User login
Expert clarifies guidance on adolescent polycystic ovary syndrome
A trio of international expert recommendations mainly agree on essentials for the diagnosis and treatment of polycystic ovary syndrome in adolescents, but some confusion persists, according to Robert L. Rosenfield, MD, of the University of California, San Francisco.
In a commentary published in the Journal of Pediatric & Adolescent Gynecology, Dr. Rosenfield, who convened one of the three conferences at which guidance was developed, noted that the three recommendations – published by the Pediatric Endocrine Society, the International Consortium of Paediatric Endocrinology, and the International PCOS Network in 2015, 2017, and 2018, respectively – “are fairly dense” and reviews have suggested a lack of agreement. His comments offer perspective and practice suggestions that follow the consensus of the recommendations.
“All the documents agree on the core diagnostic criteria for adolescent PCOS: otherwise unexplained evidence of ovulatory dysfunction, as indicated by menstrual abnormalities based on stage-appropriate standards, and evidence of an androgen excess disorder,” Dr. Rosenfield said.
The main differences among the recommendations from the three groups reflect tension between the value of an early diagnosis and the liabilities of a mistaken diagnosis in the context of attitudes about adolescent contraception. “These are issues not likely to be resolved easily, yet they are matters for every physician to consider in management of each case,” he said.
Dr. Rosenfield emphasized that clinicians must consider PCOS “in the general context of all causes of adolescent menstrual disturbances,” when evaluating a girl within 1-2 years of menarche who presents with a menstrual abnormality, hirsutism, and/or acne that has been resistant to topical treatment.
A key point on which the recommendations differ is whether further assessment is needed if the menstrual abnormality has persisted for 1 year (the 2018 recommendations) or 2 years (the 2015 and 2017 recommendations), Dr. Rosenfield explained. “What the conferees struggled with is differentiating how long after menarche a menstrual abnormality should persist to avoid confusing PCOS with normal immaturity of the menstrual cycle,” known as physiologic adolescent anovulation (PAA). “The degree of certainty is improved only modestly by waiting 2 years rather than 1 year to make a diagnosis.”
However, the three documents agree that girls suspected of having PCOS within the first 1-2 years after menarche should be evaluated at that time, and followed with a diagnosis of “at risk for PCOS” if the early test results are consistent with a PCOS diagnosis, he said.
Another point of difference among the groups is the extent to which hirsutism and acne represent clinical evidence of hyperandrogenism that justifies testing for biochemical hyperandrogenism, Dr. Rosenfield said.
“All three sets of adolescent PCOS recommendations agree that investigation for biochemical hyperandrogenism be initiated by measuring serum total and/or free testosterone by specialty assays with well-defined reference ranges,” he said.
However, “documentation of biochemical hyperandrogenism has been problematic because standard platform assays of testosterone give grossly inaccurate results.”
As said Dr. Rosenfield. Guidelines in the United States favor estrogen-progestin combined oral contraceptives as first-line therapy, while the international guidelines support contraceptives if contraception also is desired; otherwise the 2017 guidelines recommend metformin as a first-line treatment.
“Agreement is uniform that healthy lifestyle management is first-line therapy for management of the associated obesity and metabolic disturbances, i.e., prior to and/or in conjunction with metformin therapy,” he noted.
In general, Dr. Rosenfield acknowledged that front-line clinicians cannot easily evaluate all early postmenarcheal girls for abnormal menstrual cycles. Instead, he advocated a “middle ground” approach between early diagnosis and potentially labeling a girl with a false positive diagnosis.
Postmenarcheal girls who are amenorrheic for 2 months could be assessed for signs of PCOS or pregnancy, and whether she is generally in good health, he said. “However, for example, if she remains amenorrheic for more than 90 days or if two successive periods are more than 2 months apart, laboratory screening would be reasonable.”
PCOS is “a diagnosis of exclusion for which referral to a specialist is advisable” to rule out other conditions such as non-classic congenital adrenal hyperplasia, hyperprolactinemia, endogenous Cushing syndrome, thyroid dysfunction, and virilizing tumors, said Dr. Rosenfield.
However, PCOS accounts for most cases of adolescent hyperandrogenism. The symptomatic treatment of early postmenarcheal girls at risk of PCOS is recommended to manage menstrual abnormality, hirsutism, acne, or obesity, and these girls should be reassessed by the time they finish high school after a 3-month treatment withdrawal period, he emphasized.
Dr. Rosenfield had no relevant financial conflicts to disclose.
SOURCE: Rosenfield RL. J Pediatr Adolesc Gynecol. 2020 June 29. doi: 10.1016/j.jpag.2020.06.017.
A trio of international expert recommendations mainly agree on essentials for the diagnosis and treatment of polycystic ovary syndrome in adolescents, but some confusion persists, according to Robert L. Rosenfield, MD, of the University of California, San Francisco.
In a commentary published in the Journal of Pediatric & Adolescent Gynecology, Dr. Rosenfield, who convened one of the three conferences at which guidance was developed, noted that the three recommendations – published by the Pediatric Endocrine Society, the International Consortium of Paediatric Endocrinology, and the International PCOS Network in 2015, 2017, and 2018, respectively – “are fairly dense” and reviews have suggested a lack of agreement. His comments offer perspective and practice suggestions that follow the consensus of the recommendations.
“All the documents agree on the core diagnostic criteria for adolescent PCOS: otherwise unexplained evidence of ovulatory dysfunction, as indicated by menstrual abnormalities based on stage-appropriate standards, and evidence of an androgen excess disorder,” Dr. Rosenfield said.
The main differences among the recommendations from the three groups reflect tension between the value of an early diagnosis and the liabilities of a mistaken diagnosis in the context of attitudes about adolescent contraception. “These are issues not likely to be resolved easily, yet they are matters for every physician to consider in management of each case,” he said.
Dr. Rosenfield emphasized that clinicians must consider PCOS “in the general context of all causes of adolescent menstrual disturbances,” when evaluating a girl within 1-2 years of menarche who presents with a menstrual abnormality, hirsutism, and/or acne that has been resistant to topical treatment.
A key point on which the recommendations differ is whether further assessment is needed if the menstrual abnormality has persisted for 1 year (the 2018 recommendations) or 2 years (the 2015 and 2017 recommendations), Dr. Rosenfield explained. “What the conferees struggled with is differentiating how long after menarche a menstrual abnormality should persist to avoid confusing PCOS with normal immaturity of the menstrual cycle,” known as physiologic adolescent anovulation (PAA). “The degree of certainty is improved only modestly by waiting 2 years rather than 1 year to make a diagnosis.”
However, the three documents agree that girls suspected of having PCOS within the first 1-2 years after menarche should be evaluated at that time, and followed with a diagnosis of “at risk for PCOS” if the early test results are consistent with a PCOS diagnosis, he said.
Another point of difference among the groups is the extent to which hirsutism and acne represent clinical evidence of hyperandrogenism that justifies testing for biochemical hyperandrogenism, Dr. Rosenfield said.
“All three sets of adolescent PCOS recommendations agree that investigation for biochemical hyperandrogenism be initiated by measuring serum total and/or free testosterone by specialty assays with well-defined reference ranges,” he said.
However, “documentation of biochemical hyperandrogenism has been problematic because standard platform assays of testosterone give grossly inaccurate results.”
As said Dr. Rosenfield. Guidelines in the United States favor estrogen-progestin combined oral contraceptives as first-line therapy, while the international guidelines support contraceptives if contraception also is desired; otherwise the 2017 guidelines recommend metformin as a first-line treatment.
“Agreement is uniform that healthy lifestyle management is first-line therapy for management of the associated obesity and metabolic disturbances, i.e., prior to and/or in conjunction with metformin therapy,” he noted.
In general, Dr. Rosenfield acknowledged that front-line clinicians cannot easily evaluate all early postmenarcheal girls for abnormal menstrual cycles. Instead, he advocated a “middle ground” approach between early diagnosis and potentially labeling a girl with a false positive diagnosis.
Postmenarcheal girls who are amenorrheic for 2 months could be assessed for signs of PCOS or pregnancy, and whether she is generally in good health, he said. “However, for example, if she remains amenorrheic for more than 90 days or if two successive periods are more than 2 months apart, laboratory screening would be reasonable.”
PCOS is “a diagnosis of exclusion for which referral to a specialist is advisable” to rule out other conditions such as non-classic congenital adrenal hyperplasia, hyperprolactinemia, endogenous Cushing syndrome, thyroid dysfunction, and virilizing tumors, said Dr. Rosenfield.
However, PCOS accounts for most cases of adolescent hyperandrogenism. The symptomatic treatment of early postmenarcheal girls at risk of PCOS is recommended to manage menstrual abnormality, hirsutism, acne, or obesity, and these girls should be reassessed by the time they finish high school after a 3-month treatment withdrawal period, he emphasized.
Dr. Rosenfield had no relevant financial conflicts to disclose.
SOURCE: Rosenfield RL. J Pediatr Adolesc Gynecol. 2020 June 29. doi: 10.1016/j.jpag.2020.06.017.
A trio of international expert recommendations mainly agree on essentials for the diagnosis and treatment of polycystic ovary syndrome in adolescents, but some confusion persists, according to Robert L. Rosenfield, MD, of the University of California, San Francisco.
In a commentary published in the Journal of Pediatric & Adolescent Gynecology, Dr. Rosenfield, who convened one of the three conferences at which guidance was developed, noted that the three recommendations – published by the Pediatric Endocrine Society, the International Consortium of Paediatric Endocrinology, and the International PCOS Network in 2015, 2017, and 2018, respectively – “are fairly dense” and reviews have suggested a lack of agreement. His comments offer perspective and practice suggestions that follow the consensus of the recommendations.
“All the documents agree on the core diagnostic criteria for adolescent PCOS: otherwise unexplained evidence of ovulatory dysfunction, as indicated by menstrual abnormalities based on stage-appropriate standards, and evidence of an androgen excess disorder,” Dr. Rosenfield said.
The main differences among the recommendations from the three groups reflect tension between the value of an early diagnosis and the liabilities of a mistaken diagnosis in the context of attitudes about adolescent contraception. “These are issues not likely to be resolved easily, yet they are matters for every physician to consider in management of each case,” he said.
Dr. Rosenfield emphasized that clinicians must consider PCOS “in the general context of all causes of adolescent menstrual disturbances,” when evaluating a girl within 1-2 years of menarche who presents with a menstrual abnormality, hirsutism, and/or acne that has been resistant to topical treatment.
A key point on which the recommendations differ is whether further assessment is needed if the menstrual abnormality has persisted for 1 year (the 2018 recommendations) or 2 years (the 2015 and 2017 recommendations), Dr. Rosenfield explained. “What the conferees struggled with is differentiating how long after menarche a menstrual abnormality should persist to avoid confusing PCOS with normal immaturity of the menstrual cycle,” known as physiologic adolescent anovulation (PAA). “The degree of certainty is improved only modestly by waiting 2 years rather than 1 year to make a diagnosis.”
However, the three documents agree that girls suspected of having PCOS within the first 1-2 years after menarche should be evaluated at that time, and followed with a diagnosis of “at risk for PCOS” if the early test results are consistent with a PCOS diagnosis, he said.
Another point of difference among the groups is the extent to which hirsutism and acne represent clinical evidence of hyperandrogenism that justifies testing for biochemical hyperandrogenism, Dr. Rosenfield said.
“All three sets of adolescent PCOS recommendations agree that investigation for biochemical hyperandrogenism be initiated by measuring serum total and/or free testosterone by specialty assays with well-defined reference ranges,” he said.
However, “documentation of biochemical hyperandrogenism has been problematic because standard platform assays of testosterone give grossly inaccurate results.”
As said Dr. Rosenfield. Guidelines in the United States favor estrogen-progestin combined oral contraceptives as first-line therapy, while the international guidelines support contraceptives if contraception also is desired; otherwise the 2017 guidelines recommend metformin as a first-line treatment.
“Agreement is uniform that healthy lifestyle management is first-line therapy for management of the associated obesity and metabolic disturbances, i.e., prior to and/or in conjunction with metformin therapy,” he noted.
In general, Dr. Rosenfield acknowledged that front-line clinicians cannot easily evaluate all early postmenarcheal girls for abnormal menstrual cycles. Instead, he advocated a “middle ground” approach between early diagnosis and potentially labeling a girl with a false positive diagnosis.
Postmenarcheal girls who are amenorrheic for 2 months could be assessed for signs of PCOS or pregnancy, and whether she is generally in good health, he said. “However, for example, if she remains amenorrheic for more than 90 days or if two successive periods are more than 2 months apart, laboratory screening would be reasonable.”
PCOS is “a diagnosis of exclusion for which referral to a specialist is advisable” to rule out other conditions such as non-classic congenital adrenal hyperplasia, hyperprolactinemia, endogenous Cushing syndrome, thyroid dysfunction, and virilizing tumors, said Dr. Rosenfield.
However, PCOS accounts for most cases of adolescent hyperandrogenism. The symptomatic treatment of early postmenarcheal girls at risk of PCOS is recommended to manage menstrual abnormality, hirsutism, acne, or obesity, and these girls should be reassessed by the time they finish high school after a 3-month treatment withdrawal period, he emphasized.
Dr. Rosenfield had no relevant financial conflicts to disclose.
SOURCE: Rosenfield RL. J Pediatr Adolesc Gynecol. 2020 June 29. doi: 10.1016/j.jpag.2020.06.017.
FROM THE JOURNAL OF PEDIATRIC AND ADOLESCENT GYNECOLOGY
COVID-19 pandemic dictates reconsideration of pemphigus therapy
The Dedee F. Murrell, MD, said at the virtual annual meeting of the American Academy of Dermatology.
Together with physicians from the Mayo Clinic, Alexandria (Egypt) University, and Tehran (Iran) University, she recently published updated expert guidance for treatment of this severe, potentially fatal mucocutaneous autoimmune blistering disease, in a letter to the editor in the Journal of the American Academy of Dermatology. She presented some of the key recommendations at AAD 2020.
First off, rituximab (Rituxan), the only Food and Drug Administration–approved medication for moderate to severe pemphigus vulgaris and a biologic considered first-line therapy prepandemic, is ill-advised during the COVID-19 era. Its mechanism of benefit is through B-cell depletion. This is an irreversible effect, and reconstitution of B-cell immunity takes 6-12 months. The absence of this immunologic protection for such a long time poses potentially serious problems for pemphigus patients who become infected with SARS-CoV-2.
Also, the opportunity to administer intravenous infusions of the biologic becomes unpredictable during pandemic surges, when limitations on nonemergent medical care may be necessary, noted Dr. Murrell, professor of dermatology at the University of New South Wales and head of dermatology at St. George University Hospital, both in Sydney.
“We have taken the approach of postponing rituximab infusions temporarily, with the aim of delaying peak patient immunosuppression during peak COVID-19 incidence to reduce the risk of adverse outcomes,” Dr. Murrell and coauthors wrote in the letter (J Am Acad Dermatol. 2020 Jun;82[6]:e235-6).
The other traditional go-to therapy for pemphigus is corticosteroids. They’re effective, fast acting, and relatively inexpensive. But their nonselective immunosuppressive action boosts infection risk in general, and more specifically it increases the risk of developing severe forms of COVID-19 should a patient become infected with SARS-CoV-2.
“A basic therapeutic principle with particular importance during the pandemic is that glucocorticoids and steroid-sparing immunosuppressive agents, such as azathioprine and mycophenolate mofetil, should be tapered to the lowest effective dose. In active COVID-19 infection, immunosuppressive steroid-sparing medications should be discontinued when possible, although glucocorticoid cessation often cannot be considered due to risk for adrenal insufficiency,” the authors continued.
“Effective as adjuvant treatment in both pemphigus and COVID-19,intravenous immunoglobulin supports immunity and therefore may be useful in this setting,” they wrote. It’s not immunosuppressive, and, they noted, there’s good-quality evidence from a Japanese randomized, double-blind, controlled trial that a 5-day course of intravenous immunoglobulin is effective therapy for pemphigus (J Am Acad Dermatol. 2009 Apr;60[4]:595-603).
Moreover, intravenous immunoglobulin is also reportedly effective in severe COVID-19 (Open Forum Infect Dis. 2020 Mar 21. doi: 10.1093/ofid/ofaa102.).
Another option is to consider enrolling a patient with moderate or severe pemphigus vulgaris or foliaceus in the ongoing pivotal phase 3, international, double-blind, placebo-controlled PEGASUS trial of rilzabrutinib, a promising oral reversible Bruton tyrosine kinase inhibitor. The medication has a short half-life and a self-limited immunomodulatory effect. Moreover, the trial is set up for remote patient visits on an outpatient basis via teledermatology, so the 65-week study can continue despite the pandemic. Both newly diagnosed and relapsing patients are eligible for the trial, headed by Dr. Murrell. At AAD 2020 she reported encouraging results from a phase 2b trial of rilzabrutinib.
She is a consultant to Principia Biopharma, sponsor of the PEGASUS trial, and has received institutional research grants from numerous pharmaceutical companies.
The Dedee F. Murrell, MD, said at the virtual annual meeting of the American Academy of Dermatology.
Together with physicians from the Mayo Clinic, Alexandria (Egypt) University, and Tehran (Iran) University, she recently published updated expert guidance for treatment of this severe, potentially fatal mucocutaneous autoimmune blistering disease, in a letter to the editor in the Journal of the American Academy of Dermatology. She presented some of the key recommendations at AAD 2020.
First off, rituximab (Rituxan), the only Food and Drug Administration–approved medication for moderate to severe pemphigus vulgaris and a biologic considered first-line therapy prepandemic, is ill-advised during the COVID-19 era. Its mechanism of benefit is through B-cell depletion. This is an irreversible effect, and reconstitution of B-cell immunity takes 6-12 months. The absence of this immunologic protection for such a long time poses potentially serious problems for pemphigus patients who become infected with SARS-CoV-2.
Also, the opportunity to administer intravenous infusions of the biologic becomes unpredictable during pandemic surges, when limitations on nonemergent medical care may be necessary, noted Dr. Murrell, professor of dermatology at the University of New South Wales and head of dermatology at St. George University Hospital, both in Sydney.
“We have taken the approach of postponing rituximab infusions temporarily, with the aim of delaying peak patient immunosuppression during peak COVID-19 incidence to reduce the risk of adverse outcomes,” Dr. Murrell and coauthors wrote in the letter (J Am Acad Dermatol. 2020 Jun;82[6]:e235-6).
The other traditional go-to therapy for pemphigus is corticosteroids. They’re effective, fast acting, and relatively inexpensive. But their nonselective immunosuppressive action boosts infection risk in general, and more specifically it increases the risk of developing severe forms of COVID-19 should a patient become infected with SARS-CoV-2.
“A basic therapeutic principle with particular importance during the pandemic is that glucocorticoids and steroid-sparing immunosuppressive agents, such as azathioprine and mycophenolate mofetil, should be tapered to the lowest effective dose. In active COVID-19 infection, immunosuppressive steroid-sparing medications should be discontinued when possible, although glucocorticoid cessation often cannot be considered due to risk for adrenal insufficiency,” the authors continued.
“Effective as adjuvant treatment in both pemphigus and COVID-19,intravenous immunoglobulin supports immunity and therefore may be useful in this setting,” they wrote. It’s not immunosuppressive, and, they noted, there’s good-quality evidence from a Japanese randomized, double-blind, controlled trial that a 5-day course of intravenous immunoglobulin is effective therapy for pemphigus (J Am Acad Dermatol. 2009 Apr;60[4]:595-603).
Moreover, intravenous immunoglobulin is also reportedly effective in severe COVID-19 (Open Forum Infect Dis. 2020 Mar 21. doi: 10.1093/ofid/ofaa102.).
Another option is to consider enrolling a patient with moderate or severe pemphigus vulgaris or foliaceus in the ongoing pivotal phase 3, international, double-blind, placebo-controlled PEGASUS trial of rilzabrutinib, a promising oral reversible Bruton tyrosine kinase inhibitor. The medication has a short half-life and a self-limited immunomodulatory effect. Moreover, the trial is set up for remote patient visits on an outpatient basis via teledermatology, so the 65-week study can continue despite the pandemic. Both newly diagnosed and relapsing patients are eligible for the trial, headed by Dr. Murrell. At AAD 2020 she reported encouraging results from a phase 2b trial of rilzabrutinib.
She is a consultant to Principia Biopharma, sponsor of the PEGASUS trial, and has received institutional research grants from numerous pharmaceutical companies.
The Dedee F. Murrell, MD, said at the virtual annual meeting of the American Academy of Dermatology.
Together with physicians from the Mayo Clinic, Alexandria (Egypt) University, and Tehran (Iran) University, she recently published updated expert guidance for treatment of this severe, potentially fatal mucocutaneous autoimmune blistering disease, in a letter to the editor in the Journal of the American Academy of Dermatology. She presented some of the key recommendations at AAD 2020.
First off, rituximab (Rituxan), the only Food and Drug Administration–approved medication for moderate to severe pemphigus vulgaris and a biologic considered first-line therapy prepandemic, is ill-advised during the COVID-19 era. Its mechanism of benefit is through B-cell depletion. This is an irreversible effect, and reconstitution of B-cell immunity takes 6-12 months. The absence of this immunologic protection for such a long time poses potentially serious problems for pemphigus patients who become infected with SARS-CoV-2.
Also, the opportunity to administer intravenous infusions of the biologic becomes unpredictable during pandemic surges, when limitations on nonemergent medical care may be necessary, noted Dr. Murrell, professor of dermatology at the University of New South Wales and head of dermatology at St. George University Hospital, both in Sydney.
“We have taken the approach of postponing rituximab infusions temporarily, with the aim of delaying peak patient immunosuppression during peak COVID-19 incidence to reduce the risk of adverse outcomes,” Dr. Murrell and coauthors wrote in the letter (J Am Acad Dermatol. 2020 Jun;82[6]:e235-6).
The other traditional go-to therapy for pemphigus is corticosteroids. They’re effective, fast acting, and relatively inexpensive. But their nonselective immunosuppressive action boosts infection risk in general, and more specifically it increases the risk of developing severe forms of COVID-19 should a patient become infected with SARS-CoV-2.
“A basic therapeutic principle with particular importance during the pandemic is that glucocorticoids and steroid-sparing immunosuppressive agents, such as azathioprine and mycophenolate mofetil, should be tapered to the lowest effective dose. In active COVID-19 infection, immunosuppressive steroid-sparing medications should be discontinued when possible, although glucocorticoid cessation often cannot be considered due to risk for adrenal insufficiency,” the authors continued.
“Effective as adjuvant treatment in both pemphigus and COVID-19,intravenous immunoglobulin supports immunity and therefore may be useful in this setting,” they wrote. It’s not immunosuppressive, and, they noted, there’s good-quality evidence from a Japanese randomized, double-blind, controlled trial that a 5-day course of intravenous immunoglobulin is effective therapy for pemphigus (J Am Acad Dermatol. 2009 Apr;60[4]:595-603).
Moreover, intravenous immunoglobulin is also reportedly effective in severe COVID-19 (Open Forum Infect Dis. 2020 Mar 21. doi: 10.1093/ofid/ofaa102.).
Another option is to consider enrolling a patient with moderate or severe pemphigus vulgaris or foliaceus in the ongoing pivotal phase 3, international, double-blind, placebo-controlled PEGASUS trial of rilzabrutinib, a promising oral reversible Bruton tyrosine kinase inhibitor. The medication has a short half-life and a self-limited immunomodulatory effect. Moreover, the trial is set up for remote patient visits on an outpatient basis via teledermatology, so the 65-week study can continue despite the pandemic. Both newly diagnosed and relapsing patients are eligible for the trial, headed by Dr. Murrell. At AAD 2020 she reported encouraging results from a phase 2b trial of rilzabrutinib.
She is a consultant to Principia Biopharma, sponsor of the PEGASUS trial, and has received institutional research grants from numerous pharmaceutical companies.
FROM AAD 20
Hemospray shows high efficacy, but rebleeding concerns remain
Hemospray is highly effective for initial gastrointestinal hemostasis, but not long-term therapy, based on a recent meta-analysis.
Among 814 patients with GI bleeding who were treated with Hemospray, respective rates of clinical success and early rebleeding were 92% and 20%, reported lead author Andrew Ofosu, MD, of the Brooklyn Hospital Center, New York, and colleagues.
“Since its introduction, multiple studies have evaluated the efficacy of Hemospray for endoscopic hemostasis in a wide array of bleeding disorders in either the upper and/or lower GI tract,” the investigators wrote. Their report is in the Journal of Clinical Gastroenterology.
The present review and meta-analysis included 19 of those studies, including randomized controlled trials, case series, and case-control studies.
Of 814 adult patients, 212 were treated with Hemospray as monotherapy, while 602 were treated with Hemospray combined with conventional hemostatic techniques.
“Unlike conventional endoscopic methods currently in use to achieve immediate hemostasis in GI bleeding, Hemospray is noncontact, nonthermal, and nontraumatic,” the investigators noted.
Clinical success, defined by endoscopically observed initial hemostasis, was achieved in 91% of patients who were treated with Hemospray as monotherapy, a rate that did not significantly differ from the 93% success rate achieved by a combination approach.
Early rebleeding, defined by rebleeding within 7 days, was comparable between monotherapy (21%) and combination therapy (20%), a finding that was maintained in subgroup analysis. Similarly, no statistical difference was found between rates of rebleeding within 30 days, which were 22% and 24%, for monotherapy and combination therapy, respectively.
“Our study showed the rate of rebleeding increased with time after the application of Hemospray, likely due to the limited duration of action of the hemostatic powder at the site of bleeding,” wrote Dr. Ofosu and colleagues. “Second-look endoscopy performed in some studies has shown Hemospray is eliminated from the GI tract in as few as 24 hours after use, which potentially increases the risk of recurrent bleeding.”
The investigators suggested that Hemospray is best suited for short-term use because of the rebleeding risk.
“The use of Hemospray offers the potential to control bleeding initially and to optimize positioning or application of other modalities if needed in a more controlled setting,” concluded Dr. Ofosu and colleagues, who noted that this stance aligns with the views of other investigators.
Daljeet Chahal, MD and Fergal Donnellan, MD, of the University of British Columbia, Vancouver, are two such investigators, having just published a retrospective cohort study that involved 86 applications of Hemospray. Their study, which was not included in the present meta-analysis because of recency of publication, revealed that “Hemospray is effective in achieving immediate hemostasis but is plagued by high rates of rebleeding.”
According to Dr. Chahal and Dr. Donnellan, who provided a written comment, the findings of Dr. Ofosu and colleagues are comparable to their own, thereby supporting a similar conclusion.
“Hemospray appears more suited to emergent situations, where it should be used as a last resort; as a bridge therapy to more definitive measures such as embolization or surgery,” they wrote.
Dr. Chahal and Dr. Donnellan also suggested that more work is needed to develop a comprehensive picture of Hemospray outcomes, which could guide usage.
“The meta-analysis does not comment specifically on rates of embolization or surgery after Hemospray use, or whether these rates differ by type of lesion,” they wrote. “These would be interesting measures to explore in future studies to more concretely define appropriate indications for Hemospray use.”
Bilal Toka, MD, of Sakarya University in Serdivan, Turkey, who has previously published research comparing conventional hemostatic techniques, also provided a written comment, in which he advised clinicians to be ready for a combination approach, particularly among high-risk patients.
“This meta-analysis shows that Hemospray is very useful in providing initial hemostasis in patients with GI bleeding,” Dr. Toka wrote. “[However], due to its high early and delayed rebleeding rates, additional mechanical or thermal endoscopic treatment should be applied in high-risk lesions such as actively bleeding peptic ulcers.”
The investigators reported no conflicts of interest.
SOURCE: Ofosu A et al. J Clin Gastroenterol. 2020 Jul 3. doi: 10.1097/MCG.0000000000001379.
Hemospray is highly effective for initial gastrointestinal hemostasis, but not long-term therapy, based on a recent meta-analysis.
Among 814 patients with GI bleeding who were treated with Hemospray, respective rates of clinical success and early rebleeding were 92% and 20%, reported lead author Andrew Ofosu, MD, of the Brooklyn Hospital Center, New York, and colleagues.
“Since its introduction, multiple studies have evaluated the efficacy of Hemospray for endoscopic hemostasis in a wide array of bleeding disorders in either the upper and/or lower GI tract,” the investigators wrote. Their report is in the Journal of Clinical Gastroenterology.
The present review and meta-analysis included 19 of those studies, including randomized controlled trials, case series, and case-control studies.
Of 814 adult patients, 212 were treated with Hemospray as monotherapy, while 602 were treated with Hemospray combined with conventional hemostatic techniques.
“Unlike conventional endoscopic methods currently in use to achieve immediate hemostasis in GI bleeding, Hemospray is noncontact, nonthermal, and nontraumatic,” the investigators noted.
Clinical success, defined by endoscopically observed initial hemostasis, was achieved in 91% of patients who were treated with Hemospray as monotherapy, a rate that did not significantly differ from the 93% success rate achieved by a combination approach.
Early rebleeding, defined by rebleeding within 7 days, was comparable between monotherapy (21%) and combination therapy (20%), a finding that was maintained in subgroup analysis. Similarly, no statistical difference was found between rates of rebleeding within 30 days, which were 22% and 24%, for monotherapy and combination therapy, respectively.
“Our study showed the rate of rebleeding increased with time after the application of Hemospray, likely due to the limited duration of action of the hemostatic powder at the site of bleeding,” wrote Dr. Ofosu and colleagues. “Second-look endoscopy performed in some studies has shown Hemospray is eliminated from the GI tract in as few as 24 hours after use, which potentially increases the risk of recurrent bleeding.”
The investigators suggested that Hemospray is best suited for short-term use because of the rebleeding risk.
“The use of Hemospray offers the potential to control bleeding initially and to optimize positioning or application of other modalities if needed in a more controlled setting,” concluded Dr. Ofosu and colleagues, who noted that this stance aligns with the views of other investigators.
Daljeet Chahal, MD and Fergal Donnellan, MD, of the University of British Columbia, Vancouver, are two such investigators, having just published a retrospective cohort study that involved 86 applications of Hemospray. Their study, which was not included in the present meta-analysis because of recency of publication, revealed that “Hemospray is effective in achieving immediate hemostasis but is plagued by high rates of rebleeding.”
According to Dr. Chahal and Dr. Donnellan, who provided a written comment, the findings of Dr. Ofosu and colleagues are comparable to their own, thereby supporting a similar conclusion.
“Hemospray appears more suited to emergent situations, where it should be used as a last resort; as a bridge therapy to more definitive measures such as embolization or surgery,” they wrote.
Dr. Chahal and Dr. Donnellan also suggested that more work is needed to develop a comprehensive picture of Hemospray outcomes, which could guide usage.
“The meta-analysis does not comment specifically on rates of embolization or surgery after Hemospray use, or whether these rates differ by type of lesion,” they wrote. “These would be interesting measures to explore in future studies to more concretely define appropriate indications for Hemospray use.”
Bilal Toka, MD, of Sakarya University in Serdivan, Turkey, who has previously published research comparing conventional hemostatic techniques, also provided a written comment, in which he advised clinicians to be ready for a combination approach, particularly among high-risk patients.
“This meta-analysis shows that Hemospray is very useful in providing initial hemostasis in patients with GI bleeding,” Dr. Toka wrote. “[However], due to its high early and delayed rebleeding rates, additional mechanical or thermal endoscopic treatment should be applied in high-risk lesions such as actively bleeding peptic ulcers.”
The investigators reported no conflicts of interest.
SOURCE: Ofosu A et al. J Clin Gastroenterol. 2020 Jul 3. doi: 10.1097/MCG.0000000000001379.
Hemospray is highly effective for initial gastrointestinal hemostasis, but not long-term therapy, based on a recent meta-analysis.
Among 814 patients with GI bleeding who were treated with Hemospray, respective rates of clinical success and early rebleeding were 92% and 20%, reported lead author Andrew Ofosu, MD, of the Brooklyn Hospital Center, New York, and colleagues.
“Since its introduction, multiple studies have evaluated the efficacy of Hemospray for endoscopic hemostasis in a wide array of bleeding disorders in either the upper and/or lower GI tract,” the investigators wrote. Their report is in the Journal of Clinical Gastroenterology.
The present review and meta-analysis included 19 of those studies, including randomized controlled trials, case series, and case-control studies.
Of 814 adult patients, 212 were treated with Hemospray as monotherapy, while 602 were treated with Hemospray combined with conventional hemostatic techniques.
“Unlike conventional endoscopic methods currently in use to achieve immediate hemostasis in GI bleeding, Hemospray is noncontact, nonthermal, and nontraumatic,” the investigators noted.
Clinical success, defined by endoscopically observed initial hemostasis, was achieved in 91% of patients who were treated with Hemospray as monotherapy, a rate that did not significantly differ from the 93% success rate achieved by a combination approach.
Early rebleeding, defined by rebleeding within 7 days, was comparable between monotherapy (21%) and combination therapy (20%), a finding that was maintained in subgroup analysis. Similarly, no statistical difference was found between rates of rebleeding within 30 days, which were 22% and 24%, for monotherapy and combination therapy, respectively.
“Our study showed the rate of rebleeding increased with time after the application of Hemospray, likely due to the limited duration of action of the hemostatic powder at the site of bleeding,” wrote Dr. Ofosu and colleagues. “Second-look endoscopy performed in some studies has shown Hemospray is eliminated from the GI tract in as few as 24 hours after use, which potentially increases the risk of recurrent bleeding.”
The investigators suggested that Hemospray is best suited for short-term use because of the rebleeding risk.
“The use of Hemospray offers the potential to control bleeding initially and to optimize positioning or application of other modalities if needed in a more controlled setting,” concluded Dr. Ofosu and colleagues, who noted that this stance aligns with the views of other investigators.
Daljeet Chahal, MD and Fergal Donnellan, MD, of the University of British Columbia, Vancouver, are two such investigators, having just published a retrospective cohort study that involved 86 applications of Hemospray. Their study, which was not included in the present meta-analysis because of recency of publication, revealed that “Hemospray is effective in achieving immediate hemostasis but is plagued by high rates of rebleeding.”
According to Dr. Chahal and Dr. Donnellan, who provided a written comment, the findings of Dr. Ofosu and colleagues are comparable to their own, thereby supporting a similar conclusion.
“Hemospray appears more suited to emergent situations, where it should be used as a last resort; as a bridge therapy to more definitive measures such as embolization or surgery,” they wrote.
Dr. Chahal and Dr. Donnellan also suggested that more work is needed to develop a comprehensive picture of Hemospray outcomes, which could guide usage.
“The meta-analysis does not comment specifically on rates of embolization or surgery after Hemospray use, or whether these rates differ by type of lesion,” they wrote. “These would be interesting measures to explore in future studies to more concretely define appropriate indications for Hemospray use.”
Bilal Toka, MD, of Sakarya University in Serdivan, Turkey, who has previously published research comparing conventional hemostatic techniques, also provided a written comment, in which he advised clinicians to be ready for a combination approach, particularly among high-risk patients.
“This meta-analysis shows that Hemospray is very useful in providing initial hemostasis in patients with GI bleeding,” Dr. Toka wrote. “[However], due to its high early and delayed rebleeding rates, additional mechanical or thermal endoscopic treatment should be applied in high-risk lesions such as actively bleeding peptic ulcers.”
The investigators reported no conflicts of interest.
SOURCE: Ofosu A et al. J Clin Gastroenterol. 2020 Jul 3. doi: 10.1097/MCG.0000000000001379.
FROM THE JOURNAL OF CLINICAL GASTROENTEROLOGY
Prior beta-blockers predict extra burden of heart failure in women with ACS
In the analysis of more than 13,000 patients with ACS and no history of cardiovascular (CV) disease, the women who had taken beta-blockers for hypertension showed about a one-third increased risk for heart failure (HF) at the time of their ACS presentation.
The difference between women and men was especially pronounced among patients with ST-segment elevation MI, compared with those with non-STEMI.
No such relationship between sex and risk for HF with ACS was observed among the larger portion of the cohort that had not previously been treated with beta-blockers, according to a report published July 13 in Hypertension, with lead author Raffaele Bugiardini, MD, University of Bologna (Italy).
Mortality at 30 days was sharply higher for patients with than without HF at their ACS presentation, by more than 600% for women and more than 800% for men.
“Our study provides robust evidence of an interaction between sex and beta-blocker therapy and suggests an increased risk of HF among women presenting with incident myocardial infarction,” Dr. Bugiardini said in an interview.
Given their novelty, “our findings raise strong concern about the appropriate role of beta-blockers in the therapy of hypertension in women with no prior history of cardiovascular diseases. Beta-blocker use may be an acute precipitant of heart failure in women presenting with incident ACS as first manifestation of coronary heart disease.” Dr. Bugiardini and colleagues wrote.
“There is one main implication for clinical practice. Discontinuing a beta-blocker in an otherwise healthy woman with hypertension and no prior CV disease is not harmful and could be wise,” Dr. Bugiardini said. “Blood pressure in women may be regulated in a safer way, such as using other medications and, of course, through diet and exercise.”
Rationale for the study
Men and women “differ with respect to the risk, causes, and prognosis of HF,” Dr. Bugiardini and colleagues wrote, and current guidelines “do not differentiate between the use of beta-blockers in men and in women.”
However, they proposed, “because prior trials and meta-analyses enrolled nearly five men for every woman, any differences in the effect of beta-blockers among women would have been concealed by the effect of beta-blocker therapy among men.”
The current study looked at data from October 2010 to July 2018 in the ISACS ARCHIVES, ISACS-TC, and the EMMACE-3X registries, covering 13,764 patients from 12 European countries who had a history of hypertension and presented with confirmed ACS.
Of the combined cohort, 2,590 (19%) had been treated with beta-blockers prior to their ACS presentation. They were similar to those without a history of beta-blocker use with respect to baseline features and use of other medications in an adjusted analysis.
In the group with prior beta-blocker use, 21.3% of the women and 16.7% of the men had HF of Killip class 2 or higher, a 4.6% absolute difference that worked out to a relative risk of 1.35 (95% confidence interval, 1.10-1.65).
The corresponding rates for women and men without prior beta-blocker use were 17.2% and 16.1%, respectively, for an absolute difference of only 1.1% and an RR of1.09 (95% CI, 0.97-1.21).
The interaction between sex and beta-blocker therapy for the HF outcome was significant (P < .034). An analysis that excluded patients in cardiogenic shock at their ACS presentation produced similar results.
In an analysis only of patients with STEMI, the RR for HF in women versus men was 1.44 (95% CI, 1.12-1.84) among those with a history of beta-blocker use, and 1.11 (95% CI, 0.98-1.26) among those who hadn’t used the drugs. The interaction between sex and beta-blocker use was significant (P = .033).
No such significant interaction was seen for the subgroup with non-STEMI as their index ACS (P = .14).
Heart failure at ACS was the most powerful observed predictor of 30-day mortality in women and in men in multivariate analysis; the odds ratios were 7.54 (95% CI, 5.78-9.83) and 9.62 (95% CI, 7.67-12.07), respectively.
“Our study underscores the importance of sex analyses in clinical research studies, which may provide further actionable data,” Dr. Bugiardini stated. “Failure to include both sexes in therapeutic studies is a missed opportunity to uncover underlying sex-specific risks. The adverse effect of beta-blocker therapy in women with hypertension is a sex-specific risk.”
Not just a male disease
Part of the study’s conclusions are “really not that surprising, because we have known for a long time that women who have an MI are much more likely to develop HF than men, and we also know that HF raises mortality after MI,” Ileana L. Pina, MD, MPH, Wayne State University, Detroit, said in an interview.
But what surprised her was that women taking beta-blockers were at greater risk for HF. “This association needs to be proven in a prospective study and confirmed in another dataset,” said Dr. Pina, who was not involved with the current study. “The most important message is to remember that HF is not just a ‘male’ disease and to pay attention to the symptoms of women and not discount or relegate them to anxiety or gastric problems.”
The study was observational, Dr. Bugiardini noted, so “the results may have some variance and need confirmation. However, a sex-stratified, randomized, controlled trial of beta-blocker therapy in patients with hypertension but no prior history of coronary heart disease or HF may not be considered ethical, since it would be designed to confirm risk … and not benefit.”
“Further observational studies may give confirmation,” he added. “In the meantime, the Food and Drug Administration should alert health care professionals of the adverse events associated with beta-blocker use in women with hypertension and no prior history of CV disease, [because] prescribing beta-blockers to a woman with hypertension means exposing her to unnecessary risk.”
Dr. Bugiardini and the other authors had no disclosures. Dr. Pina reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In the analysis of more than 13,000 patients with ACS and no history of cardiovascular (CV) disease, the women who had taken beta-blockers for hypertension showed about a one-third increased risk for heart failure (HF) at the time of their ACS presentation.
The difference between women and men was especially pronounced among patients with ST-segment elevation MI, compared with those with non-STEMI.
No such relationship between sex and risk for HF with ACS was observed among the larger portion of the cohort that had not previously been treated with beta-blockers, according to a report published July 13 in Hypertension, with lead author Raffaele Bugiardini, MD, University of Bologna (Italy).
Mortality at 30 days was sharply higher for patients with than without HF at their ACS presentation, by more than 600% for women and more than 800% for men.
“Our study provides robust evidence of an interaction between sex and beta-blocker therapy and suggests an increased risk of HF among women presenting with incident myocardial infarction,” Dr. Bugiardini said in an interview.
Given their novelty, “our findings raise strong concern about the appropriate role of beta-blockers in the therapy of hypertension in women with no prior history of cardiovascular diseases. Beta-blocker use may be an acute precipitant of heart failure in women presenting with incident ACS as first manifestation of coronary heart disease.” Dr. Bugiardini and colleagues wrote.
“There is one main implication for clinical practice. Discontinuing a beta-blocker in an otherwise healthy woman with hypertension and no prior CV disease is not harmful and could be wise,” Dr. Bugiardini said. “Blood pressure in women may be regulated in a safer way, such as using other medications and, of course, through diet and exercise.”
Rationale for the study
Men and women “differ with respect to the risk, causes, and prognosis of HF,” Dr. Bugiardini and colleagues wrote, and current guidelines “do not differentiate between the use of beta-blockers in men and in women.”
However, they proposed, “because prior trials and meta-analyses enrolled nearly five men for every woman, any differences in the effect of beta-blockers among women would have been concealed by the effect of beta-blocker therapy among men.”
The current study looked at data from October 2010 to July 2018 in the ISACS ARCHIVES, ISACS-TC, and the EMMACE-3X registries, covering 13,764 patients from 12 European countries who had a history of hypertension and presented with confirmed ACS.
Of the combined cohort, 2,590 (19%) had been treated with beta-blockers prior to their ACS presentation. They were similar to those without a history of beta-blocker use with respect to baseline features and use of other medications in an adjusted analysis.
In the group with prior beta-blocker use, 21.3% of the women and 16.7% of the men had HF of Killip class 2 or higher, a 4.6% absolute difference that worked out to a relative risk of 1.35 (95% confidence interval, 1.10-1.65).
The corresponding rates for women and men without prior beta-blocker use were 17.2% and 16.1%, respectively, for an absolute difference of only 1.1% and an RR of1.09 (95% CI, 0.97-1.21).
The interaction between sex and beta-blocker therapy for the HF outcome was significant (P < .034). An analysis that excluded patients in cardiogenic shock at their ACS presentation produced similar results.
In an analysis only of patients with STEMI, the RR for HF in women versus men was 1.44 (95% CI, 1.12-1.84) among those with a history of beta-blocker use, and 1.11 (95% CI, 0.98-1.26) among those who hadn’t used the drugs. The interaction between sex and beta-blocker use was significant (P = .033).
No such significant interaction was seen for the subgroup with non-STEMI as their index ACS (P = .14).
Heart failure at ACS was the most powerful observed predictor of 30-day mortality in women and in men in multivariate analysis; the odds ratios were 7.54 (95% CI, 5.78-9.83) and 9.62 (95% CI, 7.67-12.07), respectively.
“Our study underscores the importance of sex analyses in clinical research studies, which may provide further actionable data,” Dr. Bugiardini stated. “Failure to include both sexes in therapeutic studies is a missed opportunity to uncover underlying sex-specific risks. The adverse effect of beta-blocker therapy in women with hypertension is a sex-specific risk.”
Not just a male disease
Part of the study’s conclusions are “really not that surprising, because we have known for a long time that women who have an MI are much more likely to develop HF than men, and we also know that HF raises mortality after MI,” Ileana L. Pina, MD, MPH, Wayne State University, Detroit, said in an interview.
But what surprised her was that women taking beta-blockers were at greater risk for HF. “This association needs to be proven in a prospective study and confirmed in another dataset,” said Dr. Pina, who was not involved with the current study. “The most important message is to remember that HF is not just a ‘male’ disease and to pay attention to the symptoms of women and not discount or relegate them to anxiety or gastric problems.”
The study was observational, Dr. Bugiardini noted, so “the results may have some variance and need confirmation. However, a sex-stratified, randomized, controlled trial of beta-blocker therapy in patients with hypertension but no prior history of coronary heart disease or HF may not be considered ethical, since it would be designed to confirm risk … and not benefit.”
“Further observational studies may give confirmation,” he added. “In the meantime, the Food and Drug Administration should alert health care professionals of the adverse events associated with beta-blocker use in women with hypertension and no prior history of CV disease, [because] prescribing beta-blockers to a woman with hypertension means exposing her to unnecessary risk.”
Dr. Bugiardini and the other authors had no disclosures. Dr. Pina reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In the analysis of more than 13,000 patients with ACS and no history of cardiovascular (CV) disease, the women who had taken beta-blockers for hypertension showed about a one-third increased risk for heart failure (HF) at the time of their ACS presentation.
The difference between women and men was especially pronounced among patients with ST-segment elevation MI, compared with those with non-STEMI.
No such relationship between sex and risk for HF with ACS was observed among the larger portion of the cohort that had not previously been treated with beta-blockers, according to a report published July 13 in Hypertension, with lead author Raffaele Bugiardini, MD, University of Bologna (Italy).
Mortality at 30 days was sharply higher for patients with than without HF at their ACS presentation, by more than 600% for women and more than 800% for men.
“Our study provides robust evidence of an interaction between sex and beta-blocker therapy and suggests an increased risk of HF among women presenting with incident myocardial infarction,” Dr. Bugiardini said in an interview.
Given their novelty, “our findings raise strong concern about the appropriate role of beta-blockers in the therapy of hypertension in women with no prior history of cardiovascular diseases. Beta-blocker use may be an acute precipitant of heart failure in women presenting with incident ACS as first manifestation of coronary heart disease.” Dr. Bugiardini and colleagues wrote.
“There is one main implication for clinical practice. Discontinuing a beta-blocker in an otherwise healthy woman with hypertension and no prior CV disease is not harmful and could be wise,” Dr. Bugiardini said. “Blood pressure in women may be regulated in a safer way, such as using other medications and, of course, through diet and exercise.”
Rationale for the study
Men and women “differ with respect to the risk, causes, and prognosis of HF,” Dr. Bugiardini and colleagues wrote, and current guidelines “do not differentiate between the use of beta-blockers in men and in women.”
However, they proposed, “because prior trials and meta-analyses enrolled nearly five men for every woman, any differences in the effect of beta-blockers among women would have been concealed by the effect of beta-blocker therapy among men.”
The current study looked at data from October 2010 to July 2018 in the ISACS ARCHIVES, ISACS-TC, and the EMMACE-3X registries, covering 13,764 patients from 12 European countries who had a history of hypertension and presented with confirmed ACS.
Of the combined cohort, 2,590 (19%) had been treated with beta-blockers prior to their ACS presentation. They were similar to those without a history of beta-blocker use with respect to baseline features and use of other medications in an adjusted analysis.
In the group with prior beta-blocker use, 21.3% of the women and 16.7% of the men had HF of Killip class 2 or higher, a 4.6% absolute difference that worked out to a relative risk of 1.35 (95% confidence interval, 1.10-1.65).
The corresponding rates for women and men without prior beta-blocker use were 17.2% and 16.1%, respectively, for an absolute difference of only 1.1% and an RR of1.09 (95% CI, 0.97-1.21).
The interaction between sex and beta-blocker therapy for the HF outcome was significant (P < .034). An analysis that excluded patients in cardiogenic shock at their ACS presentation produced similar results.
In an analysis only of patients with STEMI, the RR for HF in women versus men was 1.44 (95% CI, 1.12-1.84) among those with a history of beta-blocker use, and 1.11 (95% CI, 0.98-1.26) among those who hadn’t used the drugs. The interaction between sex and beta-blocker use was significant (P = .033).
No such significant interaction was seen for the subgroup with non-STEMI as their index ACS (P = .14).
Heart failure at ACS was the most powerful observed predictor of 30-day mortality in women and in men in multivariate analysis; the odds ratios were 7.54 (95% CI, 5.78-9.83) and 9.62 (95% CI, 7.67-12.07), respectively.
“Our study underscores the importance of sex analyses in clinical research studies, which may provide further actionable data,” Dr. Bugiardini stated. “Failure to include both sexes in therapeutic studies is a missed opportunity to uncover underlying sex-specific risks. The adverse effect of beta-blocker therapy in women with hypertension is a sex-specific risk.”
Not just a male disease
Part of the study’s conclusions are “really not that surprising, because we have known for a long time that women who have an MI are much more likely to develop HF than men, and we also know that HF raises mortality after MI,” Ileana L. Pina, MD, MPH, Wayne State University, Detroit, said in an interview.
But what surprised her was that women taking beta-blockers were at greater risk for HF. “This association needs to be proven in a prospective study and confirmed in another dataset,” said Dr. Pina, who was not involved with the current study. “The most important message is to remember that HF is not just a ‘male’ disease and to pay attention to the symptoms of women and not discount or relegate them to anxiety or gastric problems.”
The study was observational, Dr. Bugiardini noted, so “the results may have some variance and need confirmation. However, a sex-stratified, randomized, controlled trial of beta-blocker therapy in patients with hypertension but no prior history of coronary heart disease or HF may not be considered ethical, since it would be designed to confirm risk … and not benefit.”
“Further observational studies may give confirmation,” he added. “In the meantime, the Food and Drug Administration should alert health care professionals of the adverse events associated with beta-blocker use in women with hypertension and no prior history of CV disease, [because] prescribing beta-blockers to a woman with hypertension means exposing her to unnecessary risk.”
Dr. Bugiardini and the other authors had no disclosures. Dr. Pina reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
PCI or not, mortality climbs with post-ACS bleeding complications
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
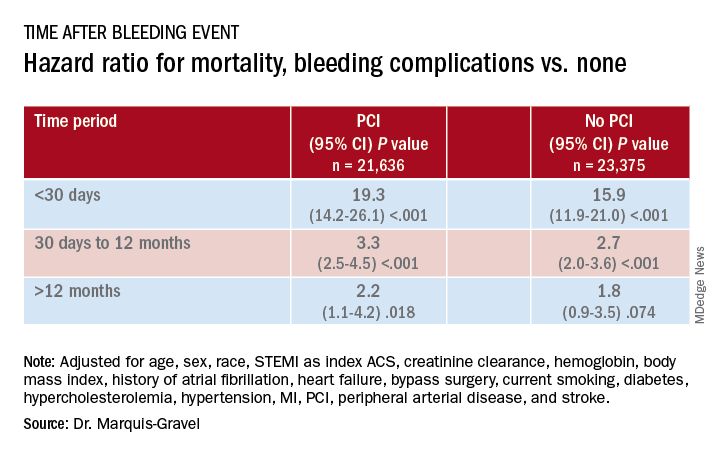
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
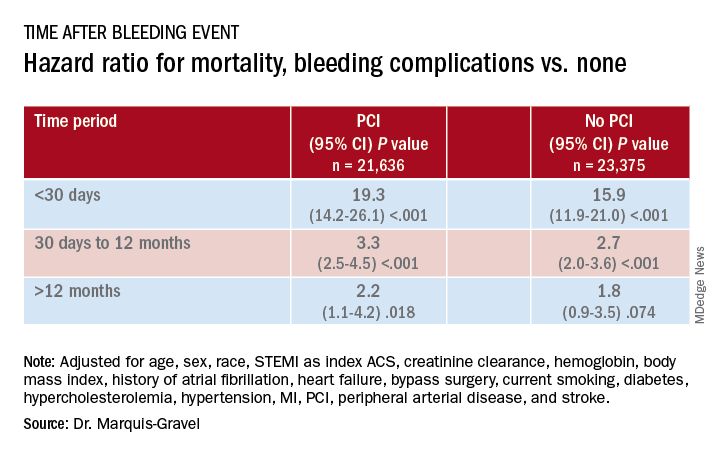
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
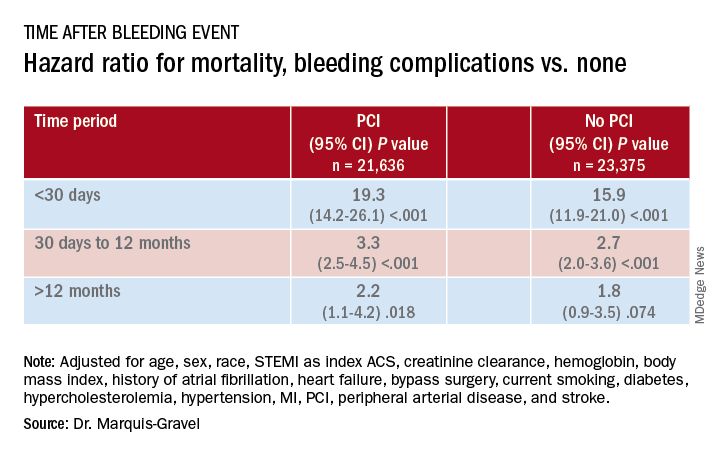
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Proton pump inhibitors tied to COVID-19 risk
In light of this finding, physicians should consider which patients truly need these powerful acid-lowering drugs, said Brennan Spiegel, MD, MSHS, AGAF, professor of medicine and public health at Cedars Sinai Medical Center in Los Angeles, Calif.
“All it means is that we’re going to have a conversation with our patients,” he said in an interview. “We don’t normally have that conversation because we don’t live in an environment with a high risk of enteric infection. But now we’re in a pandemic.”
The study by Dr. Spiegel and his colleagues was published online on July 7 in the American Journal of Gastroenterology.
Use of PPIs has skyrocketed over the past 2 decades. For ambulatory care visits, their use increased from 1.6% in 1998 to 7.6% in 2015. The increase raised questions about overprescription.
Although studies have not borne out many of the other concerns raised about adverse reactions, they have shown that the drugs increase the risk for enteric infections, including infections by SARS-CoV-1, a virus that is related to the COVID-19 virus, SARS-CoV-2, Dr. Spiegel said.
SARS-CoV-2 uses the angiotensin-converting enzyme–2 receptor to invade enterocytes. Dr. Spiegel theorized that an increase in stomach pH above 3 as a result of use of PPIs might allow the virus to enter the GI tract more easily, leading to enteritis, colitis, and systemic spread to other organs, including the lungs. “There is a reason we have acid in our stomachs,” Dr. Spiegel said.
To see how PPI use relates to COVID-19 infections, Dr. Spiegel and his colleagues surveyed online a nationally representative sample of Americans between May 3 and June 24, 2020, as part of a larger survey on gastroenterologic health.
Participants answered questions about gastrointestinal symptoms, current use of PPIs, and COVID-19 test results. They also answered questions about histamine-2 receptor agonists (H2RAs), also known as H2 blockers, which are used to treat some of the same conditions as PPIs but that do not reduce stomach acid as much.
The surveying firm, Cint, contacted 264,058 people. Of the 86,602 eligible participants who completed the survey, 53,130 said they had experienced abdominal discomfort, acid reflux, heartburn, or regurgitation. These survey participants were subsequently asked about PPI and H2RA use.
Of these, 6.4% reported testing positive for SARS-CoV-2. The researchers adjusted for age, sex, race/ethnicity, education, marital status, household income, body mass index, smoking, alcohol consumption, U.S. region, insurance status, and the presence of irritable bowel syndrome, celiac disease, gastroesophageal reflux disease, liver cirrhosis, Crohn’s disease, ulcerative colitis, diabetes, and HIV/AIDS.
After adjusting for these factors, the researchers found that those who took PPIs up to once a day were twice as likely to have had a positive COVID-19 test result than those who did not take the drugs (odds ratio, 2.15; 95% confidence interval, 1.90-2.44).
Those who took PPIs twice a day were almost four times as likely to have tested positive for the disease (OR, 3.67; 95% CI, 2.93-4.60).
By contrast, those taking H2RA drugs once daily were 15% less likely to report a positive COVID-19 test result (OR, 0.85; 95% CI, 0.74-0.99). Research is currently underway to determine whether H2RAs might protect against the disease for reasons unrelated to pH balance.
Dr. Spiegel cautioned that the current data show only an association between PPI use and COVID-19 positivity; it cannot prove cause and effect.
Nevertheless, Dr. Spiegel said the findings should encourage physicians to prescribe PPIs only when clearly indicated. “If somebody is not yet on a PPI and you’re considering whether to start them on a PPI, it’s a good idea to consider H2 blockers,” he said.
People who need a daily dose of a PPI to control a severe condition can safely continue doing so, but such patients should take care to follow standard public health recommendations for avoiding exposure to the virus. These recommendations include wearing a mask, maintaining social distance, and washing hands frequently.
“People who are older, comorbid, or smokers – if they get infected, it could be severe,” he said. “[For] someone like that, it’s reasonable to ask, do we really need to be on twice-daily PPIs? There is good evidence that they are no better off than if they are taking once-daily doses.”
Brian Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., agreed that the study should prompt physicians to take a second look at their patients’ PPI prescriptions. “My view is that PPIs are frequently overused, and maybe this is one more piece of data that, if someone is on PPIs, maybe they don’t need to be on this medication.”
On the other hand, the drugs are important for treating conditions such as erosive esophagitis and healing ulcers, he said. The overall risk of contracting COVID-19 is low, so even this finding of a 3.7-fold increased risk should not lead patients or providers to stop taking or prescribing PPIs.
The study also lends support to the idea that the gastrointestinal tract could be involved in SARS-CoV-2 transmission, and it supports warnings about aerosols emitted from flushing toilets and through exhalation, Dr. Spiegel said. There is less evidence of the virus being transmitted through food. “It may not be fecal-oral; it may be fecal-respiratory,” he said.
The study was part of a larger project funded by Ironwood Pharmaceuticals. Dr. Spiegel reported relationships with Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Shire Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. Dr. Lacy has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In light of this finding, physicians should consider which patients truly need these powerful acid-lowering drugs, said Brennan Spiegel, MD, MSHS, AGAF, professor of medicine and public health at Cedars Sinai Medical Center in Los Angeles, Calif.
“All it means is that we’re going to have a conversation with our patients,” he said in an interview. “We don’t normally have that conversation because we don’t live in an environment with a high risk of enteric infection. But now we’re in a pandemic.”
The study by Dr. Spiegel and his colleagues was published online on July 7 in the American Journal of Gastroenterology.
Use of PPIs has skyrocketed over the past 2 decades. For ambulatory care visits, their use increased from 1.6% in 1998 to 7.6% in 2015. The increase raised questions about overprescription.
Although studies have not borne out many of the other concerns raised about adverse reactions, they have shown that the drugs increase the risk for enteric infections, including infections by SARS-CoV-1, a virus that is related to the COVID-19 virus, SARS-CoV-2, Dr. Spiegel said.
SARS-CoV-2 uses the angiotensin-converting enzyme–2 receptor to invade enterocytes. Dr. Spiegel theorized that an increase in stomach pH above 3 as a result of use of PPIs might allow the virus to enter the GI tract more easily, leading to enteritis, colitis, and systemic spread to other organs, including the lungs. “There is a reason we have acid in our stomachs,” Dr. Spiegel said.
To see how PPI use relates to COVID-19 infections, Dr. Spiegel and his colleagues surveyed online a nationally representative sample of Americans between May 3 and June 24, 2020, as part of a larger survey on gastroenterologic health.
Participants answered questions about gastrointestinal symptoms, current use of PPIs, and COVID-19 test results. They also answered questions about histamine-2 receptor agonists (H2RAs), also known as H2 blockers, which are used to treat some of the same conditions as PPIs but that do not reduce stomach acid as much.
The surveying firm, Cint, contacted 264,058 people. Of the 86,602 eligible participants who completed the survey, 53,130 said they had experienced abdominal discomfort, acid reflux, heartburn, or regurgitation. These survey participants were subsequently asked about PPI and H2RA use.
Of these, 6.4% reported testing positive for SARS-CoV-2. The researchers adjusted for age, sex, race/ethnicity, education, marital status, household income, body mass index, smoking, alcohol consumption, U.S. region, insurance status, and the presence of irritable bowel syndrome, celiac disease, gastroesophageal reflux disease, liver cirrhosis, Crohn’s disease, ulcerative colitis, diabetes, and HIV/AIDS.
After adjusting for these factors, the researchers found that those who took PPIs up to once a day were twice as likely to have had a positive COVID-19 test result than those who did not take the drugs (odds ratio, 2.15; 95% confidence interval, 1.90-2.44).
Those who took PPIs twice a day were almost four times as likely to have tested positive for the disease (OR, 3.67; 95% CI, 2.93-4.60).
By contrast, those taking H2RA drugs once daily were 15% less likely to report a positive COVID-19 test result (OR, 0.85; 95% CI, 0.74-0.99). Research is currently underway to determine whether H2RAs might protect against the disease for reasons unrelated to pH balance.
Dr. Spiegel cautioned that the current data show only an association between PPI use and COVID-19 positivity; it cannot prove cause and effect.
Nevertheless, Dr. Spiegel said the findings should encourage physicians to prescribe PPIs only when clearly indicated. “If somebody is not yet on a PPI and you’re considering whether to start them on a PPI, it’s a good idea to consider H2 blockers,” he said.
People who need a daily dose of a PPI to control a severe condition can safely continue doing so, but such patients should take care to follow standard public health recommendations for avoiding exposure to the virus. These recommendations include wearing a mask, maintaining social distance, and washing hands frequently.
“People who are older, comorbid, or smokers – if they get infected, it could be severe,” he said. “[For] someone like that, it’s reasonable to ask, do we really need to be on twice-daily PPIs? There is good evidence that they are no better off than if they are taking once-daily doses.”
Brian Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., agreed that the study should prompt physicians to take a second look at their patients’ PPI prescriptions. “My view is that PPIs are frequently overused, and maybe this is one more piece of data that, if someone is on PPIs, maybe they don’t need to be on this medication.”
On the other hand, the drugs are important for treating conditions such as erosive esophagitis and healing ulcers, he said. The overall risk of contracting COVID-19 is low, so even this finding of a 3.7-fold increased risk should not lead patients or providers to stop taking or prescribing PPIs.
The study also lends support to the idea that the gastrointestinal tract could be involved in SARS-CoV-2 transmission, and it supports warnings about aerosols emitted from flushing toilets and through exhalation, Dr. Spiegel said. There is less evidence of the virus being transmitted through food. “It may not be fecal-oral; it may be fecal-respiratory,” he said.
The study was part of a larger project funded by Ironwood Pharmaceuticals. Dr. Spiegel reported relationships with Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Shire Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. Dr. Lacy has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
In light of this finding, physicians should consider which patients truly need these powerful acid-lowering drugs, said Brennan Spiegel, MD, MSHS, AGAF, professor of medicine and public health at Cedars Sinai Medical Center in Los Angeles, Calif.
“All it means is that we’re going to have a conversation with our patients,” he said in an interview. “We don’t normally have that conversation because we don’t live in an environment with a high risk of enteric infection. But now we’re in a pandemic.”
The study by Dr. Spiegel and his colleagues was published online on July 7 in the American Journal of Gastroenterology.
Use of PPIs has skyrocketed over the past 2 decades. For ambulatory care visits, their use increased from 1.6% in 1998 to 7.6% in 2015. The increase raised questions about overprescription.
Although studies have not borne out many of the other concerns raised about adverse reactions, they have shown that the drugs increase the risk for enteric infections, including infections by SARS-CoV-1, a virus that is related to the COVID-19 virus, SARS-CoV-2, Dr. Spiegel said.
SARS-CoV-2 uses the angiotensin-converting enzyme–2 receptor to invade enterocytes. Dr. Spiegel theorized that an increase in stomach pH above 3 as a result of use of PPIs might allow the virus to enter the GI tract more easily, leading to enteritis, colitis, and systemic spread to other organs, including the lungs. “There is a reason we have acid in our stomachs,” Dr. Spiegel said.
To see how PPI use relates to COVID-19 infections, Dr. Spiegel and his colleagues surveyed online a nationally representative sample of Americans between May 3 and June 24, 2020, as part of a larger survey on gastroenterologic health.
Participants answered questions about gastrointestinal symptoms, current use of PPIs, and COVID-19 test results. They also answered questions about histamine-2 receptor agonists (H2RAs), also known as H2 blockers, which are used to treat some of the same conditions as PPIs but that do not reduce stomach acid as much.
The surveying firm, Cint, contacted 264,058 people. Of the 86,602 eligible participants who completed the survey, 53,130 said they had experienced abdominal discomfort, acid reflux, heartburn, or regurgitation. These survey participants were subsequently asked about PPI and H2RA use.
Of these, 6.4% reported testing positive for SARS-CoV-2. The researchers adjusted for age, sex, race/ethnicity, education, marital status, household income, body mass index, smoking, alcohol consumption, U.S. region, insurance status, and the presence of irritable bowel syndrome, celiac disease, gastroesophageal reflux disease, liver cirrhosis, Crohn’s disease, ulcerative colitis, diabetes, and HIV/AIDS.
After adjusting for these factors, the researchers found that those who took PPIs up to once a day were twice as likely to have had a positive COVID-19 test result than those who did not take the drugs (odds ratio, 2.15; 95% confidence interval, 1.90-2.44).
Those who took PPIs twice a day were almost four times as likely to have tested positive for the disease (OR, 3.67; 95% CI, 2.93-4.60).
By contrast, those taking H2RA drugs once daily were 15% less likely to report a positive COVID-19 test result (OR, 0.85; 95% CI, 0.74-0.99). Research is currently underway to determine whether H2RAs might protect against the disease for reasons unrelated to pH balance.
Dr. Spiegel cautioned that the current data show only an association between PPI use and COVID-19 positivity; it cannot prove cause and effect.
Nevertheless, Dr. Spiegel said the findings should encourage physicians to prescribe PPIs only when clearly indicated. “If somebody is not yet on a PPI and you’re considering whether to start them on a PPI, it’s a good idea to consider H2 blockers,” he said.
People who need a daily dose of a PPI to control a severe condition can safely continue doing so, but such patients should take care to follow standard public health recommendations for avoiding exposure to the virus. These recommendations include wearing a mask, maintaining social distance, and washing hands frequently.
“People who are older, comorbid, or smokers – if they get infected, it could be severe,” he said. “[For] someone like that, it’s reasonable to ask, do we really need to be on twice-daily PPIs? There is good evidence that they are no better off than if they are taking once-daily doses.”
Brian Lacy, MD, PhD, a professor of medicine at the Mayo Clinic in Jacksonville, Fla., agreed that the study should prompt physicians to take a second look at their patients’ PPI prescriptions. “My view is that PPIs are frequently overused, and maybe this is one more piece of data that, if someone is on PPIs, maybe they don’t need to be on this medication.”
On the other hand, the drugs are important for treating conditions such as erosive esophagitis and healing ulcers, he said. The overall risk of contracting COVID-19 is low, so even this finding of a 3.7-fold increased risk should not lead patients or providers to stop taking or prescribing PPIs.
The study also lends support to the idea that the gastrointestinal tract could be involved in SARS-CoV-2 transmission, and it supports warnings about aerosols emitted from flushing toilets and through exhalation, Dr. Spiegel said. There is less evidence of the virus being transmitted through food. “It may not be fecal-oral; it may be fecal-respiratory,” he said.
The study was part of a larger project funded by Ironwood Pharmaceuticals. Dr. Spiegel reported relationships with Alnylam Pharmaceuticals, Arena Pharmaceuticals, Ironwood Pharmaceuticals, Salix Pharmaceuticals, Shire Pharmaceuticals, Synergy Pharmaceuticals, and Takeda Pharmaceuticals. Dr. Lacy has disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Easy access to PrEP reduces rates of HIV acquisition
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
When people were offered preexposure prophylaxis (PrEP) outside of traditional clinics, regardless of specific risk factors, as part of the Sustainable East Africa Research in Community Health (SEARCH) study, new HIV acquisitions dropped by 74%.
It’s a valuable lesson to providers around the world, said Catherine Koss, MD, assistant professor of medicine in HIV, infectious disease, and global medicine at the University of California, San Francisco.
“We haven’t really seen PrEP being scaled up and offered at such a broad level in communities,” Koss said during the International AIDS Conference 2020.
The first part of SEARCH, which looked at the impact of universal testing and access to HIV treatment immediately after diagnosis, showed that the strategy resulted in a population-wide 30% reduction in new HIV acquisitions. In other words, treatment alone wasn’t enough to end the HIV epidemic.
But the researchers always knew “there were likely going to be new HIV infections,” even with universal HIV testing and treatment, Koss said.
So the second part of the study was designed to see whether PrEP — with the combination of tenofovir disoproxil fumarate plus emtricitabine (Truvada, Gilead Sciences) — could further reduce rates of HIV acquisition.
PrEP out in the community
During the PrEP part of the SEARCH study, researchers discussed HIV risk with adults in 16 communities in rural Kenya and Uganda during population-level testing that took place at health fairs, beaches, trading centers, other community sites, and even in participants’ homes. PrEP was offered to anyone in a relationship with someone living with HIV, to anyone determined to be at elevated risk for infection by a previously validated algorithm, and to anyone who did not fit those criteria but who wanted a prescription.
Of the 15,632 adults eligible for PrEP, 5,447 (35%) chose to start the HIV prevention pill.
A rapid-enrollment protocol meant that people received their prescription at the time of screening or soon after that. Participants underwent testing for HIV antibodies — also out in the community — at weeks 4 and 12, and every 12 weeks thereafter; this will continue out to week 144.
HIV-negative adults who were part of the larger SEARCH cohort in the year before PrEP was made available — and from the same communities — served as the control group.
Interim 60-week data show that the rate of acquisition was 74% lower in the PrEP group than in the control group (incidence rate ratio, 0.26; P = .01). In women, the acquisition rate was 76% lower (incidence rate ratio, 0.24; P = .04), and in men, it was 40% lower (incidence rate ratio, 0.60; P = .54).
The reduction was not significant for men, probably because so few men acquired HIV, Koss reported. The powerful drop in new HIV cases overall was related to PrEP use by women; cases in women fell from 1.52 to 0.40 per 100 person-years.
Blood tests showed that 72% of the people who acquired HIV during the study period had not taken a PrEP pill for at least 30 days before their diagnosis.
“Making PrEP more easily accessible and more community-based could be very powerful in the United States,” said Koss.
“Allowing people to test for HIV and start PrEP outside of health clinics or standard health facilities could help reach more people,” she told Medscape Medical News. “Many of the people who benefit from PrEP may not otherwise need to seek medical care regularly if they’re otherwise healthy and often young.”
When PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV.
The findings were hailed by others in the field of HIV prevention.
“They’re fantastic,” said Jared Baeten, MD, vice dean of the School of Public Health and professor of global health, medicine, and epidemiology at the University of Washington in Seattle. He was involved in Partners PrEP, a study of PrEP use in mixed-HIV-status couples, the Partners Demonstration Project, and HOPE, a study of the dapivirine ring for HIV prevention.
“These data provide real evidence that when PrEP is made available — easily available — people will pick it up, they will take it away, they will put it in their mouths, and they will not get HIV,” he said in an interview.
Even more, they clarify something that has stymied American regulators and clinicians.
Early studies of PrEP use by single women were stopped because participants weren’t taking the pills; adherence was so low that researchers couldn’t show efficacy. Since then, various trials — including Partners PrEP — have shown that PrEP works in women, but doubts have lingered, leading women to “get the short end of the stick in discussions about PrEP,” Baeten explained.
“There really shouldn’t be questions anymore,” he said. “These findings should put to rest any question about women in Africa being able to benefit from PrEP.”
This article first appeared on Medscape.com.
What have we learned from COVID?
In 2015, I proposed virtual care for the division of adolescent medicine, to the administration of our Midwestern children and adolescent hospital; they gladly listened and accepted a copy of the resources I provided. Virtual care was acknowledged to be the future direction of our and other organizations.
Four years later, virtual visits were introduced in the pediatric urgent care, but with little usability as families were slow to adopt this new form of medicine. Fast forward to the COVID-19 crisis in March 2020, and virtual medicine was the only option to meet the needs of patients and to stop the economic consequences. Unfortunately, the expedited rollout at our and many other hospitals may have resulted in limited program development and a lack of shared best practices.
Since March 2020, both patients and medical providers have accepted virtual care, but we now have an opportunity to review some of the limitations to offering virtual care. Work in primary care centers may see limitations using virtual medicine to meet the needs of all patients. Take into consideration the ability to offer confidential care. Confidential care has been a challenge virtually. For example, while completing a virtual visit with a 19-year-old female, it was apparent she was not alone and when asked a benign question the commotion in the background told the real story. The young woman began to laugh and said, “That was my dad running out of the room.” Despite requesting that parents leave the call, they can be heard within earshot of the caller.
On a televisit, written words appear backwards on the video, requiring written questions to be mirror images. When asking questions meant to be confidential, we have used note cards with a question mark. Verbal directions asking the adolescent to give a thumbs up or down to answer the question are required to maintain privacy from others in the room. If the patient responds thumbs up, this leads to additional questions with note cards. Although not ideal, this process gets to the answers, and the adolescent can disclose confidential information without concern about being overheard. Child abuse and neglect professionals have found similar challenges talking to caregivers or children as they are uncertain if others in the home are out of the screen but listening to the questions or prompting responses.
Obtaining vitals may be restricted and picking up hypertension or changes in weight has been limited to face to face visits. To continue to provide virtual care will require screening stations. I foresee a kiosk at the grocery or drugstore with a computer and the ability to obtain vitals or portions of an exam such as heart and lung evaluations. Patients could go at their convenience and the results could be sent to their providers. Technology already exists to use a cell phone to take photos of a toddler’s sore ear drum, and to obtain basic pulse oximetry and ECG, but these have a cost and may be available only to those able to afford these tools.
Billing issues have developed when patients go to a lab on the same day as a virtual visit. Completing a virtual visit for a sore throat thought to be streptococcal pharyngitis should not be finalized without access to a streptococcal throat swab. Until families have home kits to evaluate for strep throat, the families must bring the patient to a clinic or lab to obtain a pharyngeal culture. Furthermore, insurance reimbursement standards will need to be set for ongoing virtual health to become a sustainable option.
Workflows have been disrupted by balancing face to face visits with virtual visits. Unless the virtual visit has been set up for the medical team to access immediately, there are delays accessing the virtual platform, resulting in unnecessary gaps in care. Arranging schedules to separate face to face visits from virtual visits offers more efficiency. Creating a block of virtual visits separated from face-to-face visits or assigning providers to virtual-only schedules may be the best option for an efficient clinic flow. Telemedicine visit templates may need to be created as virtual visits become standard practice.
At present, virtual visits can only be offered to English-speaking patients. The inability to offer translators limits access to a small number of patients. Given COVID-19’s impact on the underserved communities, having a safe resource to reach these patients has been limited, leaving face-to-face visits as their only option. Requiring a face-to-face visit during peak illness has placed patients at risk. They have refused health care as opposed to exposure to the illness in health care settings.
We have innovative opportunities to create a new health care system. Despite the initial struggles with the adoption of virtual care, patients and providers have begun embracing the technology. Best practices and shared resources will be required to have a successful system before brick and mortar organizations can be reduced or insurance companies create their own health care systems which can branch across state lines.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
The article was updated 7/17/2020.
In 2015, I proposed virtual care for the division of adolescent medicine, to the administration of our Midwestern children and adolescent hospital; they gladly listened and accepted a copy of the resources I provided. Virtual care was acknowledged to be the future direction of our and other organizations.
Four years later, virtual visits were introduced in the pediatric urgent care, but with little usability as families were slow to adopt this new form of medicine. Fast forward to the COVID-19 crisis in March 2020, and virtual medicine was the only option to meet the needs of patients and to stop the economic consequences. Unfortunately, the expedited rollout at our and many other hospitals may have resulted in limited program development and a lack of shared best practices.
Since March 2020, both patients and medical providers have accepted virtual care, but we now have an opportunity to review some of the limitations to offering virtual care. Work in primary care centers may see limitations using virtual medicine to meet the needs of all patients. Take into consideration the ability to offer confidential care. Confidential care has been a challenge virtually. For example, while completing a virtual visit with a 19-year-old female, it was apparent she was not alone and when asked a benign question the commotion in the background told the real story. The young woman began to laugh and said, “That was my dad running out of the room.” Despite requesting that parents leave the call, they can be heard within earshot of the caller.
On a televisit, written words appear backwards on the video, requiring written questions to be mirror images. When asking questions meant to be confidential, we have used note cards with a question mark. Verbal directions asking the adolescent to give a thumbs up or down to answer the question are required to maintain privacy from others in the room. If the patient responds thumbs up, this leads to additional questions with note cards. Although not ideal, this process gets to the answers, and the adolescent can disclose confidential information without concern about being overheard. Child abuse and neglect professionals have found similar challenges talking to caregivers or children as they are uncertain if others in the home are out of the screen but listening to the questions or prompting responses.
Obtaining vitals may be restricted and picking up hypertension or changes in weight has been limited to face to face visits. To continue to provide virtual care will require screening stations. I foresee a kiosk at the grocery or drugstore with a computer and the ability to obtain vitals or portions of an exam such as heart and lung evaluations. Patients could go at their convenience and the results could be sent to their providers. Technology already exists to use a cell phone to take photos of a toddler’s sore ear drum, and to obtain basic pulse oximetry and ECG, but these have a cost and may be available only to those able to afford these tools.
Billing issues have developed when patients go to a lab on the same day as a virtual visit. Completing a virtual visit for a sore throat thought to be streptococcal pharyngitis should not be finalized without access to a streptococcal throat swab. Until families have home kits to evaluate for strep throat, the families must bring the patient to a clinic or lab to obtain a pharyngeal culture. Furthermore, insurance reimbursement standards will need to be set for ongoing virtual health to become a sustainable option.
Workflows have been disrupted by balancing face to face visits with virtual visits. Unless the virtual visit has been set up for the medical team to access immediately, there are delays accessing the virtual platform, resulting in unnecessary gaps in care. Arranging schedules to separate face to face visits from virtual visits offers more efficiency. Creating a block of virtual visits separated from face-to-face visits or assigning providers to virtual-only schedules may be the best option for an efficient clinic flow. Telemedicine visit templates may need to be created as virtual visits become standard practice.
At present, virtual visits can only be offered to English-speaking patients. The inability to offer translators limits access to a small number of patients. Given COVID-19’s impact on the underserved communities, having a safe resource to reach these patients has been limited, leaving face-to-face visits as their only option. Requiring a face-to-face visit during peak illness has placed patients at risk. They have refused health care as opposed to exposure to the illness in health care settings.
We have innovative opportunities to create a new health care system. Despite the initial struggles with the adoption of virtual care, patients and providers have begun embracing the technology. Best practices and shared resources will be required to have a successful system before brick and mortar organizations can be reduced or insurance companies create their own health care systems which can branch across state lines.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
The article was updated 7/17/2020.
In 2015, I proposed virtual care for the division of adolescent medicine, to the administration of our Midwestern children and adolescent hospital; they gladly listened and accepted a copy of the resources I provided. Virtual care was acknowledged to be the future direction of our and other organizations.
Four years later, virtual visits were introduced in the pediatric urgent care, but with little usability as families were slow to adopt this new form of medicine. Fast forward to the COVID-19 crisis in March 2020, and virtual medicine was the only option to meet the needs of patients and to stop the economic consequences. Unfortunately, the expedited rollout at our and many other hospitals may have resulted in limited program development and a lack of shared best practices.
Since March 2020, both patients and medical providers have accepted virtual care, but we now have an opportunity to review some of the limitations to offering virtual care. Work in primary care centers may see limitations using virtual medicine to meet the needs of all patients. Take into consideration the ability to offer confidential care. Confidential care has been a challenge virtually. For example, while completing a virtual visit with a 19-year-old female, it was apparent she was not alone and when asked a benign question the commotion in the background told the real story. The young woman began to laugh and said, “That was my dad running out of the room.” Despite requesting that parents leave the call, they can be heard within earshot of the caller.
On a televisit, written words appear backwards on the video, requiring written questions to be mirror images. When asking questions meant to be confidential, we have used note cards with a question mark. Verbal directions asking the adolescent to give a thumbs up or down to answer the question are required to maintain privacy from others in the room. If the patient responds thumbs up, this leads to additional questions with note cards. Although not ideal, this process gets to the answers, and the adolescent can disclose confidential information without concern about being overheard. Child abuse and neglect professionals have found similar challenges talking to caregivers or children as they are uncertain if others in the home are out of the screen but listening to the questions or prompting responses.
Obtaining vitals may be restricted and picking up hypertension or changes in weight has been limited to face to face visits. To continue to provide virtual care will require screening stations. I foresee a kiosk at the grocery or drugstore with a computer and the ability to obtain vitals or portions of an exam such as heart and lung evaluations. Patients could go at their convenience and the results could be sent to their providers. Technology already exists to use a cell phone to take photos of a toddler’s sore ear drum, and to obtain basic pulse oximetry and ECG, but these have a cost and may be available only to those able to afford these tools.
Billing issues have developed when patients go to a lab on the same day as a virtual visit. Completing a virtual visit for a sore throat thought to be streptococcal pharyngitis should not be finalized without access to a streptococcal throat swab. Until families have home kits to evaluate for strep throat, the families must bring the patient to a clinic or lab to obtain a pharyngeal culture. Furthermore, insurance reimbursement standards will need to be set for ongoing virtual health to become a sustainable option.
Workflows have been disrupted by balancing face to face visits with virtual visits. Unless the virtual visit has been set up for the medical team to access immediately, there are delays accessing the virtual platform, resulting in unnecessary gaps in care. Arranging schedules to separate face to face visits from virtual visits offers more efficiency. Creating a block of virtual visits separated from face-to-face visits or assigning providers to virtual-only schedules may be the best option for an efficient clinic flow. Telemedicine visit templates may need to be created as virtual visits become standard practice.
At present, virtual visits can only be offered to English-speaking patients. The inability to offer translators limits access to a small number of patients. Given COVID-19’s impact on the underserved communities, having a safe resource to reach these patients has been limited, leaving face-to-face visits as their only option. Requiring a face-to-face visit during peak illness has placed patients at risk. They have refused health care as opposed to exposure to the illness in health care settings.
We have innovative opportunities to create a new health care system. Despite the initial struggles with the adoption of virtual care, patients and providers have begun embracing the technology. Best practices and shared resources will be required to have a successful system before brick and mortar organizations can be reduced or insurance companies create their own health care systems which can branch across state lines.
Ms. Thew is the medical director of the department of adolescent medicine at Children’s Wisconsin in Milwaukee. She said she had no relevant financial disclosures. Email her at pdnews@mdedge.com.
The article was updated 7/17/2020.
Zika virus syndrome may adversely affect children normocephalic at birth
Microcephaly may be the hallmark of congenital Zika virus syndrome, but neurologic abnormalities also are common in normocephalic children exposed to the virus in utero, according to data from a large pediatric referral center in Rio de Janeiro.
The retrospective analysis demonstrated that there is a “spectrum of clinical manifestations” in children with congenital Zika virus syndrome, including those who “had initially been perceived as developing normally based on [head circumference],” Jessica S. Cranston, a medical student at the University of California, Los Angeles, and associates wrote in JAMA Network Open.
Previous studies have described the poor clinical outcomes in Zika virus–exposed infants with microcephaly, but the current analysis evaluated head circumference (HC) as a continuous variable and stratified outcomes according to the presence or absence of microcephaly, they explained.
In the cohort of 215 children referred to Instituto Fernandes Figueira who had laboratory-confirmed antenatal Zika virus exposure, 53 had microcephaly (cephalic perimeter z score of less than –2 standard deviations) and 162 were normocephalic, the investigators said.
The children were evaluated monthly for the first 6 months of life and then every 3 months. Neurodevelopmental evaluation with the Bayley Scales of Infant and Toddler Development, Third Edition, between 6 months and 3 years of age showed that all of those with microcephaly had abnormal neuromotor findings. All but two of the children with microcephaly had abnormal neuroimaging results, and 38 (72%) had failure to thrive, they reported.
Among the children with normocephaly at birth, 68% had abnormal neurologic findings, including hyperreflexia (27%), abnormal tone (39%), and other congenital neuromotor signs (42%). Results of neuroimaging results, primarily in the form of transfontanelle ultrasonography, were abnormal in 29% of children with normocephaly.
“Infants with a larger birth HC, within the normocephalic range (±2 SDs), had higher overall neurodevelopmental scores on the Bayley-III assessment,” Sarah B. Mulkey, MD, PhD, said in an invited commentary, “whereas infants with a smaller birth HC within the normocephalic range had lower scores in the domains of cognitive and language functions.”
If HC measurements could be combined with early neurologic data such as the results of neuroimaging or a neurological exam, she suggested, it might provide “a practical tool to help determine risk for adverse clinical outcomes in a [Zika virus–]exposed infant at birth that can be widely used in a variety of follow-up settings.”
In nutritional assessments performed for 143 children with normocephaly, 51% had failure to thrive “because of neurologic repercussions leading to poor feeding,” Ms. Cranston and associates wrote, adding that 15 of the 73 (21%) infants with normocephaly and failure to thrive developed secondary microcephaly.
Altogether, 17 of the 162 (10.5%) children with normocephaly developed microcephaly during the follow-up, with the reverse – microcephaly resolving in infants who were microcephalic at birth – occurring in 4 of the 53 (7.5%) affected infants, indicating that “head circumference was not static,” they said.
“The trajectory of head growth is critical,” said Dr. Mulkey of the Prenatal Pediatrics Institute at Children’s National Hospital in Washington. “The neurologic outcome of a child who develops postnatal microcephaly would be very concerning compared with an infant who is born with normocephaly and maintains a steady HC percentile over time.”
HC is just one piece of the puzzle, however, since children with Zika virus syndrome may exhibit “a variety of manifestations and outcomes.” This lack of certainty suggests that “careful monitoring and evaluation of children with suspected exposure is essential for ensuring early detection of possible disabilities and referral to interventional services,” the investigators wrote.
The findings of this study “are both highly statistically significant and clinically significant,”said Kevin T. Powell, MD, PhD, a pediatric hospitalist and clinical ethics consultant living in St. Louis who was not associated with the study.
“While outcomes at birth are dichotomized into those with and without microcephaly, the developmental outcomes measured at 3 years of age are on a spectrum. ... Those with microcephaly tend to be more severely affected, but many infants with small but normal-sized heads are also mild to moderately impacted. The flip side is that 64% of infected babies ended up with average or better development” based on Bayley-III evaluations, said Dr. Powell, who is a member of the Pediatric News editorial advisory board.
The study was funded by grants from the National Institute of Allergy and Infectious Diseases, the National Eye Institute, and the Thrasher Foundation and by awards from Brazil’s National Council of Scientific and Technological Development; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro. Individual investigators received fees and grants from these and other organizations.
Dr. Mulkey received a contract from the Centers for Disease Control and Prevention for technical expertise for Zika virus studies and received support for Zika studies from the Thrasher Research Fund. Dr. Powell had no relevant financial disclosures.
SOURCE: Cranston JS et al. JAMA Netw Open. 2020 July 7;3(7):e209303.
Microcephaly may be the hallmark of congenital Zika virus syndrome, but neurologic abnormalities also are common in normocephalic children exposed to the virus in utero, according to data from a large pediatric referral center in Rio de Janeiro.
The retrospective analysis demonstrated that there is a “spectrum of clinical manifestations” in children with congenital Zika virus syndrome, including those who “had initially been perceived as developing normally based on [head circumference],” Jessica S. Cranston, a medical student at the University of California, Los Angeles, and associates wrote in JAMA Network Open.
Previous studies have described the poor clinical outcomes in Zika virus–exposed infants with microcephaly, but the current analysis evaluated head circumference (HC) as a continuous variable and stratified outcomes according to the presence or absence of microcephaly, they explained.
In the cohort of 215 children referred to Instituto Fernandes Figueira who had laboratory-confirmed antenatal Zika virus exposure, 53 had microcephaly (cephalic perimeter z score of less than –2 standard deviations) and 162 were normocephalic, the investigators said.
The children were evaluated monthly for the first 6 months of life and then every 3 months. Neurodevelopmental evaluation with the Bayley Scales of Infant and Toddler Development, Third Edition, between 6 months and 3 years of age showed that all of those with microcephaly had abnormal neuromotor findings. All but two of the children with microcephaly had abnormal neuroimaging results, and 38 (72%) had failure to thrive, they reported.
Among the children with normocephaly at birth, 68% had abnormal neurologic findings, including hyperreflexia (27%), abnormal tone (39%), and other congenital neuromotor signs (42%). Results of neuroimaging results, primarily in the form of transfontanelle ultrasonography, were abnormal in 29% of children with normocephaly.
“Infants with a larger birth HC, within the normocephalic range (±2 SDs), had higher overall neurodevelopmental scores on the Bayley-III assessment,” Sarah B. Mulkey, MD, PhD, said in an invited commentary, “whereas infants with a smaller birth HC within the normocephalic range had lower scores in the domains of cognitive and language functions.”
If HC measurements could be combined with early neurologic data such as the results of neuroimaging or a neurological exam, she suggested, it might provide “a practical tool to help determine risk for adverse clinical outcomes in a [Zika virus–]exposed infant at birth that can be widely used in a variety of follow-up settings.”
In nutritional assessments performed for 143 children with normocephaly, 51% had failure to thrive “because of neurologic repercussions leading to poor feeding,” Ms. Cranston and associates wrote, adding that 15 of the 73 (21%) infants with normocephaly and failure to thrive developed secondary microcephaly.
Altogether, 17 of the 162 (10.5%) children with normocephaly developed microcephaly during the follow-up, with the reverse – microcephaly resolving in infants who were microcephalic at birth – occurring in 4 of the 53 (7.5%) affected infants, indicating that “head circumference was not static,” they said.
“The trajectory of head growth is critical,” said Dr. Mulkey of the Prenatal Pediatrics Institute at Children’s National Hospital in Washington. “The neurologic outcome of a child who develops postnatal microcephaly would be very concerning compared with an infant who is born with normocephaly and maintains a steady HC percentile over time.”
HC is just one piece of the puzzle, however, since children with Zika virus syndrome may exhibit “a variety of manifestations and outcomes.” This lack of certainty suggests that “careful monitoring and evaluation of children with suspected exposure is essential for ensuring early detection of possible disabilities and referral to interventional services,” the investigators wrote.
The findings of this study “are both highly statistically significant and clinically significant,”said Kevin T. Powell, MD, PhD, a pediatric hospitalist and clinical ethics consultant living in St. Louis who was not associated with the study.
“While outcomes at birth are dichotomized into those with and without microcephaly, the developmental outcomes measured at 3 years of age are on a spectrum. ... Those with microcephaly tend to be more severely affected, but many infants with small but normal-sized heads are also mild to moderately impacted. The flip side is that 64% of infected babies ended up with average or better development” based on Bayley-III evaluations, said Dr. Powell, who is a member of the Pediatric News editorial advisory board.
The study was funded by grants from the National Institute of Allergy and Infectious Diseases, the National Eye Institute, and the Thrasher Foundation and by awards from Brazil’s National Council of Scientific and Technological Development; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro. Individual investigators received fees and grants from these and other organizations.
Dr. Mulkey received a contract from the Centers for Disease Control and Prevention for technical expertise for Zika virus studies and received support for Zika studies from the Thrasher Research Fund. Dr. Powell had no relevant financial disclosures.
SOURCE: Cranston JS et al. JAMA Netw Open. 2020 July 7;3(7):e209303.
Microcephaly may be the hallmark of congenital Zika virus syndrome, but neurologic abnormalities also are common in normocephalic children exposed to the virus in utero, according to data from a large pediatric referral center in Rio de Janeiro.
The retrospective analysis demonstrated that there is a “spectrum of clinical manifestations” in children with congenital Zika virus syndrome, including those who “had initially been perceived as developing normally based on [head circumference],” Jessica S. Cranston, a medical student at the University of California, Los Angeles, and associates wrote in JAMA Network Open.
Previous studies have described the poor clinical outcomes in Zika virus–exposed infants with microcephaly, but the current analysis evaluated head circumference (HC) as a continuous variable and stratified outcomes according to the presence or absence of microcephaly, they explained.
In the cohort of 215 children referred to Instituto Fernandes Figueira who had laboratory-confirmed antenatal Zika virus exposure, 53 had microcephaly (cephalic perimeter z score of less than –2 standard deviations) and 162 were normocephalic, the investigators said.
The children were evaluated monthly for the first 6 months of life and then every 3 months. Neurodevelopmental evaluation with the Bayley Scales of Infant and Toddler Development, Third Edition, between 6 months and 3 years of age showed that all of those with microcephaly had abnormal neuromotor findings. All but two of the children with microcephaly had abnormal neuroimaging results, and 38 (72%) had failure to thrive, they reported.
Among the children with normocephaly at birth, 68% had abnormal neurologic findings, including hyperreflexia (27%), abnormal tone (39%), and other congenital neuromotor signs (42%). Results of neuroimaging results, primarily in the form of transfontanelle ultrasonography, were abnormal in 29% of children with normocephaly.
“Infants with a larger birth HC, within the normocephalic range (±2 SDs), had higher overall neurodevelopmental scores on the Bayley-III assessment,” Sarah B. Mulkey, MD, PhD, said in an invited commentary, “whereas infants with a smaller birth HC within the normocephalic range had lower scores in the domains of cognitive and language functions.”
If HC measurements could be combined with early neurologic data such as the results of neuroimaging or a neurological exam, she suggested, it might provide “a practical tool to help determine risk for adverse clinical outcomes in a [Zika virus–]exposed infant at birth that can be widely used in a variety of follow-up settings.”
In nutritional assessments performed for 143 children with normocephaly, 51% had failure to thrive “because of neurologic repercussions leading to poor feeding,” Ms. Cranston and associates wrote, adding that 15 of the 73 (21%) infants with normocephaly and failure to thrive developed secondary microcephaly.
Altogether, 17 of the 162 (10.5%) children with normocephaly developed microcephaly during the follow-up, with the reverse – microcephaly resolving in infants who were microcephalic at birth – occurring in 4 of the 53 (7.5%) affected infants, indicating that “head circumference was not static,” they said.
“The trajectory of head growth is critical,” said Dr. Mulkey of the Prenatal Pediatrics Institute at Children’s National Hospital in Washington. “The neurologic outcome of a child who develops postnatal microcephaly would be very concerning compared with an infant who is born with normocephaly and maintains a steady HC percentile over time.”
HC is just one piece of the puzzle, however, since children with Zika virus syndrome may exhibit “a variety of manifestations and outcomes.” This lack of certainty suggests that “careful monitoring and evaluation of children with suspected exposure is essential for ensuring early detection of possible disabilities and referral to interventional services,” the investigators wrote.
The findings of this study “are both highly statistically significant and clinically significant,”said Kevin T. Powell, MD, PhD, a pediatric hospitalist and clinical ethics consultant living in St. Louis who was not associated with the study.
“While outcomes at birth are dichotomized into those with and without microcephaly, the developmental outcomes measured at 3 years of age are on a spectrum. ... Those with microcephaly tend to be more severely affected, but many infants with small but normal-sized heads are also mild to moderately impacted. The flip side is that 64% of infected babies ended up with average or better development” based on Bayley-III evaluations, said Dr. Powell, who is a member of the Pediatric News editorial advisory board.
The study was funded by grants from the National Institute of Allergy and Infectious Diseases, the National Eye Institute, and the Thrasher Foundation and by awards from Brazil’s National Council of Scientific and Technological Development; Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro. Individual investigators received fees and grants from these and other organizations.
Dr. Mulkey received a contract from the Centers for Disease Control and Prevention for technical expertise for Zika virus studies and received support for Zika studies from the Thrasher Research Fund. Dr. Powell had no relevant financial disclosures.
SOURCE: Cranston JS et al. JAMA Netw Open. 2020 July 7;3(7):e209303.
FROM JAMA NETWORK OPEN
Vitamin D supplementation may reduce negative symptoms of MDD
Key clinical point: Vitamin D supplementation may reduce negative emotions in patients with major depressive disorder (MDD).
Major finding: Vitamin D supplementation reduced negative emotions at doses of ≤4,000 IU/day (Hedges' g = −0.2311; P = .0008). In the sub-group analysis, the effects were significant in patients with serum levels of 25(OH)D ≤50 nmol/L (P = .0028), but not in those with levels >50 nmol/L (P = .0507).
Study details: Systematic review and meta-analysis of 25 randomized controlled trials (n = 7,534) comparing the effects of vitamin D and the placebo on negative emotions in patients with MDD.
Disclosures: No funding information was identified. The authors declared no conflicts of interest.
Citation: Cheng YC et al. Depress Anxiety. 2020 May 04. doi: 10.1002/da.23025.
Key clinical point: Vitamin D supplementation may reduce negative emotions in patients with major depressive disorder (MDD).
Major finding: Vitamin D supplementation reduced negative emotions at doses of ≤4,000 IU/day (Hedges' g = −0.2311; P = .0008). In the sub-group analysis, the effects were significant in patients with serum levels of 25(OH)D ≤50 nmol/L (P = .0028), but not in those with levels >50 nmol/L (P = .0507).
Study details: Systematic review and meta-analysis of 25 randomized controlled trials (n = 7,534) comparing the effects of vitamin D and the placebo on negative emotions in patients with MDD.
Disclosures: No funding information was identified. The authors declared no conflicts of interest.
Citation: Cheng YC et al. Depress Anxiety. 2020 May 04. doi: 10.1002/da.23025.
Key clinical point: Vitamin D supplementation may reduce negative emotions in patients with major depressive disorder (MDD).
Major finding: Vitamin D supplementation reduced negative emotions at doses of ≤4,000 IU/day (Hedges' g = −0.2311; P = .0008). In the sub-group analysis, the effects were significant in patients with serum levels of 25(OH)D ≤50 nmol/L (P = .0028), but not in those with levels >50 nmol/L (P = .0507).
Study details: Systematic review and meta-analysis of 25 randomized controlled trials (n = 7,534) comparing the effects of vitamin D and the placebo on negative emotions in patients with MDD.
Disclosures: No funding information was identified. The authors declared no conflicts of interest.
Citation: Cheng YC et al. Depress Anxiety. 2020 May 04. doi: 10.1002/da.23025.