User login
Elevated inflammation common in children’s severe COVID-19 disease
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
according to data from 50 patients at a single tertiary care center.
“Risk factors for severe disease in pediatric populations have not been clearly identified and the high prevalence of SARS-CoV-2 in NYC offers an opportunity to describe severe pediatric disease in more detail,” wrote Philip Zachariah, MD, of New York–Presbyterian Hospital, New York, and colleagues.
In a retrospective case series published in JAMA Pediatrics, the researchers reviewed data from 50 patients: 41 classified as severe and 9 classified as nonsevere. Among the patients, 27 were male and 25 were Hispanic. The patient population had a median of 2 days from symptom onset to hospital admission. The most common symptoms were fever (80%) and respiratory symptoms (64%). Seventy-six percent of patients had a median length of stay of 3 days (range 1-30 days).
At hospital admission, children with severe disease had significantly higher levels of several inflammatory markers compared with those without severe disease, notably C-reactive protein (median 8.978 mg/dL vs. 0.64 mg/dL) and procalcitonin (median 0.31 ng/mL vs. 0.17 ng/mL, (P < .001 for both). High mean peak levels of C-reactive protein, procalcitonin, interleukin 6, ferritin, and D-dimer were seen among the nine children (16%) who required mechanical ventilation, Dr. Zachariah and associates said.
None of the 14 infants and 1 of the 8 immunocompromised children in the study had severe disease, the researchers wrote.
Bacterial coinfections detected while patients were hospitalized were bacteremia in 6%, suspected bacterial pneumonia in 18%, urinary tract infections in 10%, skin and soft tissue infections in 6%, and streptococcus pharyngitis in 2%, Dr. Zachariah and associates reported.
Overall, 61% of the children had comorbidities identified in previous COVID-19 studies, of which obesity was the most common (22%); other comorbidities included asthma, sickle cell disease, cardiac disease, and diabetes. Obesity also was significantly associated with the need for mechanical ventilation in children aged 2 years and older (67%). A total of 16 patients required respiratory support, 9 of these were placed on mechanical ventilation; 6 of these 9 children were obese.
Fifteen patients (30%) who met criteria for increased oxygen requirements and respiratory distress received hydroxychloroquine, but the small sample size did not allow for assessment of treatment efficacy, the researchers said.
“Expanding our knowledge of COVID-19 [disease] in children will potentially permit early recognition of SARS-CoV-2 infection, understanding of the natural history of disease, and potential complications, said Stephen I. Pelton, MD, professor of pediatrics and epidemiology at Boston University and senior attending physician at Boston Medical Center. This review of 50 SARS-CoV-2 infected children (less than 21 years of age) “provides insight into the short period of symptoms prior to hospitalization, challenges the concept that infants less than 1 year are at greatest risk of severe disease (as from the experience in China), and suggests rapid recovery in many children, as median length of stay was 3 days.
“The review revealed two findings that were surprising to me. First, the median length of stay of 3 days. As nearly 20% of the children required mechanical ventilation, it suggests many of the children were discharged quickly after evaluation, suggesting that we need to identify markers of severity to predict those children likely to have progressive disease and require respiratory support,” Dr. Pelton noted.
“The second observation suggests high rates of bacterial infection (bacteremia, pneumonia, UTI, and skin and soft tissue infection). I do not think this has been widely reported in adults, and may represent a difference between child and adult disease. More studies such as this will be required to identify how common coinfection with bacteria is,” he said.
“The take-home message is that although most children with COVID-19 have a mild or even asymptomatic course, some become severely ill requiring ventilator support and potentially ECMO [extracorporeal membrane oxygenation]. Potential predictors of severity include high C-reactive protein, obesity, and older age [adolescence], said Dr. Pelton, who was not involved in the study.
What additional research is needed? Dr. Pelton said that better markers of severe disease are needed, as well as an understanding of why obesity is a risk factor for severe disease in both children and adults. Are these prediabetic patients? he asked.
The study findings were limited by the small sample size and high proportion of Hispanic patients, which may limit generalizability, and some symptoms and comorbidities may have been missed because of the retrospective nature of the study, the researchers noted. However, the results support the need for hospitals to remain vigilant to the variable presentations of COVID-19 infections in children.
“Therapeutic considerations need to [include] the risk of toxicity, control of antiviral replication, and early recognition and management of immune dysregulation,” they concluded.
