User login
Leadership & Professional Development: Make a Friend Before You Need One
“Takers believe in a zero-sum world, and they end up creating one where bosses, colleagues and clients don’t trust them. Givers build deeper and broader relationships—people are rooting for them instead of gunning for them.”
—Adam Grant
To succeed in a hospital, leaders need a generous supply of social and political capital. House officers learn this very quickly, especially when they are relying on other members of the healthcare team to obtain tests and studies for their patients and calling for specialty consultations. To be successful and efficient, building relationships and trust is key. Such capital, unfortunately, takes time to develop. Therefore, healthcare leaders and clinicians at all levels of training need to make an everyday investment of goodwill and friendliness with those they encounter. The dividends may be slow in coming, but they are substantial and sustained. Friends give you the benefit of the doubt—and help you when you are most in need.
Having friends (or friendly colleagues) at work is beneficial both professionally and personally. The benefits of social interactions have been studied for years and even more so in recent times with the dramatic increase in the use of handheld devices. Eye contact between casual acquaintances passing each other in the hallway is replaced with eyes focused downward on smartphones. The result? We are becoming more socially isolated. Our personal solution? When we see professional colleagues (or patients and families in the hallways of our hospital), we nod in acknowledgement with appropriate eye contact and say “Good morning” or “Hello” even if we don’t know them—even if their eyes are focused on their devices as they walk past you in the hallway. You get a gold star if you remember the names of the professional colleagues you see frequently in the hallways or around the hospital.
This isn’t soft science; it’s backed by hard data. When we conduct site visits of different hospitals around the country to help them improve their care quality and performance, we informally divide hospitals into two groups: The “How ya doin’?” hospitals vs the “Rec-Ignore” hospitals (in which employees recognize a colleague in the hallway but choose to not acknowledge them). Most prefer to work at a “How ya doin’?” hospital. Being friendly has been linked to increased team spirit and morale, knowledge sharing, trust, prevention of burnout, and sense of a positive working environment. It also makes you feel better about yourself—and makes other people feel similarly as well.
We’ll share an example from a search for a new department chair. The dean went on reverse site visits to meet the two finalists in their home institutions and asked them for tours of their hospitals. Candidate A walked around and it seemed like everyone knew her. She smiled and said hello to the people she came in contact with during the tour. Not so for candidate B—just the opposite. Guess which candidate the dean hired?
Put away your phone, interact with your colleagues, and learn to make small talk, and not just with your supervisors or peers. Chitchat is an important “social lubricant,” fostering a sense of community and teamwork. It helps bring down the divides that come from organizational hierarchies. It helps endear you to your staff.
Developing a reputation as a nice person who is quick with a smile and even quicker with a “How ya doin’?” pays off in the end. This reputation also makes it easier to give bad news, something that all leaders must do at some point. So make a friend before you need one—it usually will pay dividends.
“Takers believe in a zero-sum world, and they end up creating one where bosses, colleagues and clients don’t trust them. Givers build deeper and broader relationships—people are rooting for them instead of gunning for them.”
—Adam Grant
To succeed in a hospital, leaders need a generous supply of social and political capital. House officers learn this very quickly, especially when they are relying on other members of the healthcare team to obtain tests and studies for their patients and calling for specialty consultations. To be successful and efficient, building relationships and trust is key. Such capital, unfortunately, takes time to develop. Therefore, healthcare leaders and clinicians at all levels of training need to make an everyday investment of goodwill and friendliness with those they encounter. The dividends may be slow in coming, but they are substantial and sustained. Friends give you the benefit of the doubt—and help you when you are most in need.
Having friends (or friendly colleagues) at work is beneficial both professionally and personally. The benefits of social interactions have been studied for years and even more so in recent times with the dramatic increase in the use of handheld devices. Eye contact between casual acquaintances passing each other in the hallway is replaced with eyes focused downward on smartphones. The result? We are becoming more socially isolated. Our personal solution? When we see professional colleagues (or patients and families in the hallways of our hospital), we nod in acknowledgement with appropriate eye contact and say “Good morning” or “Hello” even if we don’t know them—even if their eyes are focused on their devices as they walk past you in the hallway. You get a gold star if you remember the names of the professional colleagues you see frequently in the hallways or around the hospital.
This isn’t soft science; it’s backed by hard data. When we conduct site visits of different hospitals around the country to help them improve their care quality and performance, we informally divide hospitals into two groups: The “How ya doin’?” hospitals vs the “Rec-Ignore” hospitals (in which employees recognize a colleague in the hallway but choose to not acknowledge them). Most prefer to work at a “How ya doin’?” hospital. Being friendly has been linked to increased team spirit and morale, knowledge sharing, trust, prevention of burnout, and sense of a positive working environment. It also makes you feel better about yourself—and makes other people feel similarly as well.
We’ll share an example from a search for a new department chair. The dean went on reverse site visits to meet the two finalists in their home institutions and asked them for tours of their hospitals. Candidate A walked around and it seemed like everyone knew her. She smiled and said hello to the people she came in contact with during the tour. Not so for candidate B—just the opposite. Guess which candidate the dean hired?
