is important to ensure proper medication administration. The patient should lie down with the affected ear facing up. After the canal is filled with drops, the patient should remain in this position for 3 to 5 minutes. Gently massaging the tragus can augment delivery. Patients should keep the ear canal as dry as possible and avoid inserting objects (eg, hearing aids, ear buds, cotton-tipped applicators) into the canal for the duration of treatment. The delivery of topical antibiotics can be enhanced by wick placement. Prescribe analgesics (typically nonsteroidal anti-inflammatory agents) based on severity of pain.7
Have patients abstain from water sports for 7 to 10 days. Showering is acceptable with minimal ear exposure to water; bathing is preferred when possible. If there is no clinical improvement in 48 to 72 hours, ask patients to return for re-evaluation.8 Prevention is essential for patients with a history of recurrent otitis externa. Acetic acid solutions create an acidic environment within the canal to help prevent recurrent AOE. Ear plugs and petroleum jelly–soaked cotton plugs prior to water exposure may also help prevent recurrent AOE.
Malignant otitis externa
Malignant, or necrotizing, otitis externa is an aggressive disease form of otitis externa that is most common in individuals with diabetes or other immunodeficiency disorders.9 Most cases are due to infection with P aeruginosa.10 Prior to the availability of effective antibiotics, mortality rates in patients with necrotizing otitis externa were as high as 50%.11
What you’ll see. Patients typically present with severe ear pain, otorrhea, conductive hearing loss, and a feeling of fullness in the external ear canal. Physical examination reveals purulent otorrhea and a swollen, tender ear canal. Exposed bone may be visible, most often on the floor of the canal. The tympanic membrane and middle ear are seldom involved on initial presentation.
The infection often originates at the junction of the bony and cartilaginous portion of the external canal, spreading through the fissures of Santorini to the skull base. If not aggressively treated, the infection spreads medially to the tympanomastoid suture causing intracranial complications—usually a facial nerve neuropathy.
Continue to: Given these clinical findings...
Given these clinical findings, promptly order laboratory studies and imaging to confirm the diagnosis. The erythrocyte sedimentation rate and C-reactive protein level are typically elevated, and either can be used as a marker to follow treatment. Computed tomography (CT) helps to determine the location and extent of disease and is recommended as the initial diagnostic imaging modality for patients with suspected malignant otitis externa.12
Magnetic resonance imaging helps define soft-tissue changes, dural enhancement, and involvement of medullary bone, making this the preferred modality to monitor therapeutic response.12 Technetium bone scanning can also be used for the initial diagnosis (particularly if CT findings are normal and clinical suspicion is high) and for follow-up with treatment.
How to treat. Management involves a team approach with otolaryngology, radiology, neurology, endocrinology, and infectious disease specialists. Long term (6-8 weeks) antipseudomonal antibiotic treatment is typical.
Let culture results guide the choice of antibiotic. Fluoroquinolone therapy, usually ciprofloxacin, is used most often.12 Surgical intervention may be required for local debridement and drainage of abscesses. Close follow-up is necessary due to reports of recurrence up to 1 year after treatment. If left untreated, necrotizing otitis externa can lead to osteomyelitis, meningitis, septic thrombosis, cerebral abscess, and death.11
Cerumen impaction
The relatively small diameter of the external auditory canal increases the risk for impaction of cerumen and foreign bodies. Cerumen impaction, in particular, is a common primary care complaint. Cerumen forms when glandular secretions from the outer two-thirds of the ear canal mix with exfoliated skin. It functions as a lubricant for the ear canal and as a barrier against infection, water accumulation, and foreign bodies.13
Continue to: What you'll see
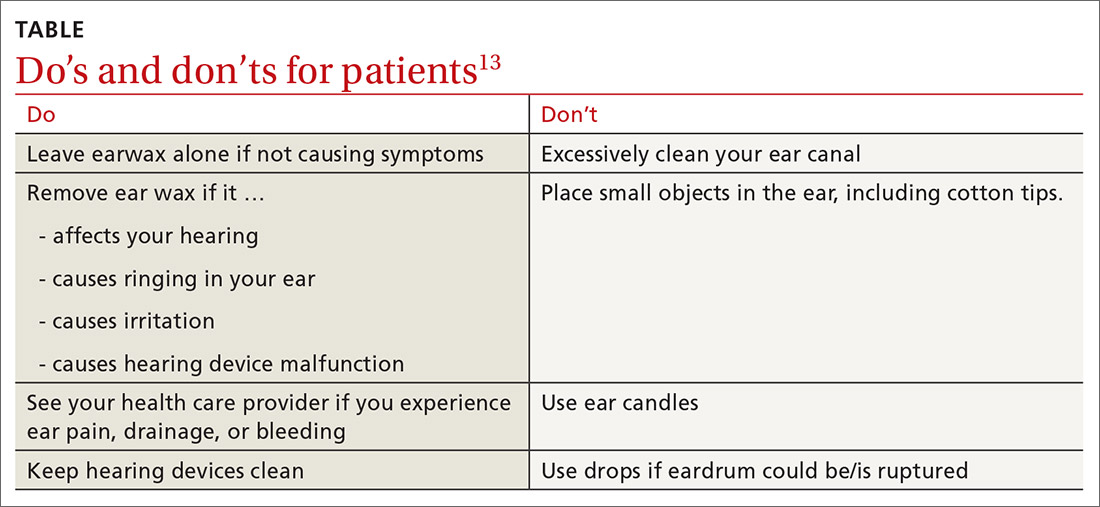
What you’ll see. You may encounter cerumen impaction in an asymptomatic patient when it prevents visualization of the external auditory canal or tympanic membrane, or when a patient complains of conductive hearing loss, tinnitus, dizziness, ear pain, itching, and cough.13 It is found in 1 in 10 children and 1 in 20 adults.13 There is a higher incidence in patients who are elderly, are cognitively impaired, or wear hearing devices or ear plugs.13,14 Asymptomatic cerumen impaction should not be treated. A recent clinical guideline provides a useful “do and don’t” list for patient education (TABLE).13
How to treat. In asymptomatic patients, the presence of cerumen on examination is not an indication for removal. Based on current guidelines,13 impacted cerumen can safely be removed from the ear canal of symptomatic patients in several ways:
- Manual removal with cerumen loop/spoon or alligator forceps. This method decreases the risk for infection because it limits moisture exposure. However, it should be performed by a health care provider trained in its use because of the risk for trauma to the ear canal and tympanic membrane.
- Irrigation of the ear using tap water or a 50-50 solution of hydrogen peroxide and water. Irrigation can be achieved with a syringe or jet irrigator using a modified tip. This method also has a risk for trauma to the ear canal and tympanic membrane and should only be performed by appropriately trained health care professionals.
- Use of cerumenolytic agents to soften and thin earwax and promote natural extrusion. Several types of cerumenolytic drops (water-based and oil-based) are available and appear to be equally effective. Water-based solutions contain hydrogen peroxide, docusate sodium, acetic acid, and sodium bicarbonate. Oil-based drops may contain peanut, almond, or olive oils. A thorough allergic history should be performed to avoid using products in patients with nut allergies. In head-to-head laboratory comparisons, distilled water appears to be the best cerumenolytic.15
Foreign bodies
Foreign bodies in the external auditory canal (typically beads, cotton tips, and insects) are more common in children than adults.16
What you’ll see. Most foreign bodies are lodged in the bony part of the external auditory canal, and many patients try to remove the object before seeking medical care. Removal requires adequate visualization and skill.17 Although patients may be asymptomatic, most complain of pain, fullness, decreased hearing, or otorrhea.
How to treat. Directly visible objects can often be removed without referral. Suction, irrigation, forceps, probes, and fine hooks have been used. Insect removal can be facilitated by first flooding the canal with xylocaine, alcohol, or mineral oil. Acetone may be used to dissolve foreign bodies containing Styrofoam or to loosen glues. If the object is a button battery, avoid irrigation to prevent liquefaction tissue necrosis.
Continue to: Complications of foreign body removal...
Complications of foreign body removal include pain, otitis externa, otitis media, and trauma to the ear or tympanic membrane. The likelihood of successful removal of the object decreases and the risk for complications increases with each subsequent attempt.17 Consult an otolaryngologist if sedation or anesthesia is required, the foreign body is tightly wedged, there is trauma to the ear canal or tympanic membrane, the foreign body has a sharp edge (eg, glass or wire), or removal attempts have been unsuccessful.
Trauma
Sports injuries, motor vehicle accidents, bites, falls, and burns are the primary causes of trauma to the external ear.18
What you’ll see. Blunt auricular trauma predisposes to infection, necrosis, and scar contracture. One of the most common sequelae is cauliflower ear. Trauma is particularly common with contact sports such as boxing, wrestling, or mixed martial arts. The skin of the auricle attaches directly to the perichondrium. Following blunt or shearing trauma to the auricle, hematomas form within the space between the perichondrium and cartilage of the anterior ear.19
How to treat. Small hematomas can be managed by aspiration, while larger ones generally require open drainage.20 Newer treatments involving pressure dressings and the use of fibrin glue have been proposed.20 Recommend that athletes participating in contact sports wear appropriate protective headgear to prevent auricular hematoma and cauliflower ear.
Neoplasm
Roughly 5% of all skin cancers involve the ear, most frequently the pinna due to chronic sun exposure.21 The most frequently occurring malignancy of the external ear is basal cell carcinoma (BCC), which is responsible for 80% of all nonmelanoma skin cancers.22
Continue to: What you'll see
What you’ll see. BCC of the ear usually involves the preauricular area and the helix. The risk for BCC is related to exposure to ultraviolet radiation. BCC of the ear is more common in men and can be particularly aggressive, highlighting the importance of prevention and prompt recognition. BCC typically presents as a fleshy papule that is often translucent or “pearly’” and has overlying telangiectasia and a “rolled” border. Central ulceration can occur as well.
How to treat. Usual treatment of BCC is surgical excision. Prevention is critical and centers on sun avoidance or the use of appropriate sunscreens.
In addition to BCC, exposure of the external ear to sunlight and ultraviolet radiation predisposes patients to the development of squamous cell carcinoma (SCC) and melanoma. SCC has a variety of presentations including papules, plaques, and nodules. SCC has a higher metastatic potential than does BCC.
Keloid
Keloids are an abnormal healing response to soft-tissue injury: benign fibrocartilaginous growths that extend beyond the original wound.
What you’ll see. Keloids are more common in dark-skinned individuals and tend to result from burns, surgical incisions, infection, trauma, tattooing, injections, piercings, and arthropod bites. In some cases, they arise spontaneously. Keloids are more common in areas of increased skin tension (chest, shoulders, back), but may occur on the ears—most commonly after piercing or trauma. Keloids present clinically as slow-growing rubbery or firm nodules. The diagnosis is typically based on clinical appearance but can be confirmed by histopathology.
Continue to: How to treat
How to treat. Treatments vary and include observation, excision, intralesional injections, cryotherapy, enzyme therapy, silicone gel application, and irradiation.23 Recurrence is common; no therapy has been proven to be universally superior or preferred.
Congenital malformations
Atresia
Disruption of embryologic development (failed invagination of the external auditory canal) can lead to a stenotic or absent ear canal (aural atresia). Aural atresia is also often associated with fusion of the incus and malleus. This condition occurs predominantly in males. Unilateral atresia is more common than bilateral atresia, and the right ear is more often involved than the left.24
Microtia
Microtia is the incomplete development of the pinna leading to a small or deformed pinna. Microtia can be unilateral or bilateral. As with atresia, microtia more commonly affects males and, if unilateral, the right side is more often affected than the left. Microtia can occur in isolation but is often associated with genetic syndromes such as Treacher Collins syndrome and craniofacial microsomia (Goldenhar syndrome). When microtia is identified (typically at birth or early infancy), audiologic testing and a thorough physical examination for evidence of associated defects should be performed. Consult with an audiologist, clinical geneticist, or pediatric otolaryngologist.
Pre-auricular pits
Pre-auricular pits (sinuses) are tiny indentations anterior to the helix and superior to the tragus. While pre-auricular pits are more common on the right side, they are bilateral in 25% to 50% of cases.25 Pre-auricular pits occur in up to 1% of white children, 5% of black children, and 10% of Asian children.25 Children with this condition should undergo formal audiologic testing as their risk for hearing loss is higher compared with the general population.26
The branchio-oto-renal syndrome (associated with pre-auricular pits and hearing loss) also features structural defects of the ear, renal anomalies and/or nasolacrimal duct stenosis or fistulas. If this syndrome is suspected, renal ultrasound imaging is warranted. Other indications for renal ultrasound in patients with a pre-auricular pit are any dysmorphic feature, a family history of deafness, an auricular malformation, or a maternal history of gestational diabetes.27 Pre-auricular pits do not require surgery unless they drain chronically or become recurrently infected. Complete surgical excision is the treatment of choice in these cases.
CORRESPONDENCE
Mark Stephens, MD, 1850 Park Avenue, State College, PA 16801; mstephens3@pennstatehealth.psu.edu
1. Cox TC, Camci ED, Vora S, et al. The genetics of auricular development and malformation: new findings in model systems driving future directions for microtia research. Eur J Med Genet. 2014;57:394-401.
2. Sosin M, Weissler JM, Pulcrano M, et al. Transcartilaginous ear piercing and infectious complications: a systematic review and critical analysis of outcomes. Laryngoscope. 2015;125:1827-1834.
3. Stirn A. Body piercing: medical consequences and psychological motivations. Lancet. 2003;361:1205-1215.
4. Liu ZW, Chokkalingam P. Piercing associated perichondritis of the pinna: are we treating it correctly? J Larygol Oncol. 2013;127:505-508.
5. Mitchell S, Ditta K, Minhas S, et al. Pinna abscesses: can we manage them better? A case series and review of the literature. Eur Arch Otorhinolaryngol. 2015;272:3163-3167.
6. Stone KE. Otitis externa. Pediatr Rev. 2007;28:77-78.
7. Rosenfeld RM, Schwartz SR, Cannon CR, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2014;150(1 suppl):S1-S24.
8. Prentice P. American Academy of Otolaryngology: Head and Neck Surgery Foundation clinical practice guideline on acute otitis externa. Arch Dis Child Educ Pract Ed. 2015;100:197.
9. Unadkat S, Kanzara T, Watters G. Necrotising otitis externa in the immunocompetent patient. J Laryngol Otol. 2018;132:71-74.
10. Carfrae MJ, Kesser BW. Malignant otitis externa. Otolarngol Clin N Am. 2008;41:537-549.
11. Chandler JR, Malignant otitis externa. Laryngoscope. 1968;78:1257-1294.
12. Hollis S, Evans K. Management of malignant (necrotising) otitis externa. J Laryngol Otol. 2011;125:1212-1217.
13. Schwartz SR, Magit AE, Rosenfeld RM, et al. Clinical practice guideline (update): earwax (cerumen impaction). Otolaryngol Head Neck Surg. 2017;156:S1-S29.
14. Guest JF, Greener MJ, Robinson AC, et al. Impacted cerumen: composition, production, epidemiology and management. QJM. 2004;97:477-488.