The study received no outside funding. Dr. Zachariah had no financial conflicts to disclose. Two coauthors reported ties with various pharmaceutical companies and organizations. Dr. Pelton said he had no relevant financial disclosures.
SOURCE: Zachariah P et al. JAMA Pediatr. 2020 June 3. doi:10.1001/jamapediatrics.2020.2430.
FROM JAMA PEDIATRICS
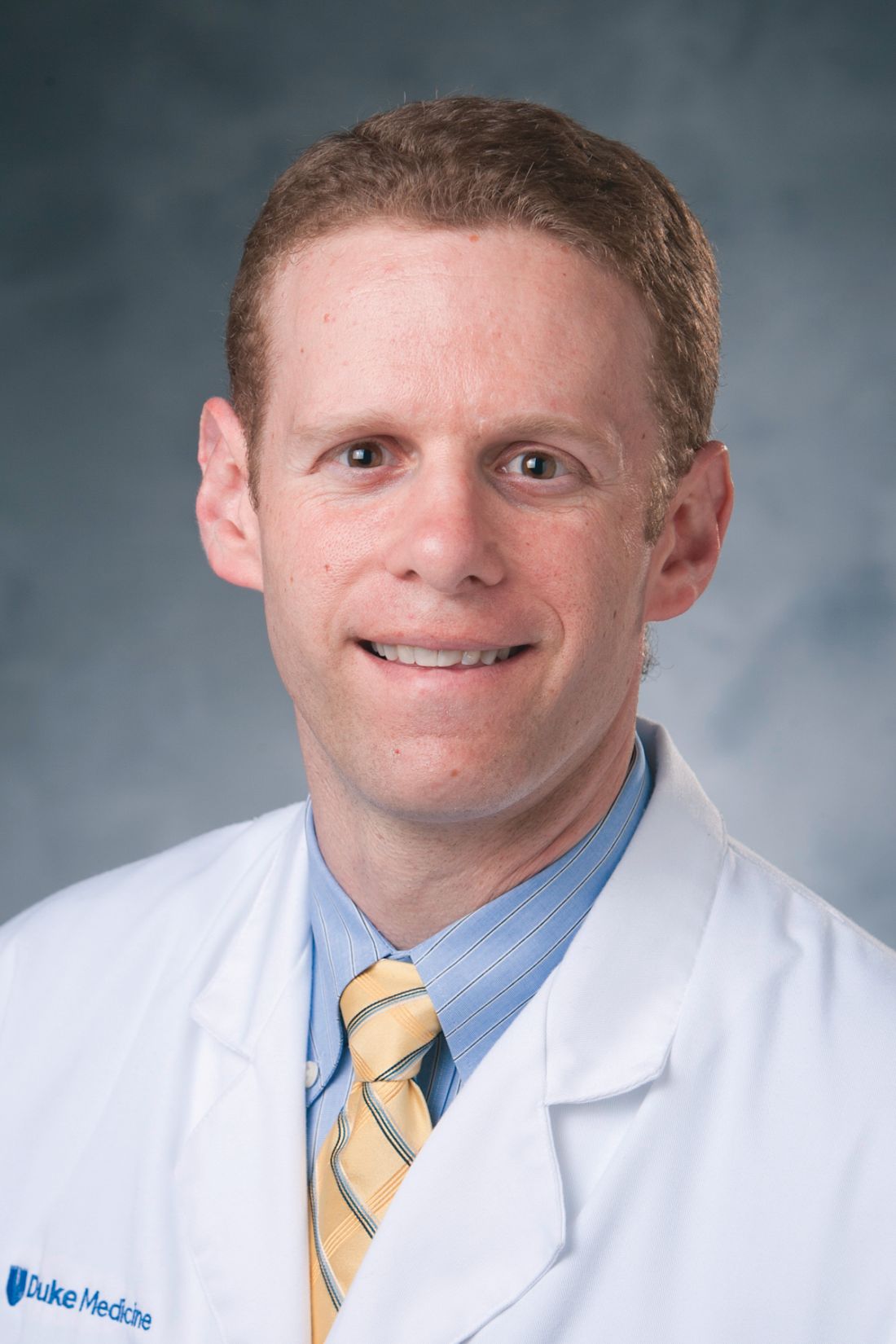
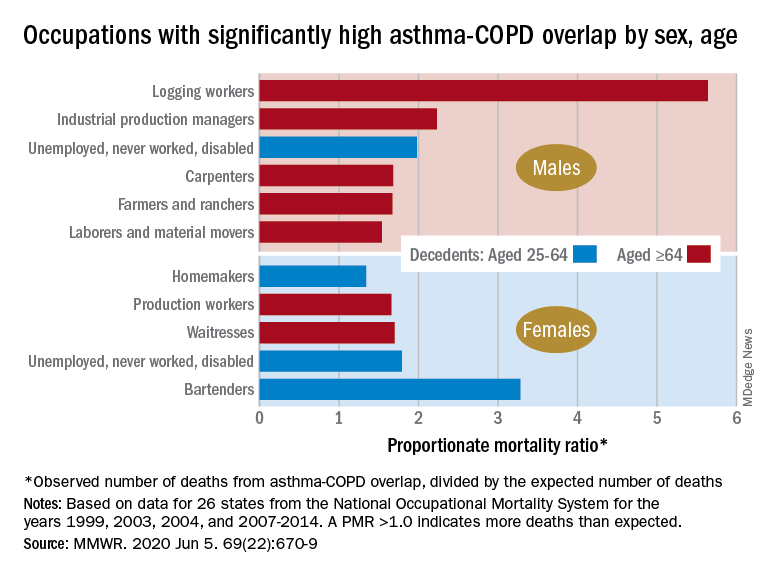
By the numbers: Asthma-COPD overlap deaths
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
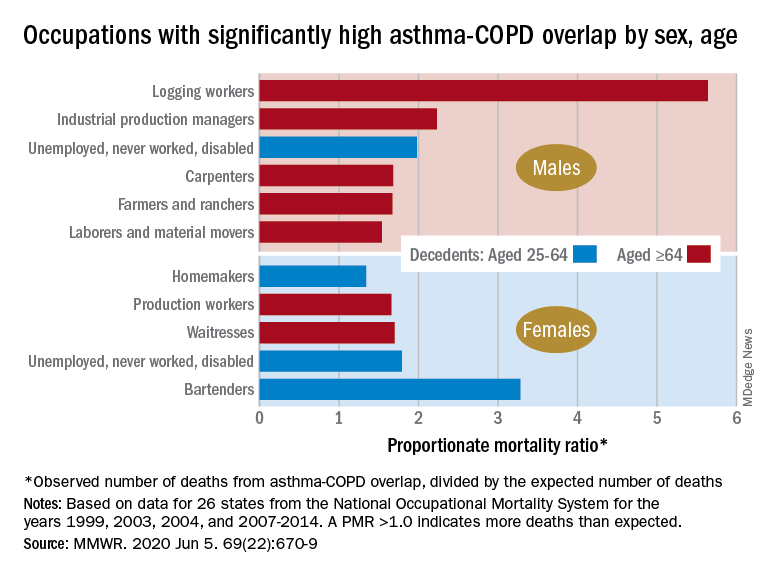
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
FROM MMWR
Rapid changes to health system spurred by COVID might be here to stay
The U.S. health care system is famously resistant to government-imposed change. It took decades to create Medicare and Medicaid, mostly because of opposition from the medical-industrial complex. Then it was nearly another half-century before the passage of the Affordable Care Act.
“Health care is never going back to the way it was before,” said Gail Wilensky, a health economist who ran the Medicare and Medicaid programs for President George H.W. Bush in the early 1990s.
Ms. Wilensky is far from the only longtime observer of the American health care system to marvel at the speed of some long-sought changes. But experts warn that the breakthroughs may not all make the health system work better or make it less expensive.
That said, here are three trends that seem likely to continue.
Telehealth for all
Telehealth is not new; medical professionals have used it to reach patients in rural or remote settings since the late 1980s.
But even while technology has made video visits easier, it has failed to reach critical mass, largely because of political fights. Licensing has been one main obstacle – determining how a doctor in one state can legally treat a patient in a state where the doctor is not licensed.
The other obstacle, not surprisingly, is payment. Should a video visit be reimbursed at the same rate as an in-person visit? Will making it easier for doctors and other medical professionals to use telehealth encourage unnecessary care, thus driving up the nation’s $3.6 trillion health tab even more? Or could it replace care once provided free by phone?
Still, the pandemic has pushed aside those sticking points. Almost overnight, by necessity, every health care provider who can is delivering telemedicine. A new survey from Gallup found the number of patients reporting “virtual” medical visits more than doubled, from 12% to 27%, from late March to mid-May. That is attributable, at least in part, to Medicare having made it easier for doctors to bill for virtual visits.
It’s easy to see why many patients like video visits – there’s no parking to find and pay for, and it takes far less time out of a workday than going to an office.
Doctors and other practitioners seem more ambivalent. On one hand, it can be harder to examine a patient over video and some services just can’t be done via a digital connection. On the other hand, they can see more patients in the same amount of time and may need less support staff and possibly smaller offices if more visits are conducted virtually.
Of course, telemedicine doesn’t work for everyone. Many areas and patients don’t have reliable or robust broadband connections that make video visits work. And some patients, particularly the oldest seniors, lack the technological skills needed to connect.
Primary care doctors in peril
Another trend that has suddenly accelerated is worry over the nation’s dwindling supply of primary care doctors. The exodus of practitioners performing primary care has been a concern over the past several years, as baby boomer doctors retire and others have grown weary of more and more bureaucracy from government and private payers. Having faced a difficult financial crisis during the pandemic, more family physicians may move into retirement or seek other professional options.
At the same time, fewer current medical students are choosing specialties in primary care.
“I’ve been trying to raise the alarm about the kind of perilous future of primary care,” said Farzad Mostashari, MD, a top Department of Health & Human Services official in the Obama administration. Dr. Mostashari runs Aledade, a company that helps primary care doctors make the transition from fee-for-service medicine to new payment models.
The American Academy of Family Physicians reports that 70% of primary care physicians are reporting declines in patient volume of 50% or more since March, and 40% have laid off or furloughed staff. The AAFP has joined other primary care and insurance groups in asking HHS for an infusion of cash.
“This is absolutely essential to effectively treat patients today and to maintain their ongoing operations until we overcome this public health emergency,” the groups wrote.
One easy way to help keep primary care doctors afloat would be to pay them not according to what they do, but in a lump sum to keep patients healthy. This move from fee-for-service to what’s known as capitation or value-based care has unfolded gradually and was championed in the Affordable Care Act.