Put away your phone, interact with your colleagues, and learn to make small talk, and not just with your supervisors or peers. Chitchat is an important “social lubricant,” fostering a sense of community and teamwork. It helps bring down the divides that come from organizational hierarchies. It helps endear you to your staff.
Developing a reputation as a nice person who is quick with a smile and even quicker with a “How ya doin’?” pays off in the end. This reputation also makes it easier to give bad news, something that all leaders must do at some point. So make a friend before you need one—it usually will pay dividends.
“Takers believe in a zero-sum world, and they end up creating one where bosses, colleagues and clients don’t trust them. Givers build deeper and broader relationships—people are rooting for them instead of gunning for them.”
—Adam Grant
To succeed in a hospital, leaders need a generous supply of social and political capital. House officers learn this very quickly, especially when they are relying on other members of the healthcare team to obtain tests and studies for their patients and calling for specialty consultations. To be successful and efficient, building relationships and trust is key. Such capital, unfortunately, takes time to develop. Therefore, healthcare leaders and clinicians at all levels of training need to make an everyday investment of goodwill and friendliness with those they encounter. The dividends may be slow in coming, but they are substantial and sustained. Friends give you the benefit of the doubt—and help you when you are most in need.
Having friends (or friendly colleagues) at work is beneficial both professionally and personally. The benefits of social interactions have been studied for years and even more so in recent times with the dramatic increase in the use of handheld devices. Eye contact between casual acquaintances passing each other in the hallway is replaced with eyes focused downward on smartphones. The result? We are becoming more socially isolated. Our personal solution? When we see professional colleagues (or patients and families in the hallways of our hospital), we nod in acknowledgement with appropriate eye contact and say “Good morning” or “Hello” even if we don’t know them—even if their eyes are focused on their devices as they walk past you in the hallway. You get a gold star if you remember the names of the professional colleagues you see frequently in the hallways or around the hospital.
This isn’t soft science; it’s backed by hard data. When we conduct site visits of different hospitals around the country to help them improve their care quality and performance, we informally divide hospitals into two groups: The “How ya doin’?” hospitals vs the “Rec-Ignore” hospitals (in which employees recognize a colleague in the hallway but choose to not acknowledge them). Most prefer to work at a “How ya doin’?” hospital. Being friendly has been linked to increased team spirit and morale, knowledge sharing, trust, prevention of burnout, and sense of a positive working environment. It also makes you feel better about yourself—and makes other people feel similarly as well.