15. Saxby C, Williams R, Hickey S. Finding the most effective cerumenolytic. J Laryngol Otol. 2013;127:1067-1070.
16. Awad AH, ElTaher M. ENT foreign bodies: an experience. Int Arch Otorhinolaryngol. 2018;22:146-151.
17. Heim SW, Maughan KL. Foreign bodies in the ear, nose, and throat. Am Fam Physician. 2007;76:1185-1189.
18. Sharma K, Goswami SC, Baruah DK. Auricular trauma and its management. Indian J Otolaryngol Head Neck Surg. 2006;58:232-234.
19. Haik J, Givol O, Kornhaber R, et al. Cauliflower ear–a minimally invasive treatment in a wrestling athlete: a case report. Int Med Case Rep J. 2018;11:5-7.
20. Ebrahimi A, Kazemi A, Rasouli HR, et al. Reconstructive surgery of auricular defects: an overview. Trauma Mon. 2015;20:e28202.
21. Warner E, Weston C, Barclay-Klingle N, et al. The swollen pinna. BMJ. 2017; 359; j5073.
22. Rubin AI, Chen EH, Ratner D. Basal cell carcinoma. N Engl J Med. 2005;353:2262-2269.
23. Ranjan SK, Ahmed A, Harsh V, et al. Giant bilateral keloids of the ear lobule: case report and brief review of the literature. J Family Med Prim Care. 2017;6:677-679.
24. Roland PS, Marple BF. Disorders of the external auditory canal. J Am Acad Audiol. 1997;8:367-378.
25. Scheinfeld NS, Silverberg NB, Weinberg JM, et al. The preauricular sinus: a review of its clinical presentation, treatment, and associations. Pediatr Dermatol. 2004;21:191-196.
26. Roth DA, Hildesheimer M, Bardestein S, et al. Preauricular skin tags and ear pits are associated with permanent hearing impairment in newborns. Pediatrics. 2008;122:e884-890.
27. Tan T, Constantinides H, Mitchell TE. The preauricular sinus: a review of its aetiology, clinical presentation and management. Int J Ped Otorhinolaryngol. 2005;69:1469-1474.
Which antibiotics are most useful for infection following ear piercing? When is it safe to attempt removal of a foreign body from the ear canal, and which cerumenolytic agent may be best for ear wax? This review covers common ailments of the outer ear, which are often readily diagnosed given a patient’s history and thorough physical examination. We also address more complicated matters such as deciding when to refer for treatment of suspected malignant otitis externa, and which lab markers to follow when managing it yourself.
A (very) brief review of ear anatomy
Understanding the unique embryology and intricate anatomy of the external ear informs our understanding of predictable infections, growths, and malformations.
The external ear is composed of the external auditory canal and auricle. The external auditory canal has a lateral (external) cartilaginous portion and a medial (internal) bony portion. The auricular structure is complex and formed by the helix, antihelix (crura; scaphoid fossa), tragus, antitragus, conchae, and lobule. The auricle is composed of elastic cartilage covered by skin. The lobule is composed of skin, adipose tissue, and connective tissue.
Embryologically, the auricle, auditory canal, and middle ear form from ectoderm of the first 2 branchial arches during early gestation. The auricle forms from the fusion of soft-tissue swellings (hillocks). Three hillocks arise from the first branchial arch and 3 from the second branchial arch during the fifth and sixth weeks of gestation. Tissues from the second branchial arch comprise the lobule, antihelix, and caudal helix. The cartilage of the tragus forms from the first branchial arch. The ear canal forms from an epithelial invagination of the first branchial arch that also occurs during the fifth week of gestation.1
Infections
Perichondritis
Inflammation or infection of the connective tissue layer surrounding the auricular cartilage (perichondrium) results in perichondritis. Further extension of infection can lead to an auricular abscess. Both of these conditions can have serious consequences.
What you’ll see. The most common risk factor for perichondritis is the popular practice of cosmetic transcartilaginous piercing.2 Piercing of the helix, scapha, or anti-helix (often referred to as “high” ear piercing) causes localized trauma that can strip the adjacent perichondrium, decrease blood supply, create cartilaginous microfractures, and lead to devascularization. Rates of infection as high as 35% have been reported with high-ear piercing.3
The most common microbes associated with perichondritis and pinna abscess formation are Pseudomonas and Staphylococcus species.2 P
Continue to: How to treat
How to treat. The cornerstone of treatment is early detection and antimicrobial coverage with antipseudomonal antibiotics. Ciprofloxacin is the oral antibiotic of choice because of its ability to penetrate the tissue.4 Other options include clindamycin and third- or fourth-generation cephalosporins. If the wound becomes abscessed, perform (or refer for) early surgical incision and drainage.5 A failure to promptly recognize perichondritis or to mistakenly prescribe non-antipseudomonal antibiotics contributes to increased rates of hospitalization.2 Cosmetic deformity is the most common complication of perichondritis. This may require reconstructive surgery.
Otitis externa
Acute otitis externa (AOE; “swimmer’s ear”) is cellulitis of the skin and subdermis of the external ear canal. It is most prevalent in warm, moist climates and almost always associated with acute bacterial infection, most commonly P aeruginosa or S aureus.6 There is also an increased association with poor water quality (containing higher bacterial loads). Anything breaching the integrity of the ear canal can potentially predispose to the development of AOE. This includes trauma from cleaning, cerumen removal, scratching due to allergic conditions, and placement of hearing-aid devices.6
What you’ll see. Suspect AOE when signs or symptoms of ear canal inflammation have appeared rapidly (generally within 2 days) over the past 3 weeks.7 Findings include otalgia, itching, fullness, tragal tenderness, ear canal edema, erythema with or without otorrhea, lymphadenitis, or cellulitis of the pinna or adjacent skin.7 AOE must be distinguished from other causes of otalgia and otorrhea, including dermatitis and viral infection.
How to treat. Topical therapy is recommended for the initial treatment of uncomplicated AOE, usually given over 7 days. Multiple topical preparations are available, such as ciprofloxacin 0.2%/hydrocortisone 1.0%; neomycin/polymyxin B/hydrocortisone; ofloxacin 0.3%; or acetic acid 2.0%.7 Avoid these agents, though, if you suspect tympanic membrane rupture. Quinolone drops are the only topical antimicrobials approved for middle ear use.7
Systemic antibiotics are not recommended for the initial treatment of AOE. Topical agents deliver a much higher concentration of medication than can be achieved systemically. Consider systemic antibiotics if there is extension outside the ear canal, a concern for necrotizing otitis externa (more on this in a bit), or the patient is immunodeficient.8
Continue to: Patient (or parent) education...
Patient (or parent) education is important to ensure proper medication administration. The patient should lie down with the affected ear facing up. After the canal is filled with drops, the patient should remain in this position for 3 to 5 minutes. Gently massaging the tragus can augment delivery. Patients should keep the ear canal as dry as possible and avoid inserting objects (eg, hearing aids, ear buds, cotton-tipped applicators) into the canal for the duration of treatment. The delivery of topical antibiotics can be enhanced by wick placement. Prescribe analgesics (typically nonsteroidal anti-inflammatory agents) based on severity of pain.7
Have patients abstain from water sports for 7 to 10 days. Showering is acceptable with minimal ear exposure to water; bathing is preferred when possible. If there is no clinical improvement in 48 to 72 hours, ask patients to return for re-evaluation.8 Prevention is essential for patients with a history of recurrent otitis externa. Acetic acid solutions create an acidic environment within the canal to help prevent recurrent AOE. Ear plugs and petroleum jelly–soaked cotton plugs prior to water exposure may also help prevent recurrent AOE.
Malignant otitis externa
Malignant, or necrotizing, otitis externa is an aggressive disease form of otitis externa that is most common in individuals with diabetes or other immunodeficiency disorders.9 Most cases are due to infection with P aeruginosa.10 Prior to the availability of effective antibiotics, mortality rates in patients with necrotizing otitis externa were as high as 50%.11
What you’ll see. Patients typically present with severe ear pain, otorrhea, conductive hearing loss, and a feeling of fullness in the external ear canal. Physical examination reveals purulent otorrhea and a swollen, tender ear canal. Exposed bone may be visible, most often on the floor of the canal. The tympanic membrane and middle ear are seldom involved on initial presentation.
The infection often originates at the junction of the bony and cartilaginous portion of the external canal, spreading through the fissures of Santorini to the skull base. If not aggressively treated, the infection spreads medially to the tympanomastoid suture causing intracranial complications—usually a facial nerve neuropathy.
Continue to: Given these clinical findings...
Given these clinical findings, promptly order laboratory studies and imaging to confirm the diagnosis. The erythrocyte sedimentation rate and C-reactive protein level are typically elevated, and either can be used as a marker to follow treatment. Computed tomography (CT) helps to determine the location and extent of disease and is recommended as the initial diagnostic imaging modality for patients with suspected malignant otitis externa.12
Magnetic resonance imaging helps define soft-tissue changes, dural enhancement, and involvement of medullary bone, making this the preferred modality to monitor therapeutic response.12 Technetium bone scanning can also be used for the initial diagnosis (particularly if CT findings are normal and clinical suspicion is high) and for follow-up with treatment.
How to treat. Management involves a team approach with otolaryngology, radiology, neurology, endocrinology, and infectious disease specialists. Long term (6-8 weeks) antipseudomonal antibiotic treatment is typical.
Let culture results guide the choice of antibiotic. Fluoroquinolone therapy, usually ciprofloxacin, is used most often.12 Surgical intervention may be required for local debridement and drainage of abscesses. Close follow-up is necessary due to reports of recurrence up to 1 year after treatment. If left untreated, necrotizing otitis externa can lead to osteomyelitis, meningitis, septic thrombosis, cerebral abscess, and death.11
Cerumen impaction
The relatively small diameter of the external auditory canal increases the risk for impaction of cerumen and foreign bodies. Cerumen impaction, in particular, is a common primary care complaint. Cerumen forms when glandular secretions from the outer two-thirds of the ear canal mix with exfoliated skin. It functions as a lubricant for the ear canal and as a barrier against infection, water accumulation, and foreign bodies.13
Continue to: What you'll see
What you’ll see. You may encounter cerumen impaction in an asymptomatic patient when it prevents visualization of the external auditory canal or tympanic membrane, or when a patient complains of conductive hearing loss, tinnitus, dizziness, ear pain, itching, and cough.13 It is found in 1 in 10 children and 1 in 20 adults.13 There is a higher incidence in patients who are elderly, are cognitively impaired, or wear hearing devices or ear plugs.13,14 Asymptomatic cerumen impaction should not be treated. A recent clinical guideline provides a useful “do and don’t” list for patient education (TABLE).13
How to treat. In asymptomatic patients, the presence of cerumen on examination is not an indication for removal. Based on current guidelines,13 impacted cerumen can safely be removed from the ear canal of symptomatic patients in several ways:
- Manual removal with cerumen loop/spoon or alligator forceps. This method decreases the risk for infection because it limits moisture exposure. However, it should be performed by a health care provider trained in its use because of the risk for trauma to the ear canal and tympanic membrane.
- Irrigation of the ear using tap water or a 50-50 solution of hydrogen peroxide and water. Irrigation can be achieved with a syringe or jet irrigator using a modified tip. This method also has a risk for trauma to the ear canal and tympanic membrane and should only be performed by appropriately trained health care professionals.
- Use of cerumenolytic agents to soften and thin earwax and promote natural extrusion. Several types of cerumenolytic drops (water-based and oil-based) are available and appear to be equally effective. Water-based solutions contain hydrogen peroxide, docusate sodium, acetic acid, and sodium bicarbonate. Oil-based drops may contain peanut, almond, or olive oils. A thorough allergic history should be performed to avoid using products in patients with nut allergies. In head-to-head laboratory comparisons, distilled water appears to be the best cerumenolytic.15
Foreign bodies
Foreign bodies in the external auditory canal (typically beads, cotton tips, and insects) are more common in children than adults.16
What you’ll see. Most foreign bodies are lodged in the bony part of the external auditory canal, and many patients try to remove the object before seeking medical care. Removal requires adequate visualization and skill.17 Although patients may be asymptomatic, most complain of pain, fullness, decreased hearing, or otorrhea.
How to treat. Directly visible objects can often be removed without referral. Suction, irrigation, forceps, probes, and fine hooks have been used. Insect removal can be facilitated by first flooding the canal with xylocaine, alcohol, or mineral oil. Acetone may be used to dissolve foreign bodies containing Styrofoam or to loosen glues. If the object is a button battery, avoid irrigation to prevent liquefaction tissue necrosis.
Continue to: Complications of foreign body removal...
Complications of foreign body removal include pain, otitis externa, otitis media, and trauma to the ear or tympanic membrane. The likelihood of successful removal of the object decreases and the risk for complications increases with each subsequent attempt.17 Consult an otolaryngologist if sedation or anesthesia is required, the foreign body is tightly wedged, there is trauma to the ear canal or tympanic membrane, the foreign body has a sharp edge (eg, glass or wire), or removal attempts have been unsuccessful.
Trauma
Sports injuries, motor vehicle accidents, bites, falls, and burns are the primary causes of trauma to the external ear.18
What you’ll see. Blunt auricular trauma predisposes to infection, necrosis, and scar contracture. One of the most common sequelae is cauliflower ear. Trauma is particularly common with contact sports such as boxing, wrestling, or mixed martial arts. The skin of the auricle attaches directly to the perichondrium. Following blunt or shearing trauma to the auricle, hematomas form within the space between the perichondrium and cartilage of the anterior ear.19
How to treat. Small hematomas can be managed by aspiration, while larger ones generally require open drainage.20 Newer treatments involving pressure dressings and the use of fibrin glue have been proposed.20 Recommend that athletes participating in contact sports wear appropriate protective headgear to prevent auricular hematoma and cauliflower ear.
Neoplasm
Roughly 5% of all skin cancers involve the ear, most frequently the pinna due to chronic sun exposure.21 The most frequently occurring malignancy of the external ear is basal cell carcinoma (BCC), which is responsible for 80% of all nonmelanoma skin cancers.22
Continue to: What you'll see
What you’ll see. BCC of the ear usually involves the preauricular area and the helix. The risk for BCC is related to exposure to ultraviolet radiation. BCC of the ear is more common in men and can be particularly aggressive, highlighting the importance of prevention and prompt recognition. BCC typically presents as a fleshy papule that is often translucent or “pearly’” and has overlying telangiectasia and a “rolled” border. Central ulceration can occur as well.
How to treat. Usual treatment of BCC is surgical excision. Prevention is critical and centers on sun avoidance or the use of appropriate sunscreens.
In addition to BCC, exposure of the external ear to sunlight and ultraviolet radiation predisposes patients to the development of squamous cell carcinoma (SCC) and melanoma. SCC has a variety of presentations including papules, plaques, and nodules. SCC has a higher metastatic potential than does BCC.
Keloid
Keloids are an abnormal healing response to soft-tissue injury: benign fibrocartilaginous growths that extend beyond the original wound.
What you’ll see. Keloids are more common in dark-skinned individuals and tend to result from burns, surgical incisions, infection, trauma, tattooing, injections, piercings, and arthropod bites. In some cases, they arise spontaneously. Keloids are more common in areas of increased skin tension (chest, shoulders, back), but may occur on the ears—most commonly after piercing or trauma. Keloids present clinically as slow-growing rubbery or firm nodules. The diagnosis is typically based on clinical appearance but can be confirmed by histopathology.
Continue to: How to treat
How to treat. Treatments vary and include observation, excision, intralesional injections, cryotherapy, enzyme therapy, silicone gel application, and irradiation.23 Recurrence is common; no therapy has been proven to be universally superior or preferred.
Congenital malformations
Atresia
Disruption of embryologic development (failed invagination of the external auditory canal) can lead to a stenotic or absent ear canal (aural atresia). Aural atresia is also often associated with fusion of the incus and malleus. This condition occurs predominantly in males. Unilateral atresia is more common than bilateral atresia, and the right ear is more often involved than the left.24
Microtia
Microtia is the incomplete development of the pinna leading to a small or deformed pinna. Microtia can be unilateral or bilateral. As with atresia, microtia more commonly affects males and, if unilateral, the right side is more often affected than the left. Microtia can occur in isolation but is often associated with genetic syndromes such as Treacher Collins syndrome and craniofacial microsomia (Goldenhar syndrome). When microtia is identified (typically at birth or early infancy), audiologic testing and a thorough physical examination for evidence of associated defects should be performed. Consult with an audiologist, clinical geneticist, or pediatric otolaryngologist.
Pre-auricular pits
Pre-auricular pits (sinuses) are tiny indentations anterior to the helix and superior to the tragus. While pre-auricular pits are more common on the right side, they are bilateral in 25% to 50% of cases.25 Pre-auricular pits occur in up to 1% of white children, 5% of black children, and 10% of Asian children.25 Children with this condition should undergo formal audiologic testing as their risk for hearing loss is higher compared with the general population.26
The branchio-oto-renal syndrome (associated with pre-auricular pits and hearing loss) also features structural defects of the ear, renal anomalies and/or nasolacrimal duct stenosis or fistulas. If this syndrome is suspected, renal ultrasound imaging is warranted. Other indications for renal ultrasound in patients with a pre-auricular pit are any dysmorphic feature, a family history of deafness, an auricular malformation, or a maternal history of gestational diabetes.27 Pre-auricular pits do not require surgery unless they drain chronically or become recurrently infected. Complete surgical excision is the treatment of choice in these cases.
CORRESPONDENCE
Mark Stephens, MD, 1850 Park Avenue, State College, PA 16801; mstephens3@pennstatehealth.psu.edu
Which antibiotics are most useful for infection following ear piercing? When is it safe to attempt removal of a foreign body from the ear canal, and which cerumenolytic agent may be best for ear wax? This review covers common ailments of the outer ear, which are often readily diagnosed given a patient’s history and thorough physical examination. We also address more complicated matters such as deciding when to refer for treatment of suspected malignant otitis externa, and which lab markers to follow when managing it yourself.
A (very) brief review of ear anatomy
Understanding the unique embryology and intricate anatomy of the external ear informs our understanding of predictable infections, growths, and malformations.
The external ear is composed of the external auditory canal and auricle. The external auditory canal has a lateral (external) cartilaginous portion and a medial (internal) bony portion. The auricular structure is complex and formed by the helix, antihelix (crura; scaphoid fossa), tragus, antitragus, conchae, and lobule. The auricle is composed of elastic cartilage covered by skin. The lobule is composed of skin, adipose tissue, and connective tissue.
Embryologically, the auricle, auditory canal, and middle ear form from ectoderm of the first 2 branchial arches during early gestation. The auricle forms from the fusion of soft-tissue swellings (hillocks). Three hillocks arise from the first branchial arch and 3 from the second branchial arch during the fifth and sixth weeks of gestation. Tissues from the second branchial arch comprise the lobule, antihelix, and caudal helix. The cartilage of the tragus forms from the first branchial arch. The ear canal forms from an epithelial invagination of the first branchial arch that also occurs during the fifth week of gestation.1
Infections
Perichondritis
Inflammation or infection of the connective tissue layer surrounding the auricular cartilage (perichondrium) results in perichondritis. Further extension of infection can lead to an auricular abscess. Both of these conditions can have serious consequences.
What you’ll see. The most common risk factor for perichondritis is the popular practice of cosmetic transcartilaginous piercing.2 Piercing of the helix, scapha, or anti-helix (often referred to as “high” ear piercing) causes localized trauma that can strip the adjacent perichondrium, decrease blood supply, create cartilaginous microfractures, and lead to devascularization. Rates of infection as high as 35% have been reported with high-ear piercing.3
The most common microbes associated with perichondritis and pinna abscess formation are Pseudomonas and Staphylococcus species.2 P
Continue to: How to treat
How to treat. The cornerstone of treatment is early detection and antimicrobial coverage with antipseudomonal antibiotics. Ciprofloxacin is the oral antibiotic of choice because of its ability to penetrate the tissue.4 Other options include clindamycin and third- or fourth-generation cephalosporins. If the wound becomes abscessed, perform (or refer for) early surgical incision and drainage.5 A failure to promptly recognize perichondritis or to mistakenly prescribe non-antipseudomonal antibiotics contributes to increased rates of hospitalization.2 Cosmetic deformity is the most common complication of perichondritis. This may require reconstructive surgery.
Otitis externa
Acute otitis externa (AOE; “swimmer’s ear”) is cellulitis of the skin and subdermis of the external ear canal. It is most prevalent in warm, moist climates and almost always associated with acute bacterial infection, most commonly P aeruginosa or S aureus.6 There is also an increased association with poor water quality (containing higher bacterial loads). Anything breaching the integrity of the ear canal can potentially predispose to the development of AOE. This includes trauma from cleaning, cerumen removal, scratching due to allergic conditions, and placement of hearing-aid devices.6
What you’ll see. Suspect AOE when signs or symptoms of ear canal inflammation have appeared rapidly (generally within 2 days) over the past 3 weeks.7 Findings include otalgia, itching, fullness, tragal tenderness, ear canal edema, erythema with or without otorrhea, lymphadenitis, or cellulitis of the pinna or adjacent skin.7 AOE must be distinguished from other causes of otalgia and otorrhea, including dermatitis and viral infection.
How to treat. Topical therapy is recommended for the initial treatment of uncomplicated AOE, usually given over 7 days. Multiple topical preparations are available, such as ciprofloxacin 0.2%/hydrocortisone 1.0%; neomycin/polymyxin B/hydrocortisone; ofloxacin 0.3%; or acetic acid 2.0%.7 Avoid these agents, though, if you suspect tympanic membrane rupture. Quinolone drops are the only topical antimicrobials approved for middle ear use.7
Systemic antibiotics are not recommended for the initial treatment of AOE. Topical agents deliver a much higher concentration of medication than can be achieved systemically. Consider systemic antibiotics if there is extension outside the ear canal, a concern for necrotizing otitis externa (more on this in a bit), or the patient is immunodeficient.8
Continue to: Patient (or parent) education...
Patient (or parent) education is important to ensure proper medication administration. The patient should lie down with the affected ear facing up. After the canal is filled with drops, the patient should remain in this position for 3 to 5 minutes. Gently massaging the tragus can augment delivery. Patients should keep the ear canal as dry as possible and avoid inserting objects (eg, hearing aids, ear buds, cotton-tipped applicators) into the canal for the duration of treatment. The delivery of topical antibiotics can be enhanced by wick placement. Prescribe analgesics (typically nonsteroidal anti-inflammatory agents) based on severity of pain.7
Have patients abstain from water sports for 7 to 10 days. Showering is acceptable with minimal ear exposure to water; bathing is preferred when possible. If there is no clinical improvement in 48 to 72 hours, ask patients to return for re-evaluation.8 Prevention is essential for patients with a history of recurrent otitis externa. Acetic acid solutions create an acidic environment within the canal to help prevent recurrent AOE. Ear plugs and petroleum jelly–soaked cotton plugs prior to water exposure may also help prevent recurrent AOE.
Malignant otitis externa
Malignant, or necrotizing, otitis externa is an aggressive disease form of otitis externa that is most common in individuals with diabetes or other immunodeficiency disorders.9 Most cases are due to infection with P aeruginosa.10 Prior to the availability of effective antibiotics, mortality rates in patients with necrotizing otitis externa were as high as 50%.11
What you’ll see. Patients typically present with severe ear pain, otorrhea, conductive hearing loss, and a feeling of fullness in the external ear canal. Physical examination reveals purulent otorrhea and a swollen, tender ear canal. Exposed bone may be visible, most often on the floor of the canal. The tympanic membrane and middle ear are seldom involved on initial presentation.
The infection often originates at the junction of the bony and cartilaginous portion of the external canal, spreading through the fissures of Santorini to the skull base. If not aggressively treated, the infection spreads medially to the tympanomastoid suture causing intracranial complications—usually a facial nerve neuropathy.
Continue to: Given these clinical findings...
Given these clinical findings, promptly order laboratory studies and imaging to confirm the diagnosis. The erythrocyte sedimentation rate and C-reactive protein level are typically elevated, and either can be used as a marker to follow treatment. Computed tomography (CT) helps to determine the location and extent of disease and is recommended as the initial diagnostic imaging modality for patients with suspected malignant otitis externa.12
Magnetic resonance imaging helps define soft-tissue changes, dural enhancement, and involvement of medullary bone, making this the preferred modality to monitor therapeutic response.12 Technetium bone scanning can also be used for the initial diagnosis (particularly if CT findings are normal and clinical suspicion is high) and for follow-up with treatment.
How to treat. Management involves a team approach with otolaryngology, radiology, neurology, endocrinology, and infectious disease specialists. Long term (6-8 weeks) antipseudomonal antibiotic treatment is typical.
Let culture results guide the choice of antibiotic. Fluoroquinolone therapy, usually ciprofloxacin, is used most often.12 Surgical intervention may be required for local debridement and drainage of abscesses. Close follow-up is necessary due to reports of recurrence up to 1 year after treatment. If left untreated, necrotizing otitis externa can lead to osteomyelitis, meningitis, septic thrombosis, cerebral abscess, and death.11
Cerumen impaction
The relatively small diameter of the external auditory canal increases the risk for impaction of cerumen and foreign bodies. Cerumen impaction, in particular, is a common primary care complaint. Cerumen forms when glandular secretions from the outer two-thirds of the ear canal mix with exfoliated skin. It functions as a lubricant for the ear canal and as a barrier against infection, water accumulation, and foreign bodies.13
Continue to: What you'll see
What you’ll see. You may encounter cerumen impaction in an asymptomatic patient when it prevents visualization of the external auditory canal or tympanic membrane, or when a patient complains of conductive hearing loss, tinnitus, dizziness, ear pain, itching, and cough.13 It is found in 1 in 10 children and 1 in 20 adults.13 There is a higher incidence in patients who are elderly, are cognitively impaired, or wear hearing devices or ear plugs.13,14 Asymptomatic cerumen impaction should not be treated. A recent clinical guideline provides a useful “do and don’t” list for patient education (TABLE).13
How to treat. In asymptomatic patients, the presence of cerumen on examination is not an indication for removal. Based on current guidelines,13 impacted cerumen can safely be removed from the ear canal of symptomatic patients in several ways:
- Manual removal with cerumen loop/spoon or alligator forceps. This method decreases the risk for infection because it limits moisture exposure. However, it should be performed by a health care provider trained in its use because of the risk for trauma to the ear canal and tympanic membrane.
- Irrigation of the ear using tap water or a 50-50 solution of hydrogen peroxide and water. Irrigation can be achieved with a syringe or jet irrigator using a modified tip. This method also has a risk for trauma to the ear canal and tympanic membrane and should only be performed by appropriately trained health care professionals.
- Use of cerumenolytic agents to soften and thin earwax and promote natural extrusion. Several types of cerumenolytic drops (water-based and oil-based) are available and appear to be equally effective. Water-based solutions contain hydrogen peroxide, docusate sodium, acetic acid, and sodium bicarbonate. Oil-based drops may contain peanut, almond, or olive oils. A thorough allergic history should be performed to avoid using products in patients with nut allergies. In head-to-head laboratory comparisons, distilled water appears to be the best cerumenolytic.15
Foreign bodies
Foreign bodies in the external auditory canal (typically beads, cotton tips, and insects) are more common in children than adults.16
What you’ll see. Most foreign bodies are lodged in the bony part of the external auditory canal, and many patients try to remove the object before seeking medical care. Removal requires adequate visualization and skill.17 Although patients may be asymptomatic, most complain of pain, fullness, decreased hearing, or otorrhea.
How to treat. Directly visible objects can often be removed without referral. Suction, irrigation, forceps, probes, and fine hooks have been used. Insect removal can be facilitated by first flooding the canal with xylocaine, alcohol, or mineral oil. Acetone may be used to dissolve foreign bodies containing Styrofoam or to loosen glues. If the object is a button battery, avoid irrigation to prevent liquefaction tissue necrosis.
Continue to: Complications of foreign body removal...
Complications of foreign body removal include pain, otitis externa, otitis media, and trauma to the ear or tympanic membrane. The likelihood of successful removal of the object decreases and the risk for complications increases with each subsequent attempt.17 Consult an otolaryngologist if sedation or anesthesia is required, the foreign body is tightly wedged, there is trauma to the ear canal or tympanic membrane, the foreign body has a sharp edge (eg, glass or wire), or removal attempts have been unsuccessful.
Trauma
Sports injuries, motor vehicle accidents, bites, falls, and burns are the primary causes of trauma to the external ear.18
What you’ll see. Blunt auricular trauma predisposes to infection, necrosis, and scar contracture. One of the most common sequelae is cauliflower ear. Trauma is particularly common with contact sports such as boxing, wrestling, or mixed martial arts. The skin of the auricle attaches directly to the perichondrium. Following blunt or shearing trauma to the auricle, hematomas form within the space between the perichondrium and cartilage of the anterior ear.19
How to treat. Small hematomas can be managed by aspiration, while larger ones generally require open drainage.20 Newer treatments involving pressure dressings and the use of fibrin glue have been proposed.20 Recommend that athletes participating in contact sports wear appropriate protective headgear to prevent auricular hematoma and cauliflower ear.
Neoplasm
Roughly 5% of all skin cancers involve the ear, most frequently the pinna due to chronic sun exposure.21 The most frequently occurring malignancy of the external ear is basal cell carcinoma (BCC), which is responsible for 80% of all nonmelanoma skin cancers.22
Continue to: What you'll see
What you’ll see. BCC of the ear usually involves the preauricular area and the helix. The risk for BCC is related to exposure to ultraviolet radiation. BCC of the ear is more common in men and can be particularly aggressive, highlighting the importance of prevention and prompt recognition. BCC typically presents as a fleshy papule that is often translucent or “pearly’” and has overlying telangiectasia and a “rolled” border. Central ulceration can occur as well.
How to treat. Usual treatment of BCC is surgical excision. Prevention is critical and centers on sun avoidance or the use of appropriate sunscreens.
In addition to BCC, exposure of the external ear to sunlight and ultraviolet radiation predisposes patients to the development of squamous cell carcinoma (SCC) and melanoma. SCC has a variety of presentations including papules, plaques, and nodules. SCC has a higher metastatic potential than does BCC.
Keloid
Keloids are an abnormal healing response to soft-tissue injury: benign fibrocartilaginous growths that extend beyond the original wound.
What you’ll see. Keloids are more common in dark-skinned individuals and tend to result from burns, surgical incisions, infection, trauma, tattooing, injections, piercings, and arthropod bites. In some cases, they arise spontaneously. Keloids are more common in areas of increased skin tension (chest, shoulders, back), but may occur on the ears—most commonly after piercing or trauma. Keloids present clinically as slow-growing rubbery or firm nodules. The diagnosis is typically based on clinical appearance but can be confirmed by histopathology.
Continue to: How to treat
How to treat. Treatments vary and include observation, excision, intralesional injections, cryotherapy, enzyme therapy, silicone gel application, and irradiation.23 Recurrence is common; no therapy has been proven to be universally superior or preferred.
Congenital malformations
Atresia
Disruption of embryologic development (failed invagination of the external auditory canal) can lead to a stenotic or absent ear canal (aural atresia). Aural atresia is also often associated with fusion of the incus and malleus. This condition occurs predominantly in males. Unilateral atresia is more common than bilateral atresia, and the right ear is more often involved than the left.24
Microtia
Microtia is the incomplete development of the pinna leading to a small or deformed pinna. Microtia can be unilateral or bilateral. As with atresia, microtia more commonly affects males and, if unilateral, the right side is more often affected than the left. Microtia can occur in isolation but is often associated with genetic syndromes such as Treacher Collins syndrome and craniofacial microsomia (Goldenhar syndrome). When microtia is identified (typically at birth or early infancy), audiologic testing and a thorough physical examination for evidence of associated defects should be performed. Consult with an audiologist, clinical geneticist, or pediatric otolaryngologist.
Pre-auricular pits
Pre-auricular pits (sinuses) are tiny indentations anterior to the helix and superior to the tragus. While pre-auricular pits are more common on the right side, they are bilateral in 25% to 50% of cases.25 Pre-auricular pits occur in up to 1% of white children, 5% of black children, and 10% of Asian children.25 Children with this condition should undergo formal audiologic testing as their risk for hearing loss is higher compared with the general population.26
The branchio-oto-renal syndrome (associated with pre-auricular pits and hearing loss) also features structural defects of the ear, renal anomalies and/or nasolacrimal duct stenosis or fistulas. If this syndrome is suspected, renal ultrasound imaging is warranted. Other indications for renal ultrasound in patients with a pre-auricular pit are any dysmorphic feature, a family history of deafness, an auricular malformation, or a maternal history of gestational diabetes.27 Pre-auricular pits do not require surgery unless they drain chronically or become recurrently infected. Complete surgical excision is the treatment of choice in these cases.
CORRESPONDENCE
Mark Stephens, MD, 1850 Park Avenue, State College, PA 16801; mstephens3@pennstatehealth.psu.edu
1. Cox TC, Camci ED, Vora S, et al. The genetics of auricular development and malformation: new findings in model systems driving future directions for microtia research. Eur J Med Genet. 2014;57:394-401.
2. Sosin M, Weissler JM, Pulcrano M, et al. Transcartilaginous ear piercing and infectious complications: a systematic review and critical analysis of outcomes. Laryngoscope. 2015;125:1827-1834.
3. Stirn A. Body piercing: medical consequences and psychological motivations. Lancet. 2003;361:1205-1215.
4. Liu ZW, Chokkalingam P. Piercing associated perichondritis of the pinna: are we treating it correctly? J Larygol Oncol. 2013;127:505-508.
5. Mitchell S, Ditta K, Minhas S, et al. Pinna abscesses: can we manage them better? A case series and review of the literature. Eur Arch Otorhinolaryngol. 2015;272:3163-3167.
6. Stone KE. Otitis externa. Pediatr Rev. 2007;28:77-78.
7. Rosenfeld RM, Schwartz SR, Cannon CR, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2014;150(1 suppl):S1-S24.
8. Prentice P. American Academy of Otolaryngology: Head and Neck Surgery Foundation clinical practice guideline on acute otitis externa. Arch Dis Child Educ Pract Ed. 2015;100:197.
9. Unadkat S, Kanzara T, Watters G. Necrotising otitis externa in the immunocompetent patient. J Laryngol Otol. 2018;132:71-74.
10. Carfrae MJ, Kesser BW. Malignant otitis externa. Otolarngol Clin N Am. 2008;41:537-549.
11. Chandler JR, Malignant otitis externa. Laryngoscope. 1968;78:1257-1294.
12. Hollis S, Evans K. Management of malignant (necrotising) otitis externa. J Laryngol Otol. 2011;125:1212-1217.
13. Schwartz SR, Magit AE, Rosenfeld RM, et al. Clinical practice guideline (update): earwax (cerumen impaction). Otolaryngol Head Neck Surg. 2017;156:S1-S29.
14. Guest JF, Greener MJ, Robinson AC, et al. Impacted cerumen: composition, production, epidemiology and management. QJM. 2004;97:477-488.
15. Saxby C, Williams R, Hickey S. Finding the most effective cerumenolytic. J Laryngol Otol. 2013;127:1067-1070.
16. Awad AH, ElTaher M. ENT foreign bodies: an experience. Int Arch Otorhinolaryngol. 2018;22:146-151.
17. Heim SW, Maughan KL. Foreign bodies in the ear, nose, and throat. Am Fam Physician. 2007;76:1185-1189.
18. Sharma K, Goswami SC, Baruah DK. Auricular trauma and its management. Indian J Otolaryngol Head Neck Surg. 2006;58:232-234.
19. Haik J, Givol O, Kornhaber R, et al. Cauliflower ear–a minimally invasive treatment in a wrestling athlete: a case report. Int Med Case Rep J. 2018;11:5-7.
20. Ebrahimi A, Kazemi A, Rasouli HR, et al. Reconstructive surgery of auricular defects: an overview. Trauma Mon. 2015;20:e28202.
21. Warner E, Weston C, Barclay-Klingle N, et al. The swollen pinna. BMJ. 2017; 359; j5073.
22. Rubin AI, Chen EH, Ratner D. Basal cell carcinoma. N Engl J Med. 2005;353:2262-2269.
23. Ranjan SK, Ahmed A, Harsh V, et al. Giant bilateral keloids of the ear lobule: case report and brief review of the literature. J Family Med Prim Care. 2017;6:677-679.
24. Roland PS, Marple BF. Disorders of the external auditory canal. J Am Acad Audiol. 1997;8:367-378.
25. Scheinfeld NS, Silverberg NB, Weinberg JM, et al. The preauricular sinus: a review of its clinical presentation, treatment, and associations. Pediatr Dermatol. 2004;21:191-196.
26. Roth DA, Hildesheimer M, Bardestein S, et al. Preauricular skin tags and ear pits are associated with permanent hearing impairment in newborns. Pediatrics. 2008;122:e884-890.
27. Tan T, Constantinides H, Mitchell TE. The preauricular sinus: a review of its aetiology, clinical presentation and management. Int J Ped Otorhinolaryngol. 2005;69:1469-1474.
1. Cox TC, Camci ED, Vora S, et al. The genetics of auricular development and malformation: new findings in model systems driving future directions for microtia research. Eur J Med Genet. 2014;57:394-401.
2. Sosin M, Weissler JM, Pulcrano M, et al. Transcartilaginous ear piercing and infectious complications: a systematic review and critical analysis of outcomes. Laryngoscope. 2015;125:1827-1834.
3. Stirn A. Body piercing: medical consequences and psychological motivations. Lancet. 2003;361:1205-1215.
4. Liu ZW, Chokkalingam P. Piercing associated perichondritis of the pinna: are we treating it correctly? J Larygol Oncol. 2013;127:505-508.
5. Mitchell S, Ditta K, Minhas S, et al. Pinna abscesses: can we manage them better? A case series and review of the literature. Eur Arch Otorhinolaryngol. 2015;272:3163-3167.
6. Stone KE. Otitis externa. Pediatr Rev. 2007;28:77-78.
7. Rosenfeld RM, Schwartz SR, Cannon CR, et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2014;150(1 suppl):S1-S24.
8. Prentice P. American Academy of Otolaryngology: Head and Neck Surgery Foundation clinical practice guideline on acute otitis externa. Arch Dis Child Educ Pract Ed. 2015;100:197.
9. Unadkat S, Kanzara T, Watters G. Necrotising otitis externa in the immunocompetent patient. J Laryngol Otol. 2018;132:71-74.
10. Carfrae MJ, Kesser BW. Malignant otitis externa. Otolarngol Clin N Am. 2008;41:537-549.
11. Chandler JR, Malignant otitis externa. Laryngoscope. 1968;78:1257-1294.
12. Hollis S, Evans K. Management of malignant (necrotising) otitis externa. J Laryngol Otol. 2011;125:1212-1217.
13. Schwartz SR, Magit AE, Rosenfeld RM, et al. Clinical practice guideline (update): earwax (cerumen impaction). Otolaryngol Head Neck Surg. 2017;156:S1-S29.
14. Guest JF, Greener MJ, Robinson AC, et al. Impacted cerumen: composition, production, epidemiology and management. QJM. 2004;97:477-488.
15. Saxby C, Williams R, Hickey S. Finding the most effective cerumenolytic. J Laryngol Otol. 2013;127:1067-1070.
16. Awad AH, ElTaher M. ENT foreign bodies: an experience. Int Arch Otorhinolaryngol. 2018;22:146-151.
17. Heim SW, Maughan KL. Foreign bodies in the ear, nose, and throat. Am Fam Physician. 2007;76:1185-1189.
18. Sharma K, Goswami SC, Baruah DK. Auricular trauma and its management. Indian J Otolaryngol Head Neck Surg. 2006;58:232-234.
19. Haik J, Givol O, Kornhaber R, et al. Cauliflower ear–a minimally invasive treatment in a wrestling athlete: a case report. Int Med Case Rep J. 2018;11:5-7.
20. Ebrahimi A, Kazemi A, Rasouli HR, et al. Reconstructive surgery of auricular defects: an overview. Trauma Mon. 2015;20:e28202.
21. Warner E, Weston C, Barclay-Klingle N, et al. The swollen pinna. BMJ. 2017; 359; j5073.
22. Rubin AI, Chen EH, Ratner D. Basal cell carcinoma. N Engl J Med. 2005;353:2262-2269.
23. Ranjan SK, Ahmed A, Harsh V, et al. Giant bilateral keloids of the ear lobule: case report and brief review of the literature. J Family Med Prim Care. 2017;6:677-679.
24. Roland PS, Marple BF. Disorders of the external auditory canal. J Am Acad Audiol. 1997;8:367-378.
25. Scheinfeld NS, Silverberg NB, Weinberg JM, et al. The preauricular sinus: a review of its clinical presentation, treatment, and associations. Pediatr Dermatol. 2004;21:191-196.
26. Roth DA, Hildesheimer M, Bardestein S, et al. Preauricular skin tags and ear pits are associated with permanent hearing impairment in newborns. Pediatrics. 2008;122:e884-890.
27. Tan T, Constantinides H, Mitchell TE. The preauricular sinus: a review of its aetiology, clinical presentation and management. Int J Ped Otorhinolaryngol. 2005;69:1469-1474.
PRACTICE RECOMMENDATIONS
› Prescribe topical antibiotics for uncomplicated otitis externa, reserving systemic agents for infection extending outside the ear canal, necrotizing otitis externa, or patients who are immunodeficient. C
› Avoid clearing cerumen if a patient is asymptomatic and advise patients/parents on Do’s and Don’ts for ear wax accumulation. C
› Consider flooding the ear canal with xylocaine, alcohol, or mineral oil before attempting insect removal. C
Strength of recommendation (SOR)
A Good-quality patient-oriented evidence
B Inconsistent or limited-quality patient-oriented evidence
C Consensus, usual practice, opinion, disease-oriented evidence, case series
Managing amidst COVID-19 (and everything else that ails us)
This year, medical media has been dominated by reporting on the devastating COVID-19 pandemic. Many studies and analyses have shown that staying at home, social distancing, quarantining of close contacts, and wearing face masks and face shields are effective ways of preventing spread.
Although initially there were no known effective treatments for severe COVID-19 infection (other than oxygen and ventilator support), we now know that dexamethasone,1 remdesivir,2 and convalescent plasma3 are effective in lessening the severity of illness and perhaps preventing death. That said, we will continue to struggle with COVID-19 for the foreseeable future.
But other medical illnesses actually predominate in terms of morbidity and mortality, even during this pandemic. For example, although there has been an average of roughly 5600 COVID-19-related deaths per week for the past 4 months,4 there are, on average, more than 54,000 deaths per week in the United States from other causes.5 This means that we must continue to tend to the other health care needs of our patients even as we deal with COVID-19.
In that light, JFP continues to publish practical, evidence-based clinical reviews designed to keep family physicians and other primary health care clinicians up to date on a variety of topics. For instance, in this issue of JFP, we have articles on:
- Opioid prescribing. Although opioids have risks, they remain potent medications for relief from acute pain, as well as cancer-related pain and chronic pain not sufficiently treated with other medications. Mahvan et al provide expert advice on maximizing benefit and minimizing the risks of opioid prescribing.
- Secondary ischemic stroke prevention. For patients who have suffered a transient ischemic attack or minor stroke, a mainstay of prevention is antiplatelet therapy. Aspirin alone used to be the treatment of choice, but research has demonstrated the value of adding another antiplatelet agent. Helmer et al’s thorough review reminds us that the antiplatelet drug of choice, in addition to aspirin, is clopidogrel, which should be used only for the first 30 days after the event because of an increased bleeding risk.
- Combatting Clostridioides difficile infection. CDI has been a difficult condition to treat, especially in high-risk patients. Zukauckas et al provide a comprehensive review of diagnosis and management. Vancomycin is now the drug of choice, and fecal transplant is highly effective in preventing recurrent CDI.
This diverse range of timely, practical, evidence-based guidance—in addition to coverage of COVID-19 and other rapidly emerging medical news stories—can all be found on our Web site at www.mdedge.com/familymedicine. We remain committed to supplying you with all of the information you need to provide your patients with the very best care—no matter what brings them in to see you.
1. Low-cost dexamethasone reduces death by up to one third in hospitalized patients with severe respiratory complications of COVID-19. Recovery: Randomised Evaluation of COVID-19 Therapy Web site. June 16, 2020. www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed July 1, 2020.
2. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print]. N Engl J Med. doi: 10.1056/NEJMoa2007764.
3. Li L, Zhang W, Hu Y, et. al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print]. JAMA. doi:10.1001/jama.2020.10044.
4. Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
5. Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2018. NCHS Data Brief. 2020;1-8.
This year, medical media has been dominated by reporting on the devastating COVID-19 pandemic. Many studies and analyses have shown that staying at home, social distancing, quarantining of close contacts, and wearing face masks and face shields are effective ways of preventing spread.
Although initially there were no known effective treatments for severe COVID-19 infection (other than oxygen and ventilator support), we now know that dexamethasone,1 remdesivir,2 and convalescent plasma3 are effective in lessening the severity of illness and perhaps preventing death. That said, we will continue to struggle with COVID-19 for the foreseeable future.
But other medical illnesses actually predominate in terms of morbidity and mortality, even during this pandemic. For example, although there has been an average of roughly 5600 COVID-19-related deaths per week for the past 4 months,4 there are, on average, more than 54,000 deaths per week in the United States from other causes.5 This means that we must continue to tend to the other health care needs of our patients even as we deal with COVID-19.
In that light, JFP continues to publish practical, evidence-based clinical reviews designed to keep family physicians and other primary health care clinicians up to date on a variety of topics. For instance, in this issue of JFP, we have articles on:
- Opioid prescribing. Although opioids have risks, they remain potent medications for relief from acute pain, as well as cancer-related pain and chronic pain not sufficiently treated with other medications. Mahvan et al provide expert advice on maximizing benefit and minimizing the risks of opioid prescribing.
- Secondary ischemic stroke prevention. For patients who have suffered a transient ischemic attack or minor stroke, a mainstay of prevention is antiplatelet therapy. Aspirin alone used to be the treatment of choice, but research has demonstrated the value of adding another antiplatelet agent. Helmer et al’s thorough review reminds us that the antiplatelet drug of choice, in addition to aspirin, is clopidogrel, which should be used only for the first 30 days after the event because of an increased bleeding risk.
- Combatting Clostridioides difficile infection. CDI has been a difficult condition to treat, especially in high-risk patients. Zukauckas et al provide a comprehensive review of diagnosis and management. Vancomycin is now the drug of choice, and fecal transplant is highly effective in preventing recurrent CDI.
This diverse range of timely, practical, evidence-based guidance—in addition to coverage of COVID-19 and other rapidly emerging medical news stories—can all be found on our Web site at www.mdedge.com/familymedicine. We remain committed to supplying you with all of the information you need to provide your patients with the very best care—no matter what brings them in to see you.
This year, medical media has been dominated by reporting on the devastating COVID-19 pandemic. Many studies and analyses have shown that staying at home, social distancing, quarantining of close contacts, and wearing face masks and face shields are effective ways of preventing spread.
Although initially there were no known effective treatments for severe COVID-19 infection (other than oxygen and ventilator support), we now know that dexamethasone,1 remdesivir,2 and convalescent plasma3 are effective in lessening the severity of illness and perhaps preventing death. That said, we will continue to struggle with COVID-19 for the foreseeable future.
But other medical illnesses actually predominate in terms of morbidity and mortality, even during this pandemic. For example, although there has been an average of roughly 5600 COVID-19-related deaths per week for the past 4 months,4 there are, on average, more than 54,000 deaths per week in the United States from other causes.5 This means that we must continue to tend to the other health care needs of our patients even as we deal with COVID-19.
In that light, JFP continues to publish practical, evidence-based clinical reviews designed to keep family physicians and other primary health care clinicians up to date on a variety of topics. For instance, in this issue of JFP, we have articles on:
- Opioid prescribing. Although opioids have risks, they remain potent medications for relief from acute pain, as well as cancer-related pain and chronic pain not sufficiently treated with other medications. Mahvan et al provide expert advice on maximizing benefit and minimizing the risks of opioid prescribing.
- Secondary ischemic stroke prevention. For patients who have suffered a transient ischemic attack or minor stroke, a mainstay of prevention is antiplatelet therapy. Aspirin alone used to be the treatment of choice, but research has demonstrated the value of adding another antiplatelet agent. Helmer et al’s thorough review reminds us that the antiplatelet drug of choice, in addition to aspirin, is clopidogrel, which should be used only for the first 30 days after the event because of an increased bleeding risk.
- Combatting Clostridioides difficile infection. CDI has been a difficult condition to treat, especially in high-risk patients. Zukauckas et al provide a comprehensive review of diagnosis and management. Vancomycin is now the drug of choice, and fecal transplant is highly effective in preventing recurrent CDI.
This diverse range of timely, practical, evidence-based guidance—in addition to coverage of COVID-19 and other rapidly emerging medical news stories—can all be found on our Web site at www.mdedge.com/familymedicine. We remain committed to supplying you with all of the information you need to provide your patients with the very best care—no matter what brings them in to see you.
1. Low-cost dexamethasone reduces death by up to one third in hospitalized patients with severe respiratory complications of COVID-19. Recovery: Randomised Evaluation of COVID-19 Therapy Web site. June 16, 2020. www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed July 1, 2020.
2. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print]. N Engl J Med. doi: 10.1056/NEJMoa2007764.
3. Li L, Zhang W, Hu Y, et. al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print]. JAMA. doi:10.1001/jama.2020.10044.
4. Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
5. Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2018. NCHS Data Brief. 2020;1-8.
1. Low-cost dexamethasone reduces death by up to one third in hospitalized patients with severe respiratory complications of COVID-19. Recovery: Randomised Evaluation of COVID-19 Therapy Web site. June 16, 2020. www.recoverytrial.net/news/low-cost-dexamethasone-reduces-death-by-up-to-one-third-in-hospitalised-patients-with-severe-respiratory-complications-of-covid-19. Accessed July 1, 2020.
2. Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19—preliminary report [published online ahead of print]. N Engl J Med. doi: 10.1056/NEJMoa2007764.
3. Li L, Zhang W, Hu Y, et. al. Effect of convalescent plasma therapy on time to clinical improvement in patients with severe and life-threatening COVID-19: a randomized clinical trial [published online ahead of print]. JAMA. doi:10.1001/jama.2020.10044.
4. Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance—United States, January 22–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:759-765.
5. Xu J, Murphy SL, Kochanek KD, et al. Mortality in the United States, 2018. NCHS Data Brief. 2020;1-8.
Early screening may halve breast cancer mortality in childhood cancer survivors
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
Two strategies – annual mammography with MRI and annual MRI alone – at least halved breast cancer mortality when started at the ages of 25 or 30 years.
Jennifer M. Yeh, PhD, of Harvard Medical School in Boston and colleagues reported these results in the Annals of Internal Medicine.
When cost was also considered, 30 years emerged as the preferred starting age, dropping the incremental cost-effectiveness ratio (ICER) below the generally accepted threshold of $100,000 per quality-adjusted life-year gained.
“Our findings underscore the importance of making sure that young women previously treated with chest radiation are informed about their elevated breast cancer risk and the benefits of routine screening. Both primary care providers and oncologists who care for survivors should discuss breast cancer screening with these patients,” Dr. Yeh and colleagues wrote.
“Screening guidelines should emphasize the importance of MRI screening (with or without mammography) among survivors,” the authors recommended. “Our findings also highlight the importance of ensuring that survivors have access to health insurance coverage for MRI screening.”
Implications for awareness, coverage
“My hope is that, by showing the significantly decreased risk of death associated with early breast cancer screening, with harm-benefit ratios considerably lower than benchmarks for average-risk women, this study will help health insurance companies see the benefit in covering early screening for at-risk survivors,” commented Karen E. Effinger, MD, of Emory University, Atlanta, and the Aflac Cancer & Blood Disorders Center at Children’s Healthcare of Atlanta.
“In many survivors, the cost of current screening [as recommended by] guidelines is prohibitive,” added Dr. Effinger, who was not involved in the current study.
The main concern regarding the study’s findings is generalizability to the contemporary era, given the use of a cohort diagnosed and treated decades ago and changes in radiation techniques and dosing since then, she noted in an interview. This limitation was addressed in a sensitivity analysis that halved the women’s base-case lifetime risk of breast cancer and still netted similar results.
“However, it will take many years to determine the true risk reduction of our current treatment strategies,” Dr. Effinger acknowledged.
“It is crucial that we improve our education of both survivors and our colleagues who care for these survivors, especially in regard to risk of subsequent malignancies and the benefits of screening,” Dr. Effinger maintained. “While many people are aware of the risk of breast cancer associated with BRCA mutations, the increased risk in survivors of childhood cancer is not as recognized by nononcologists. This study reinforces that increasing this awareness can save lives.”
In educating their patients about preventive care, health care providers must strike “a fine balance between discussing the risks and benefits of screening without provoking significant anxiety,” she concluded. “It is important for survivors to establish care with a primary care provider in order to develop trust and receive the guidance they need to decrease the risk of early mortality.”
Study details
Dr. Yeh and colleagues developed models to compare outcomes with various screening strategies among women aged 20 years who had received chest radiotherapy for childhood cancer during 1970-1986. The women had been diagnosed with Hodgkin lymphoma (55%), Wilms tumor (12%), non-Hodgkin lymphoma (8%), and other cancers.
The investigators conducted their analysis using data from the Childhood Cancer Survivor Study and other published sources, a lifetime time horizon, and a payer perspective.
The team assessed three strategies: no screening; digital mammography with MRI screening starting at 25 years of age (the current Children’s Oncology Group recommendation), 30 years, or 35 years and continuing to 74 years of age; and MRI only starting at age 25, 30, or 35 years and continuing to age 74 years.
The main study results showed that, without screening, women who had received chest radiation for childhood cancer had a 10%-11% lifetime risk of breast cancer mortality across models.
Relative to no screening, starting at age 25 years, the largest share of deaths was averted with the strategy of annual mammography with MRI – 56.3%-71.2% – or with the strategy of annual MRI alone – 55.7%-62.0%.
These two strategies also yielded the most screening tests, as well as the most false-positive test results and benign biopsy results.
For women who started screening at age 25, there were 4,188-4,879 false-positive test results per 1,000 women for mammography plus MRI and 3,283-3,764 false-positive results per 1,000 women for MRI alone.
For women who started screening at age 25, there were 1,340-1,561 benign biopsy results per 1,000 women for mammography plus MRI and 1,248-1,430 benign results per 1,000 women for MRI alone.
After cost was factored in, beginning screening at age 30 emerged as the preferred strategy to achieve an ICER threshold of less than $100,000 per quality-adjusted life-year gained.
When started at 30 years of age, annual mammography with MRI averted 54.7%-68.8% of breast cancer deaths, with an ICER of $25,400-$113,200 per quality-adjusted life-year gained. Annual MRI alone averted 54.0%-60.0% of breast cancer deaths, with an ICER of $21,800-$50,580 per quality-adjusted life-year gained.
This research was supported by grants from the National Cancer Institute, American Cancer Society, and American Lebanese Syrian Associated Charities. The authors disclosed relationships with GE Healthcare and Biovector. Dr. Effinger disclosed no relevant conflicts of interest.
SOURCE: Yeh JM et al. Ann Intern Med. 2020 Jul 7. doi: 10.7326/M19-3481.
FROM ANNALS OF INTERNAL MEDICINE
Local analgesia before prolapse surgery may not be needed to reduce postop pain
Preoperative pelvic floor muscle injections and pudendal nerve blocks with bupivacaine and dexamethasone do not significantly improve pain control after vaginal apical prolapse repair, compared with placebo, according to a study.
In a randomized trial, patients generally reported mild postoperative pain and low dosages of narcotic use. “The majority reported that they returned to their baseline activity by 2 weeks after surgery, which should be reassuring to similar urogynecology patient populations,” said Lauren Giugale, MD.
Although many gynecologic surgeries increasingly are performed as outpatient procedures, patients may have inadequate pain control and persistently use narcotics after surgery. In an effort to reduce postoperative pain, doctors have tried preemptive analgesia with various local anesthetic techniques. These approaches have had mixed results, however, and there is “no consensus on the ideal local anesthetic technique to reduce postoperative pain after vaginal reconstructive surgery,” said Dr. Giugale, of the University of Pittsburgh.
To evaluate whether preoperative pelvic floor muscle injections and pudendal nerve blocks with bupivacaine and dexamethasone improve postoperative pain control after vaginal apical prolapse repairs, Dr. Giugale and colleagues conducted a three-arm, double-blind trial that included 75 patients. Patients received placebo (normal saline), bupivacaine alone, or bupivacaine combined with 4 mg of dexamethasone at four injection sites.
Dr. Giugale presented the study results at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
A range of procedures
Participants received bilateral levator ani muscle injections via a transobturator approach and pudendal nerve blocks via a transvaginal approach. They received the injections – 5 mL at each site – after the administration of general anesthesia but before the start of surgery. “Anecdotally, we have had good success” with the transobturator approach to treating chronic pelvic pain, which was part of the rationale for the trial, said Dr. Giugale.
The study included women 18 years or older who were scheduled for a vaginal native tissue repair with apical support. Participants had to be able to tolerate general anesthesia with a standardized enhanced recovery after surgery (ERAS) protocol. The investigators excluded women undergoing mesh-augmented prolapse repairs or abdominal surgery and those with chronic pelvic pain or immunosuppression.
Each treatment arm had 25 patients. Patients had an average age of 69 years and an average body mass index of 27.5 kg/m2. Most patients were white, and demographic variables did not significantly differ among the groups.
“The distribution of prolapse procedures was similar among study groups, with colpocleisis being the most common, followed by uterosacral ligament suspension, levator myorrhaphy, and sacrospinous ligament fixation,” said Dr. Giugale. Rates of concomitant hysterectomy were similar for each group.
Before surgery, patients completed pain, nausea, and activities assessments. At 6 hours after surgery, they completed pain and nausea assessments. During postoperative days 1 through 3, patients documented pain scores and analgesic use. One week after surgery, patients completed pain and activities assessments. And at postoperative weeks 2, 6, and 12, they completed additional activities assessments. The assessments included validated handouts that patients completed at home, and no additional office visits were required.
The numeric rating scale pain score on the day after surgery was the primary outcome, and the median pain score did not significantly differ among the groups (3.75 in the placebo group, 4 in the bupivacaine group, and 3 in the bupivacaine plus dexamethasone group). Between-group differences in pain scores at other time points also were not significant.
Activities assessments, nausea and vomiting scores, the percentage of patients with same-day discharge, urinary retention, postoperative narcotic use as measured by oral morphine equivalents, and adverse events also did not significantly differ among the groups.
“One week after surgery, 52% of women reported that they were at or better than their baseline preoperative activity level, which increased to 70% at 2 weeks, 84% at 6 weeks, and 94% at 12 weeks,” Dr. Giugale said.
In all, 57% of patients used narcotic medicine the day after surgery, which decreased to 44% on day 3. The dosage was low, with a median oral morphine equivalent of 5 mg of oxycodone or less per day, she said.
Early postoperative pain may be influenced by procedure type, according to an exploratory analysis. Through the first postoperative day, “there was a trend toward more pain with uterosacral ligament suspension,” Dr. Giugale said. By day 3, sacrospinous ligament fixation was associated with significantly more postoperative pain.
The role of ERAS protocols
The heterogeneity of surgical procedures among the treatment groups and the use of a predefined ERAS protocol may have confounded the results. In addition, the researchers did not measure patient satisfaction, and the findings may not apply to different patient populations, Dr. Giugale noted.
“As more and more gynecologic surgery patients have surgery under these enhanced recovery protocols, maybe additional preemptive local analgesia for vaginal reconstructive surgery is not all that beneficial,” she said. “Maybe we are getting enough benefit from the enhanced [recovery] protocols themselves.”
The investigators studied a novel idea – dual local therapy for pain in patients undergoing pelvic floor surgery – and described a novel transobturator technique for levator injection, commented Sunil Balgobin, MD, associate director of the female pelvic medicine and reconstructive surgery fellowship at University of Texas Southwestern Medical Center, Dallas.
“For the current opioid problem, development of alternative pain control strategies is extremely important to reduce narcotic use and improve patient outcomes,” Dr. Balgobin said. The study “addresses an important gap in the literature, is relevant to surgeons performing vaginal apical procedures, and aims to advance research in this area for the potential benefit of ... patients.”
Interpretation of the results for individual procedure types may be limited by the smaller sample sizes, he added.
The researchers and Dr. Balgobin had no relevant financial disclosures.
SOURCE: Giugale L et al. SGS 2020, Abstract 10.
Preoperative pelvic floor muscle injections and pudendal nerve blocks with bupivacaine and dexamethasone do not significantly improve pain control after vaginal apical prolapse repair, compared with placebo, according to a study.
In a randomized trial, patients generally reported mild postoperative pain and low dosages of narcotic use. “The majority reported that they returned to their baseline activity by 2 weeks after surgery, which should be reassuring to similar urogynecology patient populations,” said Lauren Giugale, MD.
Although many gynecologic surgeries increasingly are performed as outpatient procedures, patients may have inadequate pain control and persistently use narcotics after surgery. In an effort to reduce postoperative pain, doctors have tried preemptive analgesia with various local anesthetic techniques. These approaches have had mixed results, however, and there is “no consensus on the ideal local anesthetic technique to reduce postoperative pain after vaginal reconstructive surgery,” said Dr. Giugale, of the University of Pittsburgh.
To evaluate whether preoperative pelvic floor muscle injections and pudendal nerve blocks with bupivacaine and dexamethasone improve postoperative pain control after vaginal apical prolapse repairs, Dr. Giugale and colleagues conducted a three-arm, double-blind trial that included 75 patients. Patients received placebo (normal saline), bupivacaine alone, or bupivacaine combined with 4 mg of dexamethasone at four injection sites.
Dr. Giugale presented the study results at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
A range of procedures
Participants received bilateral levator ani muscle injections via a transobturator approach and pudendal nerve blocks via a transvaginal approach. They received the injections – 5 mL at each site – after the administration of general anesthesia but before the start of surgery. “Anecdotally, we have had good success” with the transobturator approach to treating chronic pelvic pain, which was part of the rationale for the trial, said Dr. Giugale.
The study included women 18 years or older who were scheduled for a vaginal native tissue repair with apical support. Participants had to be able to tolerate general anesthesia with a standardized enhanced recovery after surgery (ERAS) protocol. The investigators excluded women undergoing mesh-augmented prolapse repairs or abdominal surgery and those with chronic pelvic pain or immunosuppression.
Each treatment arm had 25 patients. Patients had an average age of 69 years and an average body mass index of 27.5 kg/m2. Most patients were white, and demographic variables did not significantly differ among the groups.
“The distribution of prolapse procedures was similar among study groups, with colpocleisis being the most common, followed by uterosacral ligament suspension, levator myorrhaphy, and sacrospinous ligament fixation,” said Dr. Giugale. Rates of concomitant hysterectomy were similar for each group.
Before surgery, patients completed pain, nausea, and activities assessments. At 6 hours after surgery, they completed pain and nausea assessments. During postoperative days 1 through 3, patients documented pain scores and analgesic use. One week after surgery, patients completed pain and activities assessments. And at postoperative weeks 2, 6, and 12, they completed additional activities assessments. The assessments included validated handouts that patients completed at home, and no additional office visits were required.
The numeric rating scale pain score on the day after surgery was the primary outcome, and the median pain score did not significantly differ among the groups (3.75 in the placebo group, 4 in the bupivacaine group, and 3 in the bupivacaine plus dexamethasone group). Between-group differences in pain scores at other time points also were not significant.
Activities assessments, nausea and vomiting scores, the percentage of patients with same-day discharge, urinary retention, postoperative narcotic use as measured by oral morphine equivalents, and adverse events also did not significantly differ among the groups.
“One week after surgery, 52% of women reported that they were at or better than their baseline preoperative activity level, which increased to 70% at 2 weeks, 84% at 6 weeks, and 94% at 12 weeks,” Dr. Giugale said.
In all, 57% of patients used narcotic medicine the day after surgery, which decreased to 44% on day 3. The dosage was low, with a median oral morphine equivalent of 5 mg of oxycodone or less per day, she said.
Early postoperative pain may be influenced by procedure type, according to an exploratory analysis. Through the first postoperative day, “there was a trend toward more pain with uterosacral ligament suspension,” Dr. Giugale said. By day 3, sacrospinous ligament fixation was associated with significantly more postoperative pain.
The role of ERAS protocols
The heterogeneity of surgical procedures among the treatment groups and the use of a predefined ERAS protocol may have confounded the results. In addition, the researchers did not measure patient satisfaction, and the findings may not apply to different patient populations, Dr. Giugale noted.
“As more and more gynecologic surgery patients have surgery under these enhanced recovery protocols, maybe additional preemptive local analgesia for vaginal reconstructive surgery is not all that beneficial,” she said. “Maybe we are getting enough benefit from the enhanced [recovery] protocols themselves.”
The investigators studied a novel idea – dual local therapy for pain in patients undergoing pelvic floor surgery – and described a novel transobturator technique for levator injection, commented Sunil Balgobin, MD, associate director of the female pelvic medicine and reconstructive surgery fellowship at University of Texas Southwestern Medical Center, Dallas.
“For the current opioid problem, development of alternative pain control strategies is extremely important to reduce narcotic use and improve patient outcomes,” Dr. Balgobin said. The study “addresses an important gap in the literature, is relevant to surgeons performing vaginal apical procedures, and aims to advance research in this area for the potential benefit of ... patients.”
Interpretation of the results for individual procedure types may be limited by the smaller sample sizes, he added.
The researchers and Dr. Balgobin had no relevant financial disclosures.
SOURCE: Giugale L et al. SGS 2020, Abstract 10.
Preoperative pelvic floor muscle injections and pudendal nerve blocks with bupivacaine and dexamethasone do not significantly improve pain control after vaginal apical prolapse repair, compared with placebo, according to a study.
In a randomized trial, patients generally reported mild postoperative pain and low dosages of narcotic use. “The majority reported that they returned to their baseline activity by 2 weeks after surgery, which should be reassuring to similar urogynecology patient populations,” said Lauren Giugale, MD.
Although many gynecologic surgeries increasingly are performed as outpatient procedures, patients may have inadequate pain control and persistently use narcotics after surgery. In an effort to reduce postoperative pain, doctors have tried preemptive analgesia with various local anesthetic techniques. These approaches have had mixed results, however, and there is “no consensus on the ideal local anesthetic technique to reduce postoperative pain after vaginal reconstructive surgery,” said Dr. Giugale, of the University of Pittsburgh.
To evaluate whether preoperative pelvic floor muscle injections and pudendal nerve blocks with bupivacaine and dexamethasone improve postoperative pain control after vaginal apical prolapse repairs, Dr. Giugale and colleagues conducted a three-arm, double-blind trial that included 75 patients. Patients received placebo (normal saline), bupivacaine alone, or bupivacaine combined with 4 mg of dexamethasone at four injection sites.
Dr. Giugale presented the study results at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
A range of procedures
Participants received bilateral levator ani muscle injections via a transobturator approach and pudendal nerve blocks via a transvaginal approach. They received the injections – 5 mL at each site – after the administration of general anesthesia but before the start of surgery. “Anecdotally, we have had good success” with the transobturator approach to treating chronic pelvic pain, which was part of the rationale for the trial, said Dr. Giugale.
The study included women 18 years or older who were scheduled for a vaginal native tissue repair with apical support. Participants had to be able to tolerate general anesthesia with a standardized enhanced recovery after surgery (ERAS) protocol. The investigators excluded women undergoing mesh-augmented prolapse repairs or abdominal surgery and those with chronic pelvic pain or immunosuppression.
Each treatment arm had 25 patients. Patients had an average age of 69 years and an average body mass index of 27.5 kg/m2. Most patients were white, and demographic variables did not significantly differ among the groups.
“The distribution of prolapse procedures was similar among study groups, with colpocleisis being the most common, followed by uterosacral ligament suspension, levator myorrhaphy, and sacrospinous ligament fixation,” said Dr. Giugale. Rates of concomitant hysterectomy were similar for each group.
Before surgery, patients completed pain, nausea, and activities assessments. At 6 hours after surgery, they completed pain and nausea assessments. During postoperative days 1 through 3, patients documented pain scores and analgesic use. One week after surgery, patients completed pain and activities assessments. And at postoperative weeks 2, 6, and 12, they completed additional activities assessments. The assessments included validated handouts that patients completed at home, and no additional office visits were required.
The numeric rating scale pain score on the day after surgery was the primary outcome, and the median pain score did not significantly differ among the groups (3.75 in the placebo group, 4 in the bupivacaine group, and 3 in the bupivacaine plus dexamethasone group). Between-group differences in pain scores at other time points also were not significant.
Activities assessments, nausea and vomiting scores, the percentage of patients with same-day discharge, urinary retention, postoperative narcotic use as measured by oral morphine equivalents, and adverse events also did not significantly differ among the groups.
“One week after surgery, 52% of women reported that they were at or better than their baseline preoperative activity level, which increased to 70% at 2 weeks, 84% at 6 weeks, and 94% at 12 weeks,” Dr. Giugale said.
In all, 57% of patients used narcotic medicine the day after surgery, which decreased to 44% on day 3. The dosage was low, with a median oral morphine equivalent of 5 mg of oxycodone or less per day, she said.
Early postoperative pain may be influenced by procedure type, according to an exploratory analysis. Through the first postoperative day, “there was a trend toward more pain with uterosacral ligament suspension,” Dr. Giugale said. By day 3, sacrospinous ligament fixation was associated with significantly more postoperative pain.
The role of ERAS protocols
The heterogeneity of surgical procedures among the treatment groups and the use of a predefined ERAS protocol may have confounded the results. In addition, the researchers did not measure patient satisfaction, and the findings may not apply to different patient populations, Dr. Giugale noted.
“As more and more gynecologic surgery patients have surgery under these enhanced recovery protocols, maybe additional preemptive local analgesia for vaginal reconstructive surgery is not all that beneficial,” she said. “Maybe we are getting enough benefit from the enhanced [recovery] protocols themselves.”
The investigators studied a novel idea – dual local therapy for pain in patients undergoing pelvic floor surgery – and described a novel transobturator technique for levator injection, commented Sunil Balgobin, MD, associate director of the female pelvic medicine and reconstructive surgery fellowship at University of Texas Southwestern Medical Center, Dallas.
“For the current opioid problem, development of alternative pain control strategies is extremely important to reduce narcotic use and improve patient outcomes,” Dr. Balgobin said. The study “addresses an important gap in the literature, is relevant to surgeons performing vaginal apical procedures, and aims to advance research in this area for the potential benefit of ... patients.”
Interpretation of the results for individual procedure types may be limited by the smaller sample sizes, he added.
The researchers and Dr. Balgobin had no relevant financial disclosures.
SOURCE: Giugale L et al. SGS 2020, Abstract 10.
FROM SGS 2020
Are laser treatments better than steroids for lichen sclerosus?
Laser treatment for lichen sclerosus was noninferior to steroid therapy after 6 months and may lead to better outcomes on various patient- and physician-reported measures, according to trial results presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
Patients with lichen sclerosus often present with itching, burning, and dysuria. Untreated, the vulvar dystrophy can cause architectural changes and is associated with an increased risk of vulvar malignancies.
Topical steroids are the standard treatment. To assess whether fractional CO2 laser treatment is noninferior to clobetasol propionate at 6 months, Linda Burkett, MD, and colleagues conducted a randomized controlled trial. Dr. Burkett is affiliated with MedStar Washington Hospital Center and Georgetown University in Washington and UPMC Magee-Womens Hospital in Pittsburgh.
The researchers enrolled 52 postmenopausal women with biopsy-proven lichen sclerosus. Patients had to have significant symptoms reflected by a score of at least 21 on the Skindex-29.
Twenty-seven women were assigned to receive laser therapy, and 25 were assigned to receive steroids. One patient in the steroid arm was lost to follow-up. About half of the patients in each group had prior clobetasol propionate exposure.
Patients in the steroid arm were started on 0.05% clobetasol propionate used nightly for 4 weeks, then three times per week for 8 weeks, and then as needed. They had a phone call follow-up at 2 weeks to confirm compliance and an optional in-person appointment at 3 months.
Patients in the laser arm received three laser treatments 4-6 weeks apart.
At 6 months, all patients returned for repeat assessments. The primary outcome was the Skindex-29, a dermatologic questionnaire. Secondary outcomes included a patient visual analog scale of bothersome vulvar symptoms, a provider visual assessment score, the Vaginal Health Index, the Vulvovaginal Symptom Questionnaire, the Patient Global Impression of Improvement, and the Patient Global Impression of Satisfaction.
Average Skindex-29 scores from baseline to 6 months improved more in the laser treatment group, compared with the steroid group, for all health-related quality of life categories: overall, emotional, functional, and symptoms. “At 6 months across all scores, patients reported very little bother,” Dr. Burkett said.
Differences between the groups were statistically significant for all but the functional subscore.
Average scores on subjective secondary outcomes improved more in the laser treatment group, compared with the steroid treatment group. The between-group differences were statistically significant for irritation and the Vulvovaginal Symptom Questionnaire.
For provider-based scores, patients in the laser group had greater improvement on all measures except perianal involvement, relative to patients in the steroid group. In addition, fusion of the labia minora and phimosis worsened in the steroid group.
Differences between the groups were statistically significant for phimosis, erosion, and the Vaginal Health Index.
Significantly more patients in the laser group than in the steroid group were satisfied or very satisfied with the results at 6 months (81% vs. 41%). Patients in the laser group were more likely to report that they were better or much better (89% vs. 62%), though the difference was not statistically significant.
There were no major adverse events.
The trial – the first randomized controlled study of energy-based treatment for lichen sclerosus – was conducted at a single center, and treatment was not blinded, Dr. Burkett noted.
“The treatment effect was pretty significant in favor of laser therapy,” said Cecile A. Ferrando, MD, MPH, of the Center for Urogynecology and Pelvic Reconstructive Surgery at Cleveland Clinic, commenting on the research.
“Compliance issues with clobetasol aside,” the findings raise the question of whether laser therapy should be offered as first-line treatment, Dr. Ferrando said.
The study might have been more robust had it excluded patients with previous clobetasol propionate exposure, Dr. Ferrando added.
Dr. Burkett noted that future studies may incorporate multiple centers, histology measures, and sham laser treatments and include only women who have not previously received clobetasol propionate.
The researchers had no relevant financial disclosures. Dr. Ferrando disclosed authorship royalties from UpToDate.
SOURCE: Burkett L et al. SGS 2020, Abstract 09.
Laser treatment for lichen sclerosus was noninferior to steroid therapy after 6 months and may lead to better outcomes on various patient- and physician-reported measures, according to trial results presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
Patients with lichen sclerosus often present with itching, burning, and dysuria. Untreated, the vulvar dystrophy can cause architectural changes and is associated with an increased risk of vulvar malignancies.
Topical steroids are the standard treatment. To assess whether fractional CO2 laser treatment is noninferior to clobetasol propionate at 6 months, Linda Burkett, MD, and colleagues conducted a randomized controlled trial. Dr. Burkett is affiliated with MedStar Washington Hospital Center and Georgetown University in Washington and UPMC Magee-Womens Hospital in Pittsburgh.
The researchers enrolled 52 postmenopausal women with biopsy-proven lichen sclerosus. Patients had to have significant symptoms reflected by a score of at least 21 on the Skindex-29.
Twenty-seven women were assigned to receive laser therapy, and 25 were assigned to receive steroids. One patient in the steroid arm was lost to follow-up. About half of the patients in each group had prior clobetasol propionate exposure.
Patients in the steroid arm were started on 0.05% clobetasol propionate used nightly for 4 weeks, then three times per week for 8 weeks, and then as needed. They had a phone call follow-up at 2 weeks to confirm compliance and an optional in-person appointment at 3 months.
Patients in the laser arm received three laser treatments 4-6 weeks apart.
At 6 months, all patients returned for repeat assessments. The primary outcome was the Skindex-29, a dermatologic questionnaire. Secondary outcomes included a patient visual analog scale of bothersome vulvar symptoms, a provider visual assessment score, the Vaginal Health Index, the Vulvovaginal Symptom Questionnaire, the Patient Global Impression of Improvement, and the Patient Global Impression of Satisfaction.
Average Skindex-29 scores from baseline to 6 months improved more in the laser treatment group, compared with the steroid group, for all health-related quality of life categories: overall, emotional, functional, and symptoms. “At 6 months across all scores, patients reported very little bother,” Dr. Burkett said.
Differences between the groups were statistically significant for all but the functional subscore.
Average scores on subjective secondary outcomes improved more in the laser treatment group, compared with the steroid treatment group. The between-group differences were statistically significant for irritation and the Vulvovaginal Symptom Questionnaire.
For provider-based scores, patients in the laser group had greater improvement on all measures except perianal involvement, relative to patients in the steroid group. In addition, fusion of the labia minora and phimosis worsened in the steroid group.
Differences between the groups were statistically significant for phimosis, erosion, and the Vaginal Health Index.
Significantly more patients in the laser group than in the steroid group were satisfied or very satisfied with the results at 6 months (81% vs. 41%). Patients in the laser group were more likely to report that they were better or much better (89% vs. 62%), though the difference was not statistically significant.
There were no major adverse events.
The trial – the first randomized controlled study of energy-based treatment for lichen sclerosus – was conducted at a single center, and treatment was not blinded, Dr. Burkett noted.
“The treatment effect was pretty significant in favor of laser therapy,” said Cecile A. Ferrando, MD, MPH, of the Center for Urogynecology and Pelvic Reconstructive Surgery at Cleveland Clinic, commenting on the research.
“Compliance issues with clobetasol aside,” the findings raise the question of whether laser therapy should be offered as first-line treatment, Dr. Ferrando said.
The study might have been more robust had it excluded patients with previous clobetasol propionate exposure, Dr. Ferrando added.
Dr. Burkett noted that future studies may incorporate multiple centers, histology measures, and sham laser treatments and include only women who have not previously received clobetasol propionate.
The researchers had no relevant financial disclosures. Dr. Ferrando disclosed authorship royalties from UpToDate.
SOURCE: Burkett L et al. SGS 2020, Abstract 09.
Laser treatment for lichen sclerosus was noninferior to steroid therapy after 6 months and may lead to better outcomes on various patient- and physician-reported measures, according to trial results presented at the virtual annual scientific meeting of the Society of Gynecologic Surgeons.
Patients with lichen sclerosus often present with itching, burning, and dysuria. Untreated, the vulvar dystrophy can cause architectural changes and is associated with an increased risk of vulvar malignancies.
Topical steroids are the standard treatment. To assess whether fractional CO2 laser treatment is noninferior to clobetasol propionate at 6 months, Linda Burkett, MD, and colleagues conducted a randomized controlled trial. Dr. Burkett is affiliated with MedStar Washington Hospital Center and Georgetown University in Washington and UPMC Magee-Womens Hospital in Pittsburgh.
The researchers enrolled 52 postmenopausal women with biopsy-proven lichen sclerosus. Patients had to have significant symptoms reflected by a score of at least 21 on the Skindex-29.
Twenty-seven women were assigned to receive laser therapy, and 25 were assigned to receive steroids. One patient in the steroid arm was lost to follow-up. About half of the patients in each group had prior clobetasol propionate exposure.
Patients in the steroid arm were started on 0.05% clobetasol propionate used nightly for 4 weeks, then three times per week for 8 weeks, and then as needed. They had a phone call follow-up at 2 weeks to confirm compliance and an optional in-person appointment at 3 months.
Patients in the laser arm received three laser treatments 4-6 weeks apart.
At 6 months, all patients returned for repeat assessments. The primary outcome was the Skindex-29, a dermatologic questionnaire. Secondary outcomes included a patient visual analog scale of bothersome vulvar symptoms, a provider visual assessment score, the Vaginal Health Index, the Vulvovaginal Symptom Questionnaire, the Patient Global Impression of Improvement, and the Patient Global Impression of Satisfaction.
Average Skindex-29 scores from baseline to 6 months improved more in the laser treatment group, compared with the steroid group, for all health-related quality of life categories: overall, emotional, functional, and symptoms. “At 6 months across all scores, patients reported very little bother,” Dr. Burkett said.
Differences between the groups were statistically significant for all but the functional subscore.
Average scores on subjective secondary outcomes improved more in the laser treatment group, compared with the steroid treatment group. The between-group differences were statistically significant for irritation and the Vulvovaginal Symptom Questionnaire.
For provider-based scores, patients in the laser group had greater improvement on all measures except perianal involvement, relative to patients in the steroid group. In addition, fusion of the labia minora and phimosis worsened in the steroid group.
Differences between the groups were statistically significant for phimosis, erosion, and the Vaginal Health Index.
Significantly more patients in the laser group than in the steroid group were satisfied or very satisfied with the results at 6 months (81% vs. 41%). Patients in the laser group were more likely to report that they were better or much better (89% vs. 62%), though the difference was not statistically significant.
There were no major adverse events.
The trial – the first randomized controlled study of energy-based treatment for lichen sclerosus – was conducted at a single center, and treatment was not blinded, Dr. Burkett noted.
“The treatment effect was pretty significant in favor of laser therapy,” said Cecile A. Ferrando, MD, MPH, of the Center for Urogynecology and Pelvic Reconstructive Surgery at Cleveland Clinic, commenting on the research.
“Compliance issues with clobetasol aside,” the findings raise the question of whether laser therapy should be offered as first-line treatment, Dr. Ferrando said.
The study might have been more robust had it excluded patients with previous clobetasol propionate exposure, Dr. Ferrando added.
Dr. Burkett noted that future studies may incorporate multiple centers, histology measures, and sham laser treatments and include only women who have not previously received clobetasol propionate.
The researchers had no relevant financial disclosures. Dr. Ferrando disclosed authorship royalties from UpToDate.
SOURCE: Burkett L et al. SGS 2020, Abstract 09.
FROM SGS 2020
CMS to broaden transcatheter mitral valve repair coverage, and change its name
The first order of business in the long-awaited, recently released Centers for Medicare & Medicaid Services (CMS) proposed national coverage decision (NCD) for transcatheter mitral valve repair (TMVR) was to get rid of its familiar moniker.
The document tosses the term TMVR in favor of transcatheter edge-to-edge repair (TEER) “to more precisely define the treatment addressed in this NCD” and differentiate it from other therapies that repair or replace the mitral valve.
(In an off-the-cuff Twitter poll launched right after the CMS document’s release, 80.3% of respondents answered that they “hate” the new acronym and the remainder said they “love” it; those two were the poll’s only choices.)
The NCD proposal goes on to say that CMS coverage of TEER would expand to include treatment of symptomatic moderate-to-severe or severe functional mitral regurgitation (MR) when used with maximally tolerated guideline-directed medical therapy.
The proposed NCD has been expected since March 2019 when the US Food and Drug Administration (FDA) approved the MitraClip (Abbott Vascular) for secondary functional MR. Medicare has covered MitraClip for primary degenerative MR since 2014.
Abbott announced in October 2019 that it would ramp up production of the MitraClip, which is currently the only FDA-approved TEER device.
Further specifications
Even as the new proposed NCD would add CMS coverage for functional MR, it would also decline a coverage statement for degenerative MR. Instead, it proposes to leave such coverage decisions to local Medical Administrative Contractors (MACs), given a relatively low incidence of clip intervention for degenerative MR. Less than 1% of the Medicare population undergo TEER of the mitral valve for that indication, the document says.
“The MACs are structured to be able to take into account local patient, physician, and institutional factors, which are especially important when overall prevalence is very low.”
The proposal also emphasizes that patients undergoing such covered TEER procedures be “under the care of a heart failure physician specialist experienced in the care and treatment of mitral valve disease,» with additional care provided by a heart team that includes a cardiac surgeon, interventional cardiologist, interventional echocardiographer.
The new document is generally consistent with a Consensus Statement from the American Association for Thoracic Surgery, the American College of Cardiology (ACC), the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons published in December 2019 and covered then by theheart.org / Medscape Cardiology.
In anticipation the CMS coverage proposal, the ACC earlier this year published a Focused Update of the 2017 Expert Consensus Decision Pathway on the Management of Mitral Regurgitation to reflect new evidence in the field, mainly the recent clinical trial data on functional MR from the MITRA-FR and COAPT trials.
“The proposed criteria are nicely guided by the multisociety consensus document, which sought to foster optimal patient outcomes while also maintaining access to TEER,” Sammy Elmariah, MD, MPH, from Massachusetts General Hospital in Boston, commented by email.
“These criteria, in conjunction with results of the COAPT trial, establish TEER as the standard of care for patients with symptomatic functional MR despite guideline-directed medical therapy who do not possess an alternative indication for cardiac surgery,” said Elmariah, a coauthor on both the Consensus Statement and the Focused Update.
The proposed NCD seems “reasonable,” cardiothoracic surgeon Michael J. Reardon, MD, Houston Methodist Hospital, said by email. But he thought there might be some objections to the requirement for TEER centers to have a surgery program with a minimum annual volume for mitral-valve surgeries.
The proposed NCD says a hospital must have “a surgical program that performs ≥25 total mitral valve surgical procedures for severe MR per year, of which at least 10 must be mitral valve repairs.”
“There is a very definite relationship between mitral valve surgery volume and surgical outcomes and between TEER volume and TEER outcomes, but no real relationship between mitral valve surgery volumes and TEER outcomes,” Reardon said. “A mitral valve surgery program is important, but how many cases do you need to be able to start and run a TEER program?”
Edwards Lifesciences is currently testing its own device for TEER: the PASCAL transcatheter mitral valve repair system. Early findings from the company’s ongoing CLASP IID trial, a head-to-head comparison of Pascal and MitraClip, are expected in December 2023.
CMS is seeking comments on the proposed national coverage determination, and will render a final decision within 60 days of the end of the 30-day public comment period.
Elmariah discloses receiving research grants from the American Heart Association, the National Institutes of Health, Edwards Lifesciences, Svelte Medical, and Medtronic, and consulting fees from AstraZeneca. Reardon recently reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
The first order of business in the long-awaited, recently released Centers for Medicare & Medicaid Services (CMS) proposed national coverage decision (NCD) for transcatheter mitral valve repair (TMVR) was to get rid of its familiar moniker.
The document tosses the term TMVR in favor of transcatheter edge-to-edge repair (TEER) “to more precisely define the treatment addressed in this NCD” and differentiate it from other therapies that repair or replace the mitral valve.
(In an off-the-cuff Twitter poll launched right after the CMS document’s release, 80.3% of respondents answered that they “hate” the new acronym and the remainder said they “love” it; those two were the poll’s only choices.)
The NCD proposal goes on to say that CMS coverage of TEER would expand to include treatment of symptomatic moderate-to-severe or severe functional mitral regurgitation (MR) when used with maximally tolerated guideline-directed medical therapy.
The proposed NCD has been expected since March 2019 when the US Food and Drug Administration (FDA) approved the MitraClip (Abbott Vascular) for secondary functional MR. Medicare has covered MitraClip for primary degenerative MR since 2014.
Abbott announced in October 2019 that it would ramp up production of the MitraClip, which is currently the only FDA-approved TEER device.
Further specifications
Even as the new proposed NCD would add CMS coverage for functional MR, it would also decline a coverage statement for degenerative MR. Instead, it proposes to leave such coverage decisions to local Medical Administrative Contractors (MACs), given a relatively low incidence of clip intervention for degenerative MR. Less than 1% of the Medicare population undergo TEER of the mitral valve for that indication, the document says.
“The MACs are structured to be able to take into account local patient, physician, and institutional factors, which are especially important when overall prevalence is very low.”
The proposal also emphasizes that patients undergoing such covered TEER procedures be “under the care of a heart failure physician specialist experienced in the care and treatment of mitral valve disease,» with additional care provided by a heart team that includes a cardiac surgeon, interventional cardiologist, interventional echocardiographer.
The new document is generally consistent with a Consensus Statement from the American Association for Thoracic Surgery, the American College of Cardiology (ACC), the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons published in December 2019 and covered then by theheart.org / Medscape Cardiology.
In anticipation the CMS coverage proposal, the ACC earlier this year published a Focused Update of the 2017 Expert Consensus Decision Pathway on the Management of Mitral Regurgitation to reflect new evidence in the field, mainly the recent clinical trial data on functional MR from the MITRA-FR and COAPT trials.
“The proposed criteria are nicely guided by the multisociety consensus document, which sought to foster optimal patient outcomes while also maintaining access to TEER,” Sammy Elmariah, MD, MPH, from Massachusetts General Hospital in Boston, commented by email.
“These criteria, in conjunction with results of the COAPT trial, establish TEER as the standard of care for patients with symptomatic functional MR despite guideline-directed medical therapy who do not possess an alternative indication for cardiac surgery,” said Elmariah, a coauthor on both the Consensus Statement and the Focused Update.
The proposed NCD seems “reasonable,” cardiothoracic surgeon Michael J. Reardon, MD, Houston Methodist Hospital, said by email. But he thought there might be some objections to the requirement for TEER centers to have a surgery program with a minimum annual volume for mitral-valve surgeries.
The proposed NCD says a hospital must have “a surgical program that performs ≥25 total mitral valve surgical procedures for severe MR per year, of which at least 10 must be mitral valve repairs.”
“There is a very definite relationship between mitral valve surgery volume and surgical outcomes and between TEER volume and TEER outcomes, but no real relationship between mitral valve surgery volumes and TEER outcomes,” Reardon said. “A mitral valve surgery program is important, but how many cases do you need to be able to start and run a TEER program?”
Edwards Lifesciences is currently testing its own device for TEER: the PASCAL transcatheter mitral valve repair system. Early findings from the company’s ongoing CLASP IID trial, a head-to-head comparison of Pascal and MitraClip, are expected in December 2023.
CMS is seeking comments on the proposed national coverage determination, and will render a final decision within 60 days of the end of the 30-day public comment period.
Elmariah discloses receiving research grants from the American Heart Association, the National Institutes of Health, Edwards Lifesciences, Svelte Medical, and Medtronic, and consulting fees from AstraZeneca. Reardon recently reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
The first order of business in the long-awaited, recently released Centers for Medicare & Medicaid Services (CMS) proposed national coverage decision (NCD) for transcatheter mitral valve repair (TMVR) was to get rid of its familiar moniker.
The document tosses the term TMVR in favor of transcatheter edge-to-edge repair (TEER) “to more precisely define the treatment addressed in this NCD” and differentiate it from other therapies that repair or replace the mitral valve.
(In an off-the-cuff Twitter poll launched right after the CMS document’s release, 80.3% of respondents answered that they “hate” the new acronym and the remainder said they “love” it; those two were the poll’s only choices.)
The NCD proposal goes on to say that CMS coverage of TEER would expand to include treatment of symptomatic moderate-to-severe or severe functional mitral regurgitation (MR) when used with maximally tolerated guideline-directed medical therapy.
The proposed NCD has been expected since March 2019 when the US Food and Drug Administration (FDA) approved the MitraClip (Abbott Vascular) for secondary functional MR. Medicare has covered MitraClip for primary degenerative MR since 2014.
Abbott announced in October 2019 that it would ramp up production of the MitraClip, which is currently the only FDA-approved TEER device.
Further specifications
Even as the new proposed NCD would add CMS coverage for functional MR, it would also decline a coverage statement for degenerative MR. Instead, it proposes to leave such coverage decisions to local Medical Administrative Contractors (MACs), given a relatively low incidence of clip intervention for degenerative MR. Less than 1% of the Medicare population undergo TEER of the mitral valve for that indication, the document says.
“The MACs are structured to be able to take into account local patient, physician, and institutional factors, which are especially important when overall prevalence is very low.”
The proposal also emphasizes that patients undergoing such covered TEER procedures be “under the care of a heart failure physician specialist experienced in the care and treatment of mitral valve disease,» with additional care provided by a heart team that includes a cardiac surgeon, interventional cardiologist, interventional echocardiographer.
The new document is generally consistent with a Consensus Statement from the American Association for Thoracic Surgery, the American College of Cardiology (ACC), the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons published in December 2019 and covered then by theheart.org / Medscape Cardiology.
In anticipation the CMS coverage proposal, the ACC earlier this year published a Focused Update of the 2017 Expert Consensus Decision Pathway on the Management of Mitral Regurgitation to reflect new evidence in the field, mainly the recent clinical trial data on functional MR from the MITRA-FR and COAPT trials.
“The proposed criteria are nicely guided by the multisociety consensus document, which sought to foster optimal patient outcomes while also maintaining access to TEER,” Sammy Elmariah, MD, MPH, from Massachusetts General Hospital in Boston, commented by email.
“These criteria, in conjunction with results of the COAPT trial, establish TEER as the standard of care for patients with symptomatic functional MR despite guideline-directed medical therapy who do not possess an alternative indication for cardiac surgery,” said Elmariah, a coauthor on both the Consensus Statement and the Focused Update.
The proposed NCD seems “reasonable,” cardiothoracic surgeon Michael J. Reardon, MD, Houston Methodist Hospital, said by email. But he thought there might be some objections to the requirement for TEER centers to have a surgery program with a minimum annual volume for mitral-valve surgeries.
The proposed NCD says a hospital must have “a surgical program that performs ≥25 total mitral valve surgical procedures for severe MR per year, of which at least 10 must be mitral valve repairs.”
“There is a very definite relationship between mitral valve surgery volume and surgical outcomes and between TEER volume and TEER outcomes, but no real relationship between mitral valve surgery volumes and TEER outcomes,” Reardon said. “A mitral valve surgery program is important, but how many cases do you need to be able to start and run a TEER program?”
Edwards Lifesciences is currently testing its own device for TEER: the PASCAL transcatheter mitral valve repair system. Early findings from the company’s ongoing CLASP IID trial, a head-to-head comparison of Pascal and MitraClip, are expected in December 2023.
CMS is seeking comments on the proposed national coverage determination, and will render a final decision within 60 days of the end of the 30-day public comment period.
Elmariah discloses receiving research grants from the American Heart Association, the National Institutes of Health, Edwards Lifesciences, Svelte Medical, and Medtronic, and consulting fees from AstraZeneca. Reardon recently reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
Oxford coronavirus vaccine ‘triggers immune response’
The early stage results, published in The Lancet, found that the candidate vaccine, known as ChAdOx1 nCoV-19, provoked a T-cell response peaking 14 days after vaccination, and an antibody response within 28 days.
Andrew Pollard, chief investigator on the study, and professor of pediatric infection and immunity at Oxford University, described the results as “encouraging”. He told a briefing convened by the Science Media Centre on Monday that it was “a really important milestone on the path to the development of the vaccine”.
In the Commons, the Health Secretary, Matt Hancock, hailed the results for taking us “one step closer to finding a vaccine that can potentially save lives, all around the world”.
The trial, which has so far involved 1,077 healthy adults, caused minor side effects when compared with a control group given a meningitis vaccine. Fatigue and headache were the most commonly reported reactions.
However, there were no serious adverse events from the vaccine, the researchers said.
‘Still a long way to go’
Sarah Gilbert, lead researcher of the vaccine development program, and professor of vaccinology at Oxford, cautioned that there was still a long way to go before the team could confirm that the vaccine could protect against developing COVID-19.
“The difficulty that we have, and that all vaccine developers have in trying to make a vaccine against this particular virus, is that we don’t know how strong that immune response needs to be,” she said.
“So, we can’t say just by looking at immune responses whether this is going to protect people or not. And the only way we’re going to find out is by doing the large phase 3 trials and wait for people to be infected as part of that trial before we know if the vaccine can work.”
The authors noted some limitations to their findings. They said more research was needed to confirm their results in different groups of people – including older age groups, those with other health conditions, and in ethnically and geographically diverse populations.
A notable result of the trial was that participants given a second dose of the vaccine appeared to display a stronger immune response, a finding that had influenced plans to “look at two dose regimes as well as one dose regimes in the phase 3 trial”, Prof Adrian Hill, director of Oxford’s Jenner Institute, confirmed.
ChAdOx1 nCoV-19 is made from a weakened version of an adenovirus that causes infections in chimpanzees. The virus has been genetically modified so that it cannot grow in humans.
On Monday, the government announced that it had struck a deal with AstraZeneca for access to 100 million doses of the Oxford vaccine, in addition to millions of doses of other promising candidate vaccines.
Expert reaction to the findings
The Medical Research Council helped to fund the trial. Executive Chair Professor Fiona Watt commented: “It is truly remarkable how fast this vaccine has progressed, with our support, through early clinical trials, and it is very encouraging that it shows no safety concerns and evokes strong immune responses.
“There is a lot that we don’t yet know about immunity to the virus that causes COVID-19. However, it seems that both antibody and T cell immunity are important, and this vaccine triggers both responses. The much anticipated next milestone will be the results of the larger trials that are happening now to find out if the vaccine will protect people from the virus.”
Jonathan Ball, professor of molecular virology at the University of Nottingham, told the SMC: “The results of the Oxford chimp adenovirus vaccine candidate show that the vaccine is able to generate antibodies and T cells in humans and these persisted for several weeks. Whilst encouraging there is still a long way to go before we can herald the arrival of a successful coronavirus vaccine.
“It is unclear whether the levels of immunity can protect against infection – that’s what the larger ongoing phase III trials are designed to test. Nor do we know if this vaccine can protect those most vulnerable to severe COVID-19 disease.”
Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene and Tropical Medicine, commented: “For the vaccine to be really useful, we not only need the larger studies conducted where COVID-19 is still occurring at a high rate, but we need to be reasonably sure that the protection lasts for a considerable time.”
He said it was also vital that people older than 55 were included in later trials.
Richard Torbett, chief executive of the Association of the British Pharmaceutical Industry, said: “Developing a vaccine is an incredibly difficult challenge; the fact that there are multiple candidates in development is hopefully a sign that the hard work will ultimately pay off.
“But we must be patient. Proving that a vaccine is safe and effective is a long process and we could still be many months away.”
This article first appeared on Medscape.com.
The early stage results, published in The Lancet, found that the candidate vaccine, known as ChAdOx1 nCoV-19, provoked a T-cell response peaking 14 days after vaccination, and an antibody response within 28 days.
Andrew Pollard, chief investigator on the study, and professor of pediatric infection and immunity at Oxford University, described the results as “encouraging”. He told a briefing convened by the Science Media Centre on Monday that it was “a really important milestone on the path to the development of the vaccine”.
In the Commons, the Health Secretary, Matt Hancock, hailed the results for taking us “one step closer to finding a vaccine that can potentially save lives, all around the world”.
The trial, which has so far involved 1,077 healthy adults, caused minor side effects when compared with a control group given a meningitis vaccine. Fatigue and headache were the most commonly reported reactions.
However, there were no serious adverse events from the vaccine, the researchers said.
‘Still a long way to go’
Sarah Gilbert, lead researcher of the vaccine development program, and professor of vaccinology at Oxford, cautioned that there was still a long way to go before the team could confirm that the vaccine could protect against developing COVID-19.
“The difficulty that we have, and that all vaccine developers have in trying to make a vaccine against this particular virus, is that we don’t know how strong that immune response needs to be,” she said.
“So, we can’t say just by looking at immune responses whether this is going to protect people or not. And the only way we’re going to find out is by doing the large phase 3 trials and wait for people to be infected as part of that trial before we know if the vaccine can work.”
The authors noted some limitations to their findings. They said more research was needed to confirm their results in different groups of people – including older age groups, those with other health conditions, and in ethnically and geographically diverse populations.
A notable result of the trial was that participants given a second dose of the vaccine appeared to display a stronger immune response, a finding that had influenced plans to “look at two dose regimes as well as one dose regimes in the phase 3 trial”, Prof Adrian Hill, director of Oxford’s Jenner Institute, confirmed.
ChAdOx1 nCoV-19 is made from a weakened version of an adenovirus that causes infections in chimpanzees. The virus has been genetically modified so that it cannot grow in humans.
On Monday, the government announced that it had struck a deal with AstraZeneca for access to 100 million doses of the Oxford vaccine, in addition to millions of doses of other promising candidate vaccines.
Expert reaction to the findings
The Medical Research Council helped to fund the trial. Executive Chair Professor Fiona Watt commented: “It is truly remarkable how fast this vaccine has progressed, with our support, through early clinical trials, and it is very encouraging that it shows no safety concerns and evokes strong immune responses.
“There is a lot that we don’t yet know about immunity to the virus that causes COVID-19. However, it seems that both antibody and T cell immunity are important, and this vaccine triggers both responses. The much anticipated next milestone will be the results of the larger trials that are happening now to find out if the vaccine will protect people from the virus.”
Jonathan Ball, professor of molecular virology at the University of Nottingham, told the SMC: “The results of the Oxford chimp adenovirus vaccine candidate show that the vaccine is able to generate antibodies and T cells in humans and these persisted for several weeks. Whilst encouraging there is still a long way to go before we can herald the arrival of a successful coronavirus vaccine.
“It is unclear whether the levels of immunity can protect against infection – that’s what the larger ongoing phase III trials are designed to test. Nor do we know if this vaccine can protect those most vulnerable to severe COVID-19 disease.”
Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene and Tropical Medicine, commented: “For the vaccine to be really useful, we not only need the larger studies conducted where COVID-19 is still occurring at a high rate, but we need to be reasonably sure that the protection lasts for a considerable time.”
He said it was also vital that people older than 55 were included in later trials.
Richard Torbett, chief executive of the Association of the British Pharmaceutical Industry, said: “Developing a vaccine is an incredibly difficult challenge; the fact that there are multiple candidates in development is hopefully a sign that the hard work will ultimately pay off.
“But we must be patient. Proving that a vaccine is safe and effective is a long process and we could still be many months away.”
This article first appeared on Medscape.com.
The early stage results, published in The Lancet, found that the candidate vaccine, known as ChAdOx1 nCoV-19, provoked a T-cell response peaking 14 days after vaccination, and an antibody response within 28 days.
Andrew Pollard, chief investigator on the study, and professor of pediatric infection and immunity at Oxford University, described the results as “encouraging”. He told a briefing convened by the Science Media Centre on Monday that it was “a really important milestone on the path to the development of the vaccine”.
In the Commons, the Health Secretary, Matt Hancock, hailed the results for taking us “one step closer to finding a vaccine that can potentially save lives, all around the world”.
The trial, which has so far involved 1,077 healthy adults, caused minor side effects when compared with a control group given a meningitis vaccine. Fatigue and headache were the most commonly reported reactions.
However, there were no serious adverse events from the vaccine, the researchers said.
‘Still a long way to go’
Sarah Gilbert, lead researcher of the vaccine development program, and professor of vaccinology at Oxford, cautioned that there was still a long way to go before the team could confirm that the vaccine could protect against developing COVID-19.
“The difficulty that we have, and that all vaccine developers have in trying to make a vaccine against this particular virus, is that we don’t know how strong that immune response needs to be,” she said.
“So, we can’t say just by looking at immune responses whether this is going to protect people or not. And the only way we’re going to find out is by doing the large phase 3 trials and wait for people to be infected as part of that trial before we know if the vaccine can work.”
The authors noted some limitations to their findings. They said more research was needed to confirm their results in different groups of people – including older age groups, those with other health conditions, and in ethnically and geographically diverse populations.
A notable result of the trial was that participants given a second dose of the vaccine appeared to display a stronger immune response, a finding that had influenced plans to “look at two dose regimes as well as one dose regimes in the phase 3 trial”, Prof Adrian Hill, director of Oxford’s Jenner Institute, confirmed.
ChAdOx1 nCoV-19 is made from a weakened version of an adenovirus that causes infections in chimpanzees. The virus has been genetically modified so that it cannot grow in humans.
On Monday, the government announced that it had struck a deal with AstraZeneca for access to 100 million doses of the Oxford vaccine, in addition to millions of doses of other promising candidate vaccines.
Expert reaction to the findings
The Medical Research Council helped to fund the trial. Executive Chair Professor Fiona Watt commented: “It is truly remarkable how fast this vaccine has progressed, with our support, through early clinical trials, and it is very encouraging that it shows no safety concerns and evokes strong immune responses.
“There is a lot that we don’t yet know about immunity to the virus that causes COVID-19. However, it seems that both antibody and T cell immunity are important, and this vaccine triggers both responses. The much anticipated next milestone will be the results of the larger trials that are happening now to find out if the vaccine will protect people from the virus.”
Jonathan Ball, professor of molecular virology at the University of Nottingham, told the SMC: “The results of the Oxford chimp adenovirus vaccine candidate show that the vaccine is able to generate antibodies and T cells in humans and these persisted for several weeks. Whilst encouraging there is still a long way to go before we can herald the arrival of a successful coronavirus vaccine.
“It is unclear whether the levels of immunity can protect against infection – that’s what the larger ongoing phase III trials are designed to test. Nor do we know if this vaccine can protect those most vulnerable to severe COVID-19 disease.”
Stephen Evans, professor of pharmacoepidemiology at the London School of Hygiene and Tropical Medicine, commented: “For the vaccine to be really useful, we not only need the larger studies conducted where COVID-19 is still occurring at a high rate, but we need to be reasonably sure that the protection lasts for a considerable time.”
He said it was also vital that people older than 55 were included in later trials.
Richard Torbett, chief executive of the Association of the British Pharmaceutical Industry, said: “Developing a vaccine is an incredibly difficult challenge; the fact that there are multiple candidates in development is hopefully a sign that the hard work will ultimately pay off.
“But we must be patient. Proving that a vaccine is safe and effective is a long process and we could still be many months away.”
This article first appeared on Medscape.com.