But some experts argue it needs to happen more quickly and they predict that the coronavirus pandemic could finally mark the beginning of the end for doctors who still charge for each service individually. Dr. Mostashari, who spends his time helping doctors make the transition, said in times like these, it would make more sense for primary care doctors to have “a steady monthly revenue stream, and [the doctor] can decide the best way to deliver that care: unlimited texts, phone calls, video calls. The goal is to give you satisfactory outcomes and a great patient experience.”
Still, many physicians, particularly those in solo or small practices, worry about the potential financial risk – especially the possibility of getting paid less if they don’t meet certain benchmarks that the doctors may not be able to directly control.
But with many practices now ground to a halt, or just starting to reopen, those physicians who get paid per patient rather than per service are in a much better position to stay afloat. That model may gain traction as doctors ponder the next pandemic, or the next wave of this one.
Hospitals on the decline?
The pandemic also might lead to less emphasis on hospital-based care. While hospitals in many parts of the country have obviously been full of very sick COVID patients, they have closed down other nonemergency services to preserve supplies and resources to fight the pandemic. People with other ailments have stayed away in droves even when services were available, for fear of catching something worse than what they already have.
Many experts predict that care won’t just snap back when the current emergency wanes. Mark Smith, MD, former president of the California Health Care Foundation, said among consumers, a switch has been flipped. “Overnight it seems we’ve gone from high-touch to no-touch.”
Which is not great for hospitals that have spent millions trying to attract patients to their labor-and-delivery units, orthopedic centers, and other parts of the facility that once generated lots of income.
Even more concerning is that hospitals’ ability to weather the current financial shock varies widely. Those most in danger of closing are in rural and underserved areas, where patients could wind up with even less access to care that is scarce already.
All of which underscores the point that not all these changes will necessarily be good for the health system or society. Financial pressures could end up driving more consolidation, which could push up prices as large groups of hospitals and doctors gain more bargaining clout.
But the changes are definitely happening at a pace few have ever seen, said Ms. Wilensky, “When you’re forced to find different ways of doing things, and you find out they are easier and more efficient, it’s going to be hard to go back to the old way.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The U.S. health care system is famously resistant to government-imposed change. It took decades to create Medicare and Medicaid, mostly because of opposition from the medical-industrial complex. Then it was nearly another half-century before the passage of the Affordable Care Act.
“Health care is never going back to the way it was before,” said Gail Wilensky, a health economist who ran the Medicare and Medicaid programs for President George H.W. Bush in the early 1990s.
Ms. Wilensky is far from the only longtime observer of the American health care system to marvel at the speed of some long-sought changes. But experts warn that the breakthroughs may not all make the health system work better or make it less expensive.
That said, here are three trends that seem likely to continue.
Telehealth for all
Telehealth is not new; medical professionals have used it to reach patients in rural or remote settings since the late 1980s.
But even while technology has made video visits easier, it has failed to reach critical mass, largely because of political fights. Licensing has been one main obstacle – determining how a doctor in one state can legally treat a patient in a state where the doctor is not licensed.
The other obstacle, not surprisingly, is payment. Should a video visit be reimbursed at the same rate as an in-person visit? Will making it easier for doctors and other medical professionals to use telehealth encourage unnecessary care, thus driving up the nation’s $3.6 trillion health tab even more? Or could it replace care once provided free by phone?
Still, the pandemic has pushed aside those sticking points. Almost overnight, by necessity, every health care provider who can is delivering telemedicine. A new survey from Gallup found the number of patients reporting “virtual” medical visits more than doubled, from 12% to 27%, from late March to mid-May. That is attributable, at least in part, to Medicare having made it easier for doctors to bill for virtual visits.
It’s easy to see why many patients like video visits – there’s no parking to find and pay for, and it takes far less time out of a workday than going to an office.
Doctors and other practitioners seem more ambivalent. On one hand, it can be harder to examine a patient over video and some services just can’t be done via a digital connection. On the other hand, they can see more patients in the same amount of time and may need less support staff and possibly smaller offices if more visits are conducted virtually.
Of course, telemedicine doesn’t work for everyone. Many areas and patients don’t have reliable or robust broadband connections that make video visits work. And some patients, particularly the oldest seniors, lack the technological skills needed to connect.
Primary care doctors in peril
Another trend that has suddenly accelerated is worry over the nation’s dwindling supply of primary care doctors. The exodus of practitioners performing primary care has been a concern over the past several years, as baby boomer doctors retire and others have grown weary of more and more bureaucracy from government and private payers. Having faced a difficult financial crisis during the pandemic, more family physicians may move into retirement or seek other professional options.
At the same time, fewer current medical students are choosing specialties in primary care.
“I’ve been trying to raise the alarm about the kind of perilous future of primary care,” said Farzad Mostashari, MD, a top Department of Health & Human Services official in the Obama administration. Dr. Mostashari runs Aledade, a company that helps primary care doctors make the transition from fee-for-service medicine to new payment models.
The American Academy of Family Physicians reports that 70% of primary care physicians are reporting declines in patient volume of 50% or more since March, and 40% have laid off or furloughed staff. The AAFP has joined other primary care and insurance groups in asking HHS for an infusion of cash.
“This is absolutely essential to effectively treat patients today and to maintain their ongoing operations until we overcome this public health emergency,” the groups wrote.
One easy way to help keep primary care doctors afloat would be to pay them not according to what they do, but in a lump sum to keep patients healthy. This move from fee-for-service to what’s known as capitation or value-based care has unfolded gradually and was championed in the Affordable Care Act.
But some experts argue it needs to happen more quickly and they predict that the coronavirus pandemic could finally mark the beginning of the end for doctors who still charge for each service individually. Dr. Mostashari, who spends his time helping doctors make the transition, said in times like these, it would make more sense for primary care doctors to have “a steady monthly revenue stream, and [the doctor] can decide the best way to deliver that care: unlimited texts, phone calls, video calls. The goal is to give you satisfactory outcomes and a great patient experience.”
Still, many physicians, particularly those in solo or small practices, worry about the potential financial risk – especially the possibility of getting paid less if they don’t meet certain benchmarks that the doctors may not be able to directly control.
But with many practices now ground to a halt, or just starting to reopen, those physicians who get paid per patient rather than per service are in a much better position to stay afloat. That model may gain traction as doctors ponder the next pandemic, or the next wave of this one.
Hospitals on the decline?
The pandemic also might lead to less emphasis on hospital-based care. While hospitals in many parts of the country have obviously been full of very sick COVID patients, they have closed down other nonemergency services to preserve supplies and resources to fight the pandemic. People with other ailments have stayed away in droves even when services were available, for fear of catching something worse than what they already have.
Many experts predict that care won’t just snap back when the current emergency wanes. Mark Smith, MD, former president of the California Health Care Foundation, said among consumers, a switch has been flipped. “Overnight it seems we’ve gone from high-touch to no-touch.”
Which is not great for hospitals that have spent millions trying to attract patients to their labor-and-delivery units, orthopedic centers, and other parts of the facility that once generated lots of income.
Even more concerning is that hospitals’ ability to weather the current financial shock varies widely. Those most in danger of closing are in rural and underserved areas, where patients could wind up with even less access to care that is scarce already.
All of which underscores the point that not all these changes will necessarily be good for the health system or society. Financial pressures could end up driving more consolidation, which could push up prices as large groups of hospitals and doctors gain more bargaining clout.
But the changes are definitely happening at a pace few have ever seen, said Ms. Wilensky, “When you’re forced to find different ways of doing things, and you find out they are easier and more efficient, it’s going to be hard to go back to the old way.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
The U.S. health care system is famously resistant to government-imposed change. It took decades to create Medicare and Medicaid, mostly because of opposition from the medical-industrial complex. Then it was nearly another half-century before the passage of the Affordable Care Act.
“Health care is never going back to the way it was before,” said Gail Wilensky, a health economist who ran the Medicare and Medicaid programs for President George H.W. Bush in the early 1990s.
Ms. Wilensky is far from the only longtime observer of the American health care system to marvel at the speed of some long-sought changes. But experts warn that the breakthroughs may not all make the health system work better or make it less expensive.
That said, here are three trends that seem likely to continue.
Telehealth for all
Telehealth is not new; medical professionals have used it to reach patients in rural or remote settings since the late 1980s.
But even while technology has made video visits easier, it has failed to reach critical mass, largely because of political fights. Licensing has been one main obstacle – determining how a doctor in one state can legally treat a patient in a state where the doctor is not licensed.
The other obstacle, not surprisingly, is payment. Should a video visit be reimbursed at the same rate as an in-person visit? Will making it easier for doctors and other medical professionals to use telehealth encourage unnecessary care, thus driving up the nation’s $3.6 trillion health tab even more? Or could it replace care once provided free by phone?
Still, the pandemic has pushed aside those sticking points. Almost overnight, by necessity, every health care provider who can is delivering telemedicine. A new survey from Gallup found the number of patients reporting “virtual” medical visits more than doubled, from 12% to 27%, from late March to mid-May. That is attributable, at least in part, to Medicare having made it easier for doctors to bill for virtual visits.
It’s easy to see why many patients like video visits – there’s no parking to find and pay for, and it takes far less time out of a workday than going to an office.
Doctors and other practitioners seem more ambivalent. On one hand, it can be harder to examine a patient over video and some services just can’t be done via a digital connection. On the other hand, they can see more patients in the same amount of time and may need less support staff and possibly smaller offices if more visits are conducted virtually.
Of course, telemedicine doesn’t work for everyone. Many areas and patients don’t have reliable or robust broadband connections that make video visits work. And some patients, particularly the oldest seniors, lack the technological skills needed to connect.
Primary care doctors in peril
Another trend that has suddenly accelerated is worry over the nation’s dwindling supply of primary care doctors. The exodus of practitioners performing primary care has been a concern over the past several years, as baby boomer doctors retire and others have grown weary of more and more bureaucracy from government and private payers. Having faced a difficult financial crisis during the pandemic, more family physicians may move into retirement or seek other professional options.
At the same time, fewer current medical students are choosing specialties in primary care.
“I’ve been trying to raise the alarm about the kind of perilous future of primary care,” said Farzad Mostashari, MD, a top Department of Health & Human Services official in the Obama administration. Dr. Mostashari runs Aledade, a company that helps primary care doctors make the transition from fee-for-service medicine to new payment models.
The American Academy of Family Physicians reports that 70% of primary care physicians are reporting declines in patient volume of 50% or more since March, and 40% have laid off or furloughed staff. The AAFP has joined other primary care and insurance groups in asking HHS for an infusion of cash.
“This is absolutely essential to effectively treat patients today and to maintain their ongoing operations until we overcome this public health emergency,” the groups wrote.
One easy way to help keep primary care doctors afloat would be to pay them not according to what they do, but in a lump sum to keep patients healthy. This move from fee-for-service to what’s known as capitation or value-based care has unfolded gradually and was championed in the Affordable Care Act.
But some experts argue it needs to happen more quickly and they predict that the coronavirus pandemic could finally mark the beginning of the end for doctors who still charge for each service individually. Dr. Mostashari, who spends his time helping doctors make the transition, said in times like these, it would make more sense for primary care doctors to have “a steady monthly revenue stream, and [the doctor] can decide the best way to deliver that care: unlimited texts, phone calls, video calls. The goal is to give you satisfactory outcomes and a great patient experience.”
Still, many physicians, particularly those in solo or small practices, worry about the potential financial risk – especially the possibility of getting paid less if they don’t meet certain benchmarks that the doctors may not be able to directly control.
But with many practices now ground to a halt, or just starting to reopen, those physicians who get paid per patient rather than per service are in a much better position to stay afloat. That model may gain traction as doctors ponder the next pandemic, or the next wave of this one.
Hospitals on the decline?
The pandemic also might lead to less emphasis on hospital-based care. While hospitals in many parts of the country have obviously been full of very sick COVID patients, they have closed down other nonemergency services to preserve supplies and resources to fight the pandemic. People with other ailments have stayed away in droves even when services were available, for fear of catching something worse than what they already have.
Many experts predict that care won’t just snap back when the current emergency wanes. Mark Smith, MD, former president of the California Health Care Foundation, said among consumers, a switch has been flipped. “Overnight it seems we’ve gone from high-touch to no-touch.”
Which is not great for hospitals that have spent millions trying to attract patients to their labor-and-delivery units, orthopedic centers, and other parts of the facility that once generated lots of income.
Even more concerning is that hospitals’ ability to weather the current financial shock varies widely. Those most in danger of closing are in rural and underserved areas, where patients could wind up with even less access to care that is scarce already.
All of which underscores the point that not all these changes will necessarily be good for the health system or society. Financial pressures could end up driving more consolidation, which could push up prices as large groups of hospitals and doctors gain more bargaining clout.
But the changes are definitely happening at a pace few have ever seen, said Ms. Wilensky, “When you’re forced to find different ways of doing things, and you find out they are easier and more efficient, it’s going to be hard to go back to the old way.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Pandemic conditions can complicate care of patients with PAH
in these patients, according to a research article published in Pulmonary Circulation.
“The impetus for this manuscript was a recent discussion within the Pulmonary Hypertension Association (PHA) and [its] Scientific Leadership Council who expressed a need for guidelines from experts in the field,” wrote John J. Ryan, MD, of the University of Utah, Salt Lake City, and colleagues.
The authors highlight some of the unique challenges in caring for patients with pulmonary hypertension (PH), particularly pulmonary arterial hypertension (PAH), in the context of the COVID-19 pandemic.
Telemedicine and temporary visit schedules for new and returning PAH patients can help reduce risk of virus transmission, if patient accessibility to telemedicine is feasible. Protocols to reduce the risk of virus exposure or transmission in the office setting included less frequent echocardiography and 6-Minute Walk Tests (6MWTs) for patients in stable condition. In stable patients, “avoid pulmonary function of V/Q tests when possible,” the authors wrote.
New patients who have been referred for PAH present a challenge in conducting a thorough evaluation that would normally include measurement of invasive hemodynamics in keeping with current diagnostic guidelines. Clinicians will need to balance the potential risks of COVID-19 exposure during elective procedures against the benefits of full evaluations to plan PAH treatment, the authors noted.
For established patients who are clinically stable, remote visits may be an option, with a risk/benefit assessment of the need for in-person diagnostic tests at the current time, they said. However, telemedicine’s limitations include not only patient accessibility and understanding of audio and video technology, but also inability to accurately measure vital signs, they said.
As for routine testing such as echocardiograms, 6MWTs, and other laboratory testing, “it is important to consider the additive value of these sometimes comprehensive tests in the context of the risks associated with visiting the hospital or clinic to obtain them,” the authors said.
Patients who are unstable and experience worsening right heart failure (RHF) at home may have contracted a COVID-19 infection, but the differential diagnosis includes sepsis, ischemia, and PAH disease progression. “During the current pandemic, fever at home in a PAH patient should be assumed to represent a COVID-19 infection,” and patients with worsening respiratory symptoms that require hospitalization should be tested for COVID-19, the authors emphasized.
Use of ECMO or other intensive interventions should be considered in the context of risk assessment, the authors said. “As a general recommendation, practitioners should consider utilizing an established PAH-specific risk assessment tool to help identify patients who are more likely to survive heroic interventions during the COVID-19 outbreak,” they wrote.
Training and education of PH providers will continue to be limited by the pandemic, and many clinical trials and research programs have been suspended and will need to be restructured to minimize risk of transmission of the COVID-19 virus, the authors said. However, health care providers must continue to provide PAH patients and families with advice and updates in best practices, while “acknowledging that the situation changes rapidly,” they concluded.
Dr. Ryan disclosed participating on the speakers bureau, and provides consulting services for, Actelion and Bayer, as well as research support from the Reagan Corporation, the Gordon Family, and the Cushman Family.
SOURCE: Ryan JJ et al. Pulm Circ. 2020 Apr 29. doi: 10.1177/2045894020920153.
in these patients, according to a research article published in Pulmonary Circulation.
“The impetus for this manuscript was a recent discussion within the Pulmonary Hypertension Association (PHA) and [its] Scientific Leadership Council who expressed a need for guidelines from experts in the field,” wrote John J. Ryan, MD, of the University of Utah, Salt Lake City, and colleagues.
The authors highlight some of the unique challenges in caring for patients with pulmonary hypertension (PH), particularly pulmonary arterial hypertension (PAH), in the context of the COVID-19 pandemic.
Telemedicine and temporary visit schedules for new and returning PAH patients can help reduce risk of virus transmission, if patient accessibility to telemedicine is feasible. Protocols to reduce the risk of virus exposure or transmission in the office setting included less frequent echocardiography and 6-Minute Walk Tests (6MWTs) for patients in stable condition. In stable patients, “avoid pulmonary function of V/Q tests when possible,” the authors wrote.
New patients who have been referred for PAH present a challenge in conducting a thorough evaluation that would normally include measurement of invasive hemodynamics in keeping with current diagnostic guidelines. Clinicians will need to balance the potential risks of COVID-19 exposure during elective procedures against the benefits of full evaluations to plan PAH treatment, the authors noted.
For established patients who are clinically stable, remote visits may be an option, with a risk/benefit assessment of the need for in-person diagnostic tests at the current time, they said. However, telemedicine’s limitations include not only patient accessibility and understanding of audio and video technology, but also inability to accurately measure vital signs, they said.
As for routine testing such as echocardiograms, 6MWTs, and other laboratory testing, “it is important to consider the additive value of these sometimes comprehensive tests in the context of the risks associated with visiting the hospital or clinic to obtain them,” the authors said.
Patients who are unstable and experience worsening right heart failure (RHF) at home may have contracted a COVID-19 infection, but the differential diagnosis includes sepsis, ischemia, and PAH disease progression. “During the current pandemic, fever at home in a PAH patient should be assumed to represent a COVID-19 infection,” and patients with worsening respiratory symptoms that require hospitalization should be tested for COVID-19, the authors emphasized.
Use of ECMO or other intensive interventions should be considered in the context of risk assessment, the authors said. “As a general recommendation, practitioners should consider utilizing an established PAH-specific risk assessment tool to help identify patients who are more likely to survive heroic interventions during the COVID-19 outbreak,” they wrote.
Training and education of PH providers will continue to be limited by the pandemic, and many clinical trials and research programs have been suspended and will need to be restructured to minimize risk of transmission of the COVID-19 virus, the authors said. However, health care providers must continue to provide PAH patients and families with advice and updates in best practices, while “acknowledging that the situation changes rapidly,” they concluded.
Dr. Ryan disclosed participating on the speakers bureau, and provides consulting services for, Actelion and Bayer, as well as research support from the Reagan Corporation, the Gordon Family, and the Cushman Family.
SOURCE: Ryan JJ et al. Pulm Circ. 2020 Apr 29. doi: 10.1177/2045894020920153.
in these patients, according to a research article published in Pulmonary Circulation.
“The impetus for this manuscript was a recent discussion within the Pulmonary Hypertension Association (PHA) and [its] Scientific Leadership Council who expressed a need for guidelines from experts in the field,” wrote John J. Ryan, MD, of the University of Utah, Salt Lake City, and colleagues.
The authors highlight some of the unique challenges in caring for patients with pulmonary hypertension (PH), particularly pulmonary arterial hypertension (PAH), in the context of the COVID-19 pandemic.
Telemedicine and temporary visit schedules for new and returning PAH patients can help reduce risk of virus transmission, if patient accessibility to telemedicine is feasible. Protocols to reduce the risk of virus exposure or transmission in the office setting included less frequent echocardiography and 6-Minute Walk Tests (6MWTs) for patients in stable condition. In stable patients, “avoid pulmonary function of V/Q tests when possible,” the authors wrote.
New patients who have been referred for PAH present a challenge in conducting a thorough evaluation that would normally include measurement of invasive hemodynamics in keeping with current diagnostic guidelines. Clinicians will need to balance the potential risks of COVID-19 exposure during elective procedures against the benefits of full evaluations to plan PAH treatment, the authors noted.
For established patients who are clinically stable, remote visits may be an option, with a risk/benefit assessment of the need for in-person diagnostic tests at the current time, they said. However, telemedicine’s limitations include not only patient accessibility and understanding of audio and video technology, but also inability to accurately measure vital signs, they said.
As for routine testing such as echocardiograms, 6MWTs, and other laboratory testing, “it is important to consider the additive value of these sometimes comprehensive tests in the context of the risks associated with visiting the hospital or clinic to obtain them,” the authors said.
Patients who are unstable and experience worsening right heart failure (RHF) at home may have contracted a COVID-19 infection, but the differential diagnosis includes sepsis, ischemia, and PAH disease progression. “During the current pandemic, fever at home in a PAH patient should be assumed to represent a COVID-19 infection,” and patients with worsening respiratory symptoms that require hospitalization should be tested for COVID-19, the authors emphasized.
Use of ECMO or other intensive interventions should be considered in the context of risk assessment, the authors said. “As a general recommendation, practitioners should consider utilizing an established PAH-specific risk assessment tool to help identify patients who are more likely to survive heroic interventions during the COVID-19 outbreak,” they wrote.
Training and education of PH providers will continue to be limited by the pandemic, and many clinical trials and research programs have been suspended and will need to be restructured to minimize risk of transmission of the COVID-19 virus, the authors said. However, health care providers must continue to provide PAH patients and families with advice and updates in best practices, while “acknowledging that the situation changes rapidly,” they concluded.
Dr. Ryan disclosed participating on the speakers bureau, and provides consulting services for, Actelion and Bayer, as well as research support from the Reagan Corporation, the Gordon Family, and the Cushman Family.
SOURCE: Ryan JJ et al. Pulm Circ. 2020 Apr 29. doi: 10.1177/2045894020920153.
FROM PULMONARY CIRCULATION
American Cancer Society update: ‘It is best not to drink alcohol’
In its updated cancer prevention guidelines, the American Cancer Society now recommends that “it is best not to drink alcohol.”
Previously, ACS suggested that, for those who consume alcoholic beverages, intake should be no more than one drink per day for women or two per day for men. That recommendation is still in place, but is now accompanied by this new, stronger directive.
The revised guidelines also place more emphasis on reducing the consumption of processed and red meat and highly processed foods, and on increasing physical activity.
But importantly, there is also a call for action from public, private, and community organizations to work to together to increase access to affordable, nutritious foods and physical activity.
“Making healthy choices can be challenging for many, and there are strategies included in the guidelines that communities can undertake to help reduce barriers to eating well and physical activity,” said Laura Makaroff, DO, American Cancer Society senior vice president. “Individual choice is an important part of a healthy lifestyle, but having the right policies and environmental factors to break down these barriers is also important, and that is something that clinicians can support.”
The guidelines were published in CA: A Cancer Journal for Clinicians.
The link between cancer and lifestyle factors has long been established, and for the past 4 decades, both government and leading nonprofit health organizations, including the ACS and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), have released cancer prevention guidelines and recommendations that focus on managing weight, diet, physical activity, and alcohol consumption.
In 2012, the ACS issued guidelines on diet and physical activity, and their current guideline is largely based on the WCRF/AICR systematic reviews and Continuous Update Project reports, which were last updated in 2018. The ACS guidelines also incorporated systematic reviews conducted by the International Agency on Cancer Research (IARC) and the U.S. Department of Agriculture and the Department of Health and Human Services (USDA/HHS) and other analyses that were published since the WCRF/AICR recommendations were released.
Emphasis on three areas
The differences between the old guidelines and the update do not differ dramatically, but Makaroff highlighted a few areas that have increased emphasis.
Time spent being physically active is critical. The recommendation has changed to encourage adults to engage in 150-300 minutes (2.5-5 hours) of moderate-intensity physical activity, or 75-150 minutes (1.25-2.5 hours) of vigorous-intensity physical activity, or an equivalent combination, per week. Achieving or exceeding the upper limit of 300 minutes is optimal.
“That is more than what we have recommended in the past, along with the continued message that children and adolescents engage in at least 1 hour of moderate- or vigorous-intensity activity each day,” she told Medscape Medical News.
The ACS has also increased emphasis on reducing the consumption of processed and red meat. “This is part of a healthy eating pattern and making sure that people are eating food that is high in nutrients that help achieve and maintain a healthy body weight,” said Makaroff.
A healthy diet should include a variety of dark green, red, and orange vegetables; fiber-rich legumes; and fruits with a variety of colors and whole grains, according to the guidelines. Sugar-sweetened beverages, highly processed foods, and refined grain products should be limited or avoided.
The revised dietary recommendations reflect a shift from a “reductionist or nutrient-centric” approach to one that is more “holistic” and that focuses on dietary patterns. In contrast to a focus on individual nutrients and bioactive compounds, the new approach is more consistent with what and how people actually eat, ACS points out.
The third area that Makaroff highlighted is alcohol, where the recommendation is to avoid or limit consumption. “The current update says not to drink alcohol, which is in line with the scientific evidence, but for those people who choose to drink alcohol, to limit it to one drink per day for women and two drinks per day for men.”
Thus, the change here is that the previous guideline only recommended limiting alcohol consumption, while the update suggests that, optimally, it should be avoided completely.
The ACS has also called for community involvement to help implement these goals: “Public, private, and community organizations should work collaboratively at national, state, and local levels to develop, advocate for, and implement policy and environmental changes that increase access to affordable, nutritious foods; provide safe, enjoyable, and accessible opportunities for physical activity; and limit alcohol for all individuals.”
No smoking guns
Commenting on the guidelines, Steven K. Clinton, MD, PhD, associate director of the Center for Advanced Functional Foods Research and Entrepreneurship at the Ohio State University, Columbus, explained that he didn’t view the change in alcohol as that much of an evolution. “It’s been 8 years since they revised their overall guidelines, and during that time frame, there has been an enormous growth in the evidence that has been used by many organizations,” he said.
Clinton noted that the guidelines are consistent with the whole body of current scientific literature. “It’s very easy to go to the document and look for the ‘smoking gun’ – but the smoking gun is really not one thing,” he said. “It’s a pattern, and what dietitians and nutritionists are telling people is that you need to orchestrate a healthy lifestyle and diet, with a diet that has a foundation of fruits, vegetables, whole grains, and modest intake of refined grains and meat. You are orchestrating an entire pattern to get the maximum benefit.”
Makaroff is an employee of the ACS. Clinton has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
In its updated cancer prevention guidelines, the American Cancer Society now recommends that “it is best not to drink alcohol.”
Previously, ACS suggested that, for those who consume alcoholic beverages, intake should be no more than one drink per day for women or two per day for men. That recommendation is still in place, but is now accompanied by this new, stronger directive.
The revised guidelines also place more emphasis on reducing the consumption of processed and red meat and highly processed foods, and on increasing physical activity.
But importantly, there is also a call for action from public, private, and community organizations to work to together to increase access to affordable, nutritious foods and physical activity.
“Making healthy choices can be challenging for many, and there are strategies included in the guidelines that communities can undertake to help reduce barriers to eating well and physical activity,” said Laura Makaroff, DO, American Cancer Society senior vice president. “Individual choice is an important part of a healthy lifestyle, but having the right policies and environmental factors to break down these barriers is also important, and that is something that clinicians can support.”
The guidelines were published in CA: A Cancer Journal for Clinicians.
The link between cancer and lifestyle factors has long been established, and for the past 4 decades, both government and leading nonprofit health organizations, including the ACS and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), have released cancer prevention guidelines and recommendations that focus on managing weight, diet, physical activity, and alcohol consumption.
In 2012, the ACS issued guidelines on diet and physical activity, and their current guideline is largely based on the WCRF/AICR systematic reviews and Continuous Update Project reports, which were last updated in 2018. The ACS guidelines also incorporated systematic reviews conducted by the International Agency on Cancer Research (IARC) and the U.S. Department of Agriculture and the Department of Health and Human Services (USDA/HHS) and other analyses that were published since the WCRF/AICR recommendations were released.
Emphasis on three areas
The differences between the old guidelines and the update do not differ dramatically, but Makaroff highlighted a few areas that have increased emphasis.
Time spent being physically active is critical. The recommendation has changed to encourage adults to engage in 150-300 minutes (2.5-5 hours) of moderate-intensity physical activity, or 75-150 minutes (1.25-2.5 hours) of vigorous-intensity physical activity, or an equivalent combination, per week. Achieving or exceeding the upper limit of 300 minutes is optimal.
“That is more than what we have recommended in the past, along with the continued message that children and adolescents engage in at least 1 hour of moderate- or vigorous-intensity activity each day,” she told Medscape Medical News.
The ACS has also increased emphasis on reducing the consumption of processed and red meat. “This is part of a healthy eating pattern and making sure that people are eating food that is high in nutrients that help achieve and maintain a healthy body weight,” said Makaroff.
A healthy diet should include a variety of dark green, red, and orange vegetables; fiber-rich legumes; and fruits with a variety of colors and whole grains, according to the guidelines. Sugar-sweetened beverages, highly processed foods, and refined grain products should be limited or avoided.
The revised dietary recommendations reflect a shift from a “reductionist or nutrient-centric” approach to one that is more “holistic” and that focuses on dietary patterns. In contrast to a focus on individual nutrients and bioactive compounds, the new approach is more consistent with what and how people actually eat, ACS points out.
The third area that Makaroff highlighted is alcohol, where the recommendation is to avoid or limit consumption. “The current update says not to drink alcohol, which is in line with the scientific evidence, but for those people who choose to drink alcohol, to limit it to one drink per day for women and two drinks per day for men.”
Thus, the change here is that the previous guideline only recommended limiting alcohol consumption, while the update suggests that, optimally, it should be avoided completely.
The ACS has also called for community involvement to help implement these goals: “Public, private, and community organizations should work collaboratively at national, state, and local levels to develop, advocate for, and implement policy and environmental changes that increase access to affordable, nutritious foods; provide safe, enjoyable, and accessible opportunities for physical activity; and limit alcohol for all individuals.”
No smoking guns
Commenting on the guidelines, Steven K. Clinton, MD, PhD, associate director of the Center for Advanced Functional Foods Research and Entrepreneurship at the Ohio State University, Columbus, explained that he didn’t view the change in alcohol as that much of an evolution. “It’s been 8 years since they revised their overall guidelines, and during that time frame, there has been an enormous growth in the evidence that has been used by many organizations,” he said.
Clinton noted that the guidelines are consistent with the whole body of current scientific literature. “It’s very easy to go to the document and look for the ‘smoking gun’ – but the smoking gun is really not one thing,” he said. “It’s a pattern, and what dietitians and nutritionists are telling people is that you need to orchestrate a healthy lifestyle and diet, with a diet that has a foundation of fruits, vegetables, whole grains, and modest intake of refined grains and meat. You are orchestrating an entire pattern to get the maximum benefit.”
Makaroff is an employee of the ACS. Clinton has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
In its updated cancer prevention guidelines, the American Cancer Society now recommends that “it is best not to drink alcohol.”
Previously, ACS suggested that, for those who consume alcoholic beverages, intake should be no more than one drink per day for women or two per day for men. That recommendation is still in place, but is now accompanied by this new, stronger directive.
The revised guidelines also place more emphasis on reducing the consumption of processed and red meat and highly processed foods, and on increasing physical activity.
But importantly, there is also a call for action from public, private, and community organizations to work to together to increase access to affordable, nutritious foods and physical activity.
“Making healthy choices can be challenging for many, and there are strategies included in the guidelines that communities can undertake to help reduce barriers to eating well and physical activity,” said Laura Makaroff, DO, American Cancer Society senior vice president. “Individual choice is an important part of a healthy lifestyle, but having the right policies and environmental factors to break down these barriers is also important, and that is something that clinicians can support.”
The guidelines were published in CA: A Cancer Journal for Clinicians.
The link between cancer and lifestyle factors has long been established, and for the past 4 decades, both government and leading nonprofit health organizations, including the ACS and the World Cancer Research Fund/American Institute for Cancer Research (WCRF/AICR), have released cancer prevention guidelines and recommendations that focus on managing weight, diet, physical activity, and alcohol consumption.
In 2012, the ACS issued guidelines on diet and physical activity, and their current guideline is largely based on the WCRF/AICR systematic reviews and Continuous Update Project reports, which were last updated in 2018. The ACS guidelines also incorporated systematic reviews conducted by the International Agency on Cancer Research (IARC) and the U.S. Department of Agriculture and the Department of Health and Human Services (USDA/HHS) and other analyses that were published since the WCRF/AICR recommendations were released.
Emphasis on three areas
The differences between the old guidelines and the update do not differ dramatically, but Makaroff highlighted a few areas that have increased emphasis.
Time spent being physically active is critical. The recommendation has changed to encourage adults to engage in 150-300 minutes (2.5-5 hours) of moderate-intensity physical activity, or 75-150 minutes (1.25-2.5 hours) of vigorous-intensity physical activity, or an equivalent combination, per week. Achieving or exceeding the upper limit of 300 minutes is optimal.
“That is more than what we have recommended in the past, along with the continued message that children and adolescents engage in at least 1 hour of moderate- or vigorous-intensity activity each day,” she told Medscape Medical News.
The ACS has also increased emphasis on reducing the consumption of processed and red meat. “This is part of a healthy eating pattern and making sure that people are eating food that is high in nutrients that help achieve and maintain a healthy body weight,” said Makaroff.
A healthy diet should include a variety of dark green, red, and orange vegetables; fiber-rich legumes; and fruits with a variety of colors and whole grains, according to the guidelines. Sugar-sweetened beverages, highly processed foods, and refined grain products should be limited or avoided.
The revised dietary recommendations reflect a shift from a “reductionist or nutrient-centric” approach to one that is more “holistic” and that focuses on dietary patterns. In contrast to a focus on individual nutrients and bioactive compounds, the new approach is more consistent with what and how people actually eat, ACS points out.
The third area that Makaroff highlighted is alcohol, where the recommendation is to avoid or limit consumption. “The current update says not to drink alcohol, which is in line with the scientific evidence, but for those people who choose to drink alcohol, to limit it to one drink per day for women and two drinks per day for men.”
Thus, the change here is that the previous guideline only recommended limiting alcohol consumption, while the update suggests that, optimally, it should be avoided completely.
The ACS has also called for community involvement to help implement these goals: “Public, private, and community organizations should work collaboratively at national, state, and local levels to develop, advocate for, and implement policy and environmental changes that increase access to affordable, nutritious foods; provide safe, enjoyable, and accessible opportunities for physical activity; and limit alcohol for all individuals.”
No smoking guns
Commenting on the guidelines, Steven K. Clinton, MD, PhD, associate director of the Center for Advanced Functional Foods Research and Entrepreneurship at the Ohio State University, Columbus, explained that he didn’t view the change in alcohol as that much of an evolution. “It’s been 8 years since they revised their overall guidelines, and during that time frame, there has been an enormous growth in the evidence that has been used by many organizations,” he said.
Clinton noted that the guidelines are consistent with the whole body of current scientific literature. “It’s very easy to go to the document and look for the ‘smoking gun’ – but the smoking gun is really not one thing,” he said. “It’s a pattern, and what dietitians and nutritionists are telling people is that you need to orchestrate a healthy lifestyle and diet, with a diet that has a foundation of fruits, vegetables, whole grains, and modest intake of refined grains and meat. You are orchestrating an entire pattern to get the maximum benefit.”
Makaroff is an employee of the ACS. Clinton has disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Aspirin and warfarin together leads to increased bleeding without reducing thrombotic events
Background: Current guidelines recommend against using aspirin in combination with warfarin for patients with AFib, unless the patient has another indication for aspirin such as recent percutaneous coronary intervention (PCI) or a mechanical heart valve. These recommendations are based on limited clinical trial data that showed an increased risk of adverse events with combination therapy without clinical benefit. Despite these recommendations, recent studies have shown that aspirin use without a clinical indication remains common in patients taking warfarin for AFib. The prevalence of aspirin use without a clinical indication in patients taking warfarin for VTE is less well studied.
Study design: Registry-based cohort study.
Setting: Six anticoagulation clinics in Michigan.
Synopsis: Of the 6,539 patients included in the study, 2,453 patients (37.5%) were taking both warfarin and aspirin without an indication for aspirin therapy; 3,688 propensity score–matched patients (1,844 in each group) were compared to assess rates of bleeding and rates of observed thrombosis at 1 year in patients taking warfarin alone versus warfarin plus aspirin. Patients treated with warfarin plus aspirin experienced more bleeding events than did patients on warfarin monotherapy (95% confidence interval, 23.8%-28.3% vs. 95% CI, 18.3%-22.3%; P less than .001). Rates of observed thrombosis were similar between the two groups (95% CI, 1.6%-3.1% vs. 95% CI, 2.0%-3.6%; P = .40). This study demonstrates that aspirin use without a clinical indication remains common in patients taking warfarin for AFib or VTE, and that reducing inappropriate aspirin use in this patient population may help prevent adverse outcomes.
Bottom line: Use of aspirin without a clinical indication in patients taking warfarin is common and is associated with an increased risk of bleeding without significant clinical benefit.
Citation: Schaefer JK et al. Association of adding aspirin to warfarin therapy without an apparent indication with bleeding and other adverse events. JAMA Intern Med. 2019 Mar 4;179(4):533-41.
Dr. Wachter is an associate medical director at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Current guidelines recommend against using aspirin in combination with warfarin for patients with AFib, unless the patient has another indication for aspirin such as recent percutaneous coronary intervention (PCI) or a mechanical heart valve. These recommendations are based on limited clinical trial data that showed an increased risk of adverse events with combination therapy without clinical benefit. Despite these recommendations, recent studies have shown that aspirin use without a clinical indication remains common in patients taking warfarin for AFib. The prevalence of aspirin use without a clinical indication in patients taking warfarin for VTE is less well studied.
Study design: Registry-based cohort study.
Setting: Six anticoagulation clinics in Michigan.
Synopsis: Of the 6,539 patients included in the study, 2,453 patients (37.5%) were taking both warfarin and aspirin without an indication for aspirin therapy; 3,688 propensity score–matched patients (1,844 in each group) were compared to assess rates of bleeding and rates of observed thrombosis at 1 year in patients taking warfarin alone versus warfarin plus aspirin. Patients treated with warfarin plus aspirin experienced more bleeding events than did patients on warfarin monotherapy (95% confidence interval, 23.8%-28.3% vs. 95% CI, 18.3%-22.3%; P less than .001). Rates of observed thrombosis were similar between the two groups (95% CI, 1.6%-3.1% vs. 95% CI, 2.0%-3.6%; P = .40). This study demonstrates that aspirin use without a clinical indication remains common in patients taking warfarin for AFib or VTE, and that reducing inappropriate aspirin use in this patient population may help prevent adverse outcomes.
Bottom line: Use of aspirin without a clinical indication in patients taking warfarin is common and is associated with an increased risk of bleeding without significant clinical benefit.
Citation: Schaefer JK et al. Association of adding aspirin to warfarin therapy without an apparent indication with bleeding and other adverse events. JAMA Intern Med. 2019 Mar 4;179(4):533-41.
Dr. Wachter is an associate medical director at Duke Regional Hospital and an assistant professor of medicine at Duke University.
Background: Current guidelines recommend against using aspirin in combination with warfarin for patients with AFib, unless the patient has another indication for aspirin such as recent percutaneous coronary intervention (PCI) or a mechanical heart valve. These recommendations are based on limited clinical trial data that showed an increased risk of adverse events with combination therapy without clinical benefit. Despite these recommendations, recent studies have shown that aspirin use without a clinical indication remains common in patients taking warfarin for AFib. The prevalence of aspirin use without a clinical indication in patients taking warfarin for VTE is less well studied.
Study design: Registry-based cohort study.
Setting: Six anticoagulation clinics in Michigan.
Synopsis: Of the 6,539 patients included in the study, 2,453 patients (37.5%) were taking both warfarin and aspirin without an indication for aspirin therapy; 3,688 propensity score–matched patients (1,844 in each group) were compared to assess rates of bleeding and rates of observed thrombosis at 1 year in patients taking warfarin alone versus warfarin plus aspirin. Patients treated with warfarin plus aspirin experienced more bleeding events than did patients on warfarin monotherapy (95% confidence interval, 23.8%-28.3% vs. 95% CI, 18.3%-22.3%; P less than .001). Rates of observed thrombosis were similar between the two groups (95% CI, 1.6%-3.1% vs. 95% CI, 2.0%-3.6%; P = .40). This study demonstrates that aspirin use without a clinical indication remains common in patients taking warfarin for AFib or VTE, and that reducing inappropriate aspirin use in this patient population may help prevent adverse outcomes.
Bottom line: Use of aspirin without a clinical indication in patients taking warfarin is common and is associated with an increased risk of bleeding without significant clinical benefit.
Citation: Schaefer JK et al. Association of adding aspirin to warfarin therapy without an apparent indication with bleeding and other adverse events. JAMA Intern Med. 2019 Mar 4;179(4):533-41.
Dr. Wachter is an associate medical director at Duke Regional Hospital and an assistant professor of medicine at Duke University.
SECTION 4: HEALTHCARE SYSTEMS: SUPPORTING AND ADVANCING CHILD HEALTH
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 4: Healthcare Systems: Supporting and Advancing Child Health. J Hosp Med. 2020;15(S1):xxx-xxx (insert page numbers). https://doi.org/jhm.3400
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 4: Healthcare Systems: Supporting and Advancing Child Health. J Hosp Med. 2020;15(S1):xxx-xxx (insert page numbers). https://doi.org/jhm.3400
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 4: Healthcare Systems: Supporting and Advancing Child Health. J Hosp Med. 2020;15(S1):xxx-xxx (insert page numbers). https://doi.org/jhm.3400
SECTION 3: SPECIALIZED SERVICES
How to cite articles within Section 2
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 3: Specialized Services. J Hosp Med. 2020;15(S1):xx-xxx (insert page numbers). https://doi.org/10.12788/jhm.3399
How to cite articles within Section 2
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 3: Specialized Services. J Hosp Med. 2020;15(S1):xx-xxx (insert page numbers). https://doi.org/10.12788/jhm.3399
How to cite articles within Section 2
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 3: Specialized Services. J Hosp Med. 2020;15(S1):xx-xxx (insert page numbers). https://doi.org/10.12788/jhm.3399
SECTION 2: CORE SKILLS
How to cite articles within Section 2
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 2: Core Skills. J Hosp Med. 2020;15(S1):XX-XX (insert page numbers). https://doi.org/10.12788/jhm.3398
How to cite articles within Section 2
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 2: Core Skills. J Hosp Med. 2020;15(S1):XX-XX (insert page numbers). https://doi.org/10.12788/jhm.3398
How to cite articles within Section 2
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 2: Core Skills. J Hosp Med. 2020;15(S1):XX-XX (insert page numbers). https://doi.org/10.12788/jhm.3398
SECTION 1: COMMON CLINICAL DIAGNOSES AND CONDITIONS
How to cite articles within Section 1
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 1: Common Clinical Diagnoses and Conditions. J Hosp Med. 2020;15(S1):xx-xx (insert page numbers). https://doi.org/10.12788/jhm.3397
How to cite articles within Section 1
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 1: Common Clinical Diagnoses and Conditions. J Hosp Med. 2020;15(S1):xx-xx (insert page numbers). https://doi.org/10.12788/jhm.3397
How to cite articles within Section 1
Alvarez F, Alverson B, Balighian E, Beauchamp-Walters J, Biondi E, Blankenberg R, Bridgeman C, Brown J, Buchanan AO, Carlson D, Chang P, Coon E, Daud YN, Denniston S, DeWolfe CC, Deutsch SA, Doshi A, Fisher E, Gage S, Gallagher MP, Gill A, Goel Jones V, Grill J, Gupta A, Herbst BF Jr, Hershey D, Hoang K, Holmes AV, Hopkins A, Jones Y, Khan A, Lee V, Li ST, Lye, PS, Maginot T, Maloney C, Maniscalco J, Mannino Avila E, Markowsky A, Marks M, Matheny Antommaria AH, Maul E, McCulloh R, Melwani A, Miller C, Mittal V, Natt B, O'Toole J, Ottolini M, Percelay J, Phillips S, Pressel D, Quinonez R, Ralston S, Rappaport DI, Rauch D, Rhee K, Riese J, Roberts K, Rogers A, Rosenberg RE, Ruhlen M, Russell CJ, Russo C, Schwenk KM, Sekaran A, Shadman KA, Shah SS, Shen M, Simon T, Singh A, Smith K, Srinivas N Srivastava R, Sterni L, Thompson ED Jr, Thomson J, Tieder J, Tremoulet A, Wang ME, Williams R, Wu S. Name of Chapter. In: Pediatric Hospital Medicine Core Competencies: 2020 Revision. Section 1: Common Clinical Diagnoses and Conditions. J Hosp Med. 2020;15(S1):xx-xx (insert page numbers). https://doi.org/10.12788/jhm.3397