We’ll share an example from a search for a new department chair. The dean went on reverse site visits to meet the two finalists in their home institutions and asked them for tours of their hospitals. Candidate A walked around and it seemed like everyone knew her. She smiled and said hello to the people she came in contact with during the tour. Not so for candidate B—just the opposite. Guess which candidate the dean hired?
Put away your phone, interact with your colleagues, and learn to make small talk, and not just with your supervisors or peers. Chitchat is an important “social lubricant,” fostering a sense of community and teamwork. It helps bring down the divides that come from organizational hierarchies. It helps endear you to your staff.
Developing a reputation as a nice person who is quick with a smile and even quicker with a “How ya doin’?” pays off in the end. This reputation also makes it easier to give bad news, something that all leaders must do at some point. So make a friend before you need one—it usually will pay dividends.
Yale’s COVID-19 inpatient protocol: Hydroxychloroquine plus/minus tocilizumab
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
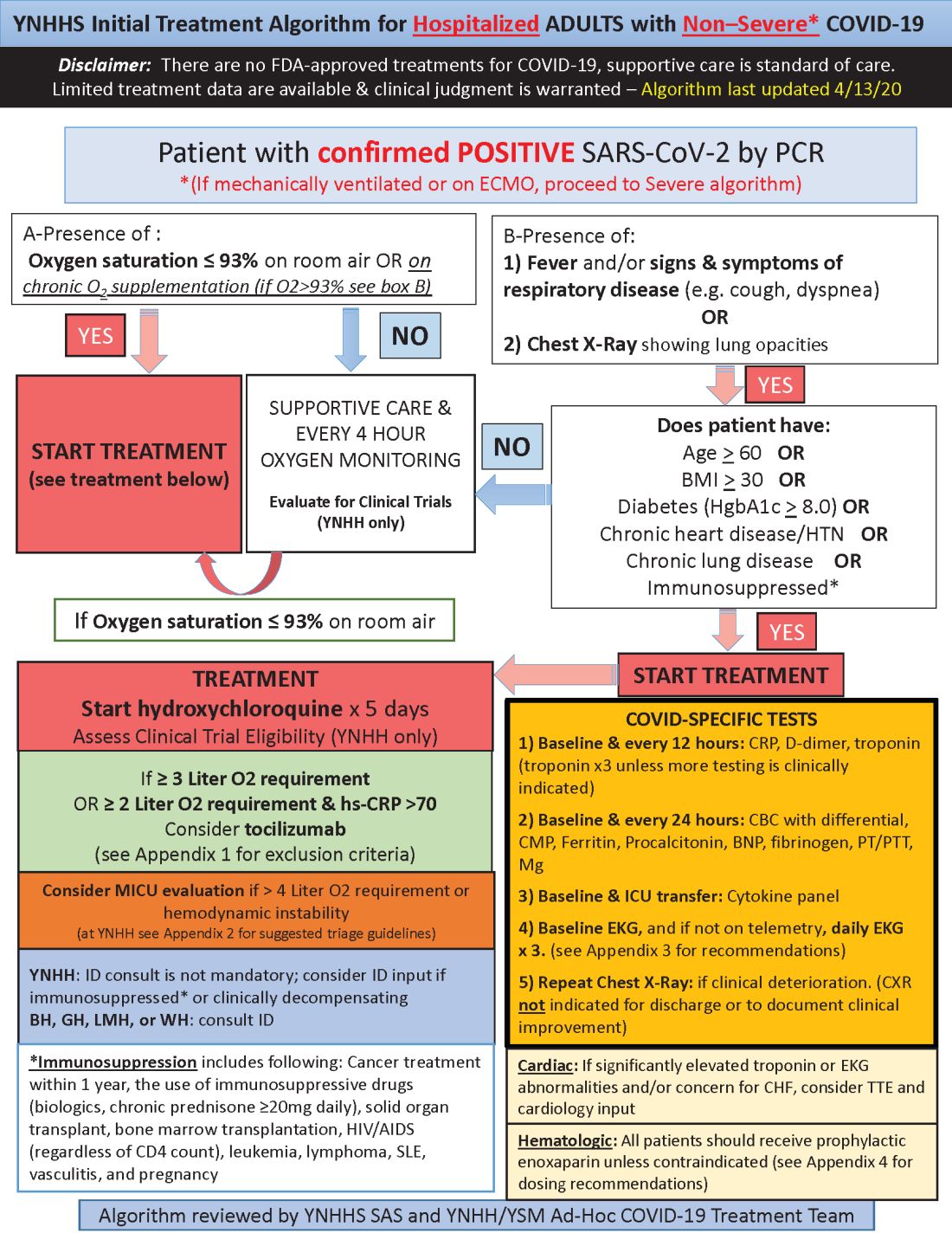
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
aotto@mdedge.com
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
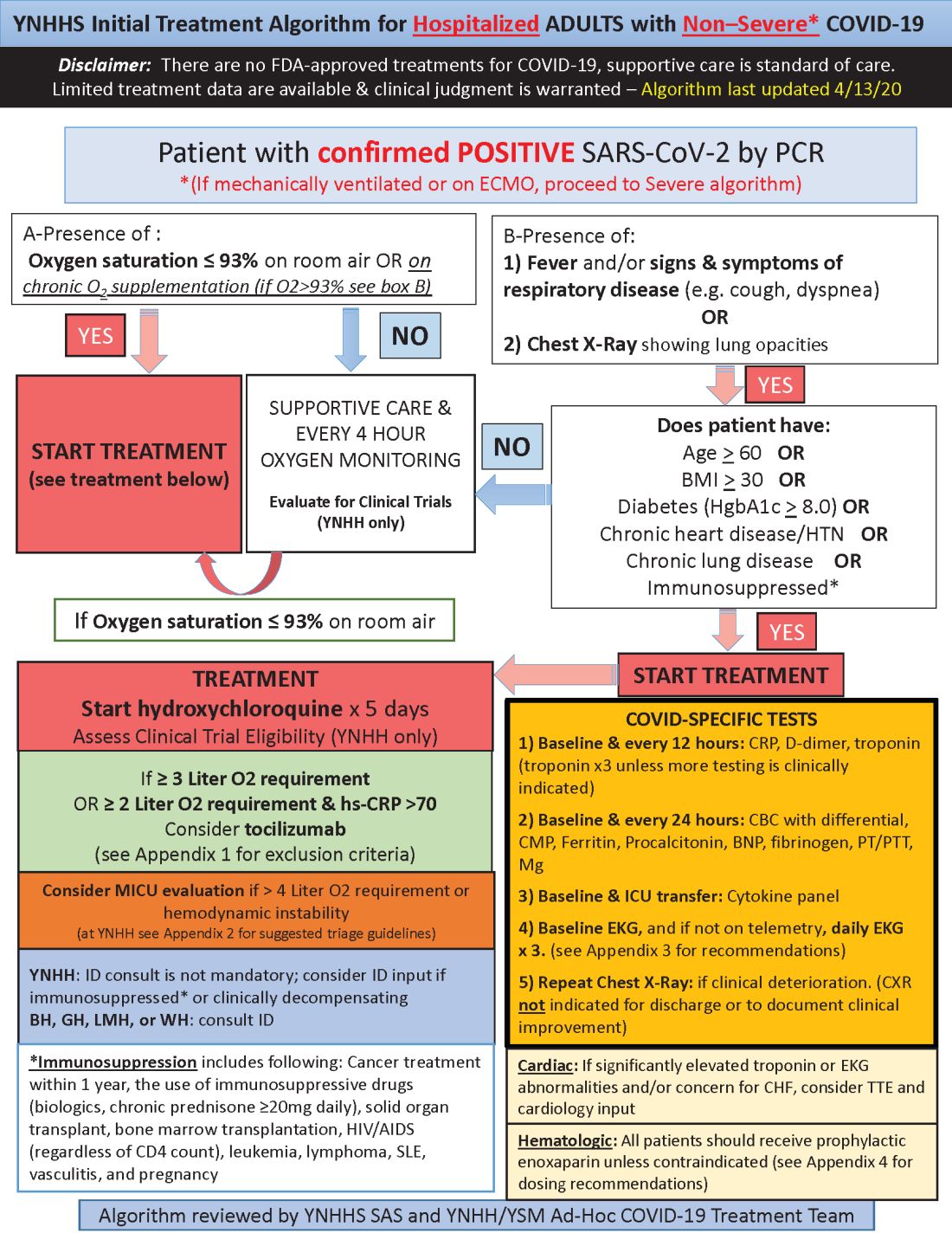
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
aotto@mdedge.com
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
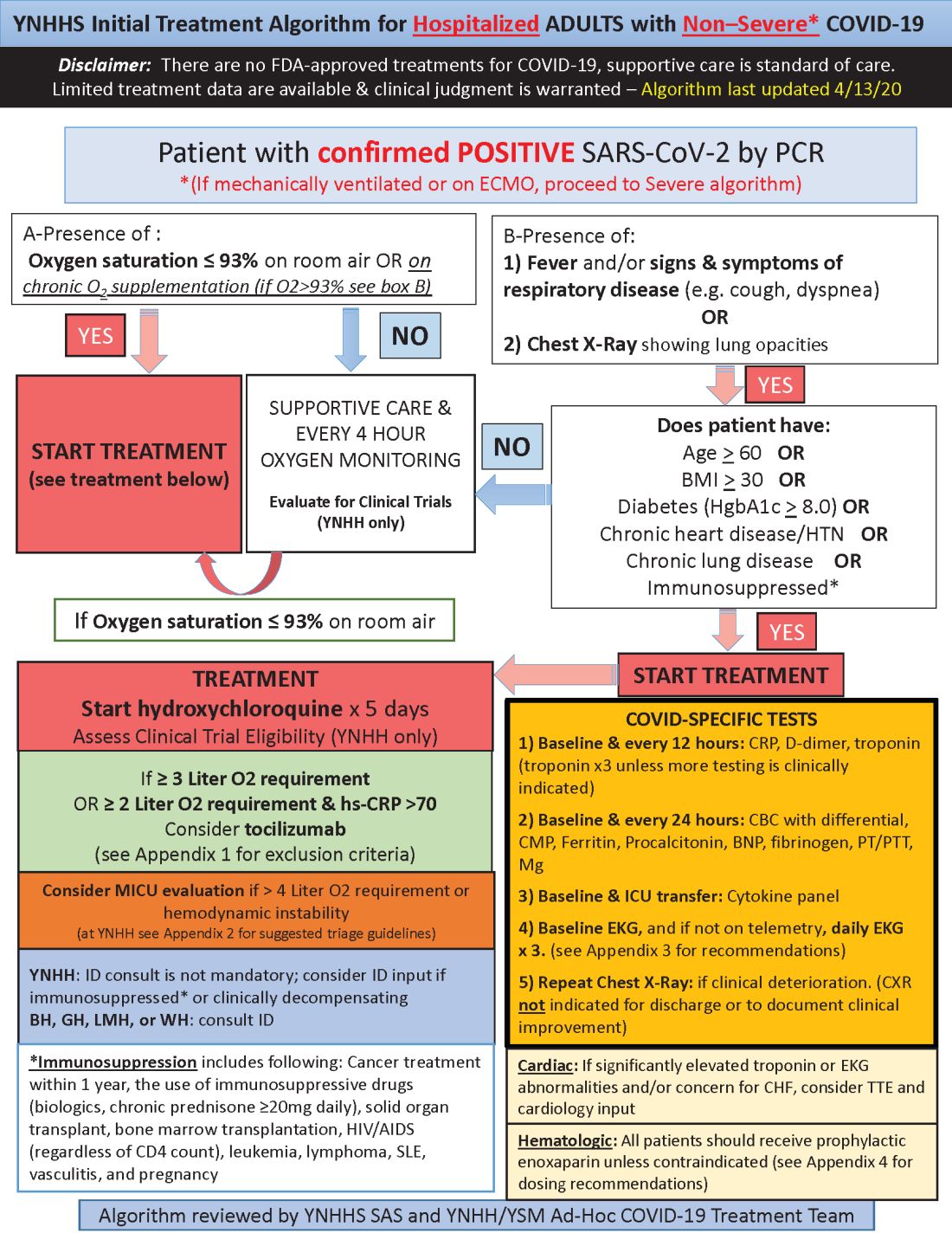
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
aotto@mdedge.com
This article was updated with the latest treatment algorithm on 5/6/2020.
POPCoRN network mobilizes pediatric capacity during pandemic
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
Med-Peds hospitalists were an organizing force
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
Prior head injury is associated with severe Parkinson’s disease phenotype
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Neurologists have identified various phenotypes among patients with Parkinson’s disease; however, the factors that determine these phenotypes, which may include genetic and environmental variables, are poorly understood. Ethan G. Brown, MD, assistant professor of neurology at the University of California, San Francisco, and colleagues hypothesized that head injury, which is a risk factor for Parkinson’s disease, would be associated with a more severe phenotype.
“Head injury is a risk factor for other conditions that involve cognitive impairment,” said Dr. Brown. “The mechanisms of how head injury contributes to neurodegenerative disease are not clear, but may be related to the initiation of an inflammatory cascade that can have a long-term, chronic effect. We hypothesized that these long-term sequelae may contribute to symptoms in Parkinson’s disease.”
An analysis of data from two cohorts
The researchers examined the relationship between head injury and clinical features by analyzing data for two cohorts of patients with Parkinson’s disease. Through an online survey, the investigators elicited information about head injury and other exposures from participants in the Parkinson’s Progression Markers Initiative (PPMI) and the Fox Insight (FI) study. Dr. Brown and colleagues determined disease phenotypes for participants in PPMI using baseline Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) score and 5-year change in Montreal Cognitive Assessment score. For participants in FI, the researchers determined phenotypes using baseline self-reported MDS-UPDRS-II score and self-reported cognitive impairment. They used parametric and nonparametric tests as appropriate and adjusted the results for age, sex, and smoking history.
In all, 267 participants with Parkinson’s disease in PPMI and 25,308 in FI submitted information about head injury. In the PPMI cohort, head injury before Parkinson’s disease diagnosis was associated with greater nonmotor symptom burden at enrollment. The mean MDS-UPDRS-I score was 7.73 among participants with any injury, compared with 6.19 among participants with no injury. Similarly, the mean MDS-UPDRS-I score was 8.29 among participants with severe head injury, compared with 6.19 among participants with no injury. Motor symptoms were worse among participants with severe injury (MDS-UPDRS-II score, 8.35). Among 110 participants who were followed for 5 years, patients who reported severe head injury before diagnosis had a decline in cognitive function. The mean change in Montreal Cognitive Assessment score was –0.60 for patients with severe head injury and 0.76 in those with no head injury.
“The improvement from baseline in the participants with Parkinson’s disease but without head injury was small and not statistically significant,” said Dr. Brown. The increase could have resulted from practice effect, although it is not certain, he added. “We are continuing to evaluate other, more sensitive tests of cognitive impairment to try to understand these results more completely in this population.”
In the FI cohort, participants who reported a prior head injury had more motor symptoms (MDS-UPDRS-II, 14.4), compared with those without head injury (MDS-UPDRS-II, 12.1). Also, the risk of self-reported cognitive impairment was elevated in participants who reported head injury (odds ratio, 1.58).
“The results most affected by the self-reported nature of [the] FI [data] are the cognitive impairment results,” said Dr. Brown. “Subjective cognitive impairment ... is very different from objective cognitive impairment, which could be measured through in-person testing in the PPMI cohort. Many factors may contribute to noticing cognitive decline, some of which can be measured and controlled for, but some cannot. There may be a correlation between subjective cognitive decline and true cognitive impairment, but this has not been fully studied in Parkinson’s disease.”
The search for the underlying mechanism
Clarifying whether the relationship between head injury and Parkinson’s disease phenotype is causal or whether falling is an early indication of worse symptoms will require more longitudinal data. “We would like to further characterize the differences between people with Parkinson’s disease with and without a history of head injury,” said Dr. Brown. “More detailed understanding of these phenotypic differences could point to an underlying mechanism, or whether or not other comorbid conditions are involved. We would also like to understand whether genetics plays a role.”
The PPMI and FI studies are funded by the Michael J. Fox Foundation. Dr. Brown has received compensation from HiOscar, NEJM Knowledge Plus, and Rune Labs and has received research support from Gateway Institute for Brain Research.
SOURCE: Brown EG et al. AAN 2020, Abstract S17.002.
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Neurologists have identified various phenotypes among patients with Parkinson’s disease; however, the factors that determine these phenotypes, which may include genetic and environmental variables, are poorly understood. Ethan G. Brown, MD, assistant professor of neurology at the University of California, San Francisco, and colleagues hypothesized that head injury, which is a risk factor for Parkinson’s disease, would be associated with a more severe phenotype.
“Head injury is a risk factor for other conditions that involve cognitive impairment,” said Dr. Brown. “The mechanisms of how head injury contributes to neurodegenerative disease are not clear, but may be related to the initiation of an inflammatory cascade that can have a long-term, chronic effect. We hypothesized that these long-term sequelae may contribute to symptoms in Parkinson’s disease.”
An analysis of data from two cohorts
The researchers examined the relationship between head injury and clinical features by analyzing data for two cohorts of patients with Parkinson’s disease. Through an online survey, the investigators elicited information about head injury and other exposures from participants in the Parkinson’s Progression Markers Initiative (PPMI) and the Fox Insight (FI) study. Dr. Brown and colleagues determined disease phenotypes for participants in PPMI using baseline Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) score and 5-year change in Montreal Cognitive Assessment score. For participants in FI, the researchers determined phenotypes using baseline self-reported MDS-UPDRS-II score and self-reported cognitive impairment. They used parametric and nonparametric tests as appropriate and adjusted the results for age, sex, and smoking history.
In all, 267 participants with Parkinson’s disease in PPMI and 25,308 in FI submitted information about head injury. In the PPMI cohort, head injury before Parkinson’s disease diagnosis was associated with greater nonmotor symptom burden at enrollment. The mean MDS-UPDRS-I score was 7.73 among participants with any injury, compared with 6.19 among participants with no injury. Similarly, the mean MDS-UPDRS-I score was 8.29 among participants with severe head injury, compared with 6.19 among participants with no injury. Motor symptoms were worse among participants with severe injury (MDS-UPDRS-II score, 8.35). Among 110 participants who were followed for 5 years, patients who reported severe head injury before diagnosis had a decline in cognitive function. The mean change in Montreal Cognitive Assessment score was –0.60 for patients with severe head injury and 0.76 in those with no head injury.
“The improvement from baseline in the participants with Parkinson’s disease but without head injury was small and not statistically significant,” said Dr. Brown. The increase could have resulted from practice effect, although it is not certain, he added. “We are continuing to evaluate other, more sensitive tests of cognitive impairment to try to understand these results more completely in this population.”
In the FI cohort, participants who reported a prior head injury had more motor symptoms (MDS-UPDRS-II, 14.4), compared with those without head injury (MDS-UPDRS-II, 12.1). Also, the risk of self-reported cognitive impairment was elevated in participants who reported head injury (odds ratio, 1.58).
“The results most affected by the self-reported nature of [the] FI [data] are the cognitive impairment results,” said Dr. Brown. “Subjective cognitive impairment ... is very different from objective cognitive impairment, which could be measured through in-person testing in the PPMI cohort. Many factors may contribute to noticing cognitive decline, some of which can be measured and controlled for, but some cannot. There may be a correlation between subjective cognitive decline and true cognitive impairment, but this has not been fully studied in Parkinson’s disease.”
The search for the underlying mechanism
Clarifying whether the relationship between head injury and Parkinson’s disease phenotype is causal or whether falling is an early indication of worse symptoms will require more longitudinal data. “We would like to further characterize the differences between people with Parkinson’s disease with and without a history of head injury,” said Dr. Brown. “More detailed understanding of these phenotypic differences could point to an underlying mechanism, or whether or not other comorbid conditions are involved. We would also like to understand whether genetics plays a role.”
The PPMI and FI studies are funded by the Michael J. Fox Foundation. Dr. Brown has received compensation from HiOscar, NEJM Knowledge Plus, and Rune Labs and has received research support from Gateway Institute for Brain Research.
SOURCE: Brown EG et al. AAN 2020, Abstract S17.002.
according to research presented online as part of the 2020 American Academy of Neurology Science Highlights.
Neurologists have identified various phenotypes among patients with Parkinson’s disease; however, the factors that determine these phenotypes, which may include genetic and environmental variables, are poorly understood. Ethan G. Brown, MD, assistant professor of neurology at the University of California, San Francisco, and colleagues hypothesized that head injury, which is a risk factor for Parkinson’s disease, would be associated with a more severe phenotype.
“Head injury is a risk factor for other conditions that involve cognitive impairment,” said Dr. Brown. “The mechanisms of how head injury contributes to neurodegenerative disease are not clear, but may be related to the initiation of an inflammatory cascade that can have a long-term, chronic effect. We hypothesized that these long-term sequelae may contribute to symptoms in Parkinson’s disease.”
An analysis of data from two cohorts
The researchers examined the relationship between head injury and clinical features by analyzing data for two cohorts of patients with Parkinson’s disease. Through an online survey, the investigators elicited information about head injury and other exposures from participants in the Parkinson’s Progression Markers Initiative (PPMI) and the Fox Insight (FI) study. Dr. Brown and colleagues determined disease phenotypes for participants in PPMI using baseline Movement Disorder Society-Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) score and 5-year change in Montreal Cognitive Assessment score. For participants in FI, the researchers determined phenotypes using baseline self-reported MDS-UPDRS-II score and self-reported cognitive impairment. They used parametric and nonparametric tests as appropriate and adjusted the results for age, sex, and smoking history.
In all, 267 participants with Parkinson’s disease in PPMI and 25,308 in FI submitted information about head injury. In the PPMI cohort, head injury before Parkinson’s disease diagnosis was associated with greater nonmotor symptom burden at enrollment. The mean MDS-UPDRS-I score was 7.73 among participants with any injury, compared with 6.19 among participants with no injury. Similarly, the mean MDS-UPDRS-I score was 8.29 among participants with severe head injury, compared with 6.19 among participants with no injury. Motor symptoms were worse among participants with severe injury (MDS-UPDRS-II score, 8.35). Among 110 participants who were followed for 5 years, patients who reported severe head injury before diagnosis had a decline in cognitive function. The mean change in Montreal Cognitive Assessment score was –0.60 for patients with severe head injury and 0.76 in those with no head injury.
“The improvement from baseline in the participants with Parkinson’s disease but without head injury was small and not statistically significant,” said Dr. Brown. The increase could have resulted from practice effect, although it is not certain, he added. “We are continuing to evaluate other, more sensitive tests of cognitive impairment to try to understand these results more completely in this population.”
In the FI cohort, participants who reported a prior head injury had more motor symptoms (MDS-UPDRS-II, 14.4), compared with those without head injury (MDS-UPDRS-II, 12.1). Also, the risk of self-reported cognitive impairment was elevated in participants who reported head injury (odds ratio, 1.58).
“The results most affected by the self-reported nature of [the] FI [data] are the cognitive impairment results,” said Dr. Brown. “Subjective cognitive impairment ... is very different from objective cognitive impairment, which could be measured through in-person testing in the PPMI cohort. Many factors may contribute to noticing cognitive decline, some of which can be measured and controlled for, but some cannot. There may be a correlation between subjective cognitive decline and true cognitive impairment, but this has not been fully studied in Parkinson’s disease.”
The search for the underlying mechanism
Clarifying whether the relationship between head injury and Parkinson’s disease phenotype is causal or whether falling is an early indication of worse symptoms will require more longitudinal data. “We would like to further characterize the differences between people with Parkinson’s disease with and without a history of head injury,” said Dr. Brown. “More detailed understanding of these phenotypic differences could point to an underlying mechanism, or whether or not other comorbid conditions are involved. We would also like to understand whether genetics plays a role.”
The PPMI and FI studies are funded by the Michael J. Fox Foundation. Dr. Brown has received compensation from HiOscar, NEJM Knowledge Plus, and Rune Labs and has received research support from Gateway Institute for Brain Research.
SOURCE: Brown EG et al. AAN 2020, Abstract S17.002.
FROM AAN 2020
Predictors of ICH after thrombectomy identified
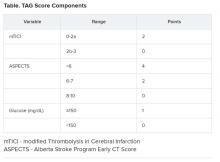
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
(ICH), new research suggests. In a study of nearly 600 patients undergoing thrombectomy, investigators combined a modified Thrombolysis in Cerebral Ischemia (TICI) score, an Alberta Stroke Program Early Computed Tomography Score (ASPECTS), and glucose levels (the “TAG score”) to predict risk. Results showed that each unit increase in the combination score was associated with a significant, nearly twofold greater likelihood of symptomatic ICH.
“It is very easy” to calculate the new score in a clinical setting, lead author Mayra Johana Montalvo Perero, MD, Department of Neurology, Brown University and Rhode Island Hospital, Providence, said. “You just need three variables.”
The findings were presented online as part of the 2020 American Academy of Neurology Science Highlights.
Limited data
High TAG scores are associated with symptomatic ICH in patients receiving mechanical thrombectomy, Dr. Montalvo Perero and colleagues said.
Although clinical predictors of symptomatic ICH are well established, “there is limited data in patients who underwent mechanical thrombectomy,” the researchers noted.
To learn more, they assessed 578 patients (52% women; mean age, 73 years) who had mechanical thrombectomy for acute ischemic stroke at a comprehensive stroke center. Within this cohort, 19 patients (3.3%) developed symptomatic ICH.
The investigators compared clinical and radiographic findings between patients who experienced symptomatic ICH and those who did not.
The TICI score emerged as a predictor when each unit decrease in this score was associated with greater risk for symptomatic ICH (odds ratio, 5.13; 95% confidence interval, 1.84-14.29; P = .002).
Each one-point decrease in the ASPECTS score also predicted increased risk (OR, 1.52; 95% CI, 1.1-2.0; P = .003).
“The main driver is the size of the stroke core, which is correlated with the ASPECTS score,” Dr. Montalvo Perero said.
Each 10 mg/dL increase in glucose level also correlated with increased risk (OR, 1.07; 95% CI, 1.01-1.13; P = .018).
Twice the risk
The investigators then combined these three independent variables into a weighted TAG score based on a multivariate analysis. Each unit increase in this composite score was associated with increased risk of symptomatic ICH (OR, 1.98; 95% CI, 1.48-2.66; P < .001).
There was no association between patients who received tissue plasminogen activator (tPA) and risk of symptomatic ICH, which Dr. Montalvo Perero said was surprising.
However, “that may be due to a small number” of patients with symptomatic ICH included in the study, she said. “Therefore, that would be an interesting question to ask in future studies with bigger cohorts.”
Larger studies are also needed to validate this scoring system and to test strategies to reduce risk of symptomatic ICH and make thrombectomy safer in patients with elevated TAG scores, Dr. Montalvo Perero said.
A step in the right direction?
Commenting on the study, Jeremy Payne, MD, PhD, director of the Stroke Center at Banner Health’s University Medicine Neuroscience Institute in Phoenix, Arizona, noted the importance of predicting which patients might have secondary bleeding after interventional treatment of a large vessel occlusion stroke
“In aggregate, the role of endovascular thrombectomy is quite clear, but we still struggle to predict at the individual patient level who will benefit,” said Dr. Payne, who was not involved with the research.
Transfer and treatment of these patients also carries an economic cost. “Just getting patients to our center, where about 80% of the complex stroke patients come by helicopter, costs upwards of $30,000,” Dr. Payne said. “The financial argument isn’t one we like to talk much about, but we’re committing to spending probably $100,000-$200,000 on each person’s care.”
This study “attempts to address an important issue,” he said.
Predicting who is more likely to benefit leads to the assumption that if that were to happen, “we could skip all the rigamarole of helicopters and procedures, avoid the extra expense and particularly not make things worse than they already are,” explained Dr. Payne.
Potential limitations include that this is a single-center study and is based on an analysis of 19 patients out of 578. As a result, it is not clear that these findings will necessarily be generalizable to other centers, said Dr. Payne.
The TICI and ASPECTS “are pretty obvious markers of risk,” he noted. “The glucose levels, however, are more subtly interesting.”
He also pointed out that an association between diabetes and worse stroke outcomes is well established.
“The mechanisms are poorly understood, but the role of glucose keeps popping up as a potential marker of risk, and so it’s interesting that it bubbles up in their work too,” Dr. Payne said.
Furthermore, unlike TICI and ASPECTS, glucose levels are modifiable.
“Overall, then, we will continue to study this,” Dr. Payne said. “It’s very important to refine our ability to predict which patients may receive benefit versus harm from such procedures, and this is a step in the right direction.”
Some findings were also published December 2019 in the Journal of Neurology, Neurosurgery & Psychiatry.
Montalvo Perero and Payne have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
SOURCE: Motalvo Perero MJ et al. AAN 2020, Abstract S20.001.
AAN 2020
AAP releases updated guidance on male teen sexual, reproductive health
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
FROM PEDIATRICS
IDSA guidelines cover N95 use and reuse
The Infectious Disease Society of America has released new guidelines on the use and reuse of personal protective equipment, most of which address the use of face protection, for health care workers caring for COVID-19 patients. In releasing the guidelines, the IDSA expert guideline panel acknowledged gaps in evidence to support the recommendations, which is why they will be updated regularly as new evidence emerges.
“Our real goal here is to update these guidelines as a live document,” panel chair John Lynch III, MD, MPH, of the University of Washington, Seattle, said in a press briefing. “Looking at whatever research is coming out where it gets to the point where we find that the evidence is strong enough to make a change, I think we’ll need to readdress these recommendations.”
The panel tailored recommendations to the availability of supplies: conventional capacity for usual supplies; contingency capacity, when supplies are conserved, adapted and substituted with occasional reuse of select supplies; and crisis capacity, when critical supplies are lacking.
The guidelines contain the following eight recommendations for encounters with suspected or confirmed COVID-19 patients:
1) Either a surgical mask or N95 (or N99 or PAPR [powered & supplied air respiratory protection]) respirator for routine patient care in a conventional setting.
2) Either a surgical mask or reprocessed respirator as opposed to no mask for routine care in a contingency or crisis setting.
3) No recommendation on the use of double gloves vs. single gloves.
4) No recommendation on the use of shoe covers for any setting.
5) An N95 (or N99 or PAPR) respirator for aerosol-generating procedures in a conventional setting.
6) A reprocessed N95 respirator as opposed to a surgical mask for aerosol-generating procedures in a contingency or crisis setting.
7) Adding a face shield or surgical mask as a cover for an N95 respirator to allow for extended use during respirator shortages when performing aerosol-generating procedures in a contingency or crisis setting. This recommendation carries a caveat: It assumes correct doffing sequence and hand hygiene before and after taking off the face shield or surgical mask cover.
8) In the same scenario, adding a face shield or surgical mask over the N95 respirator so it can be reused, again assuming the correct sequence for hand hygiene.
The guideline was developed using the GRADE approach – for Grading of Recommendations Assessment, Development, and Evaluation – and a modified methodology for developing rapid recommendations. The levels of evidence supporting each recommendation vary from moderate for the first two to knowledge gap for the third and fourth to very low certainty for the last four.
“You can see that the eight recommendations that were made, a large part of them are really focused on masks, but there are a huge number of other disparate questions that need to be answered where there is really no good evidence basis,” Dr. Lynch said. “If we see any new evidence around that, we can at least provide commentary but I would really hope evidence-based recommendations around some of those interventions.”
Panel member Allison McGeer, MD, FRCPC, of the University of Toronto, explained the lack of evidence supporting infection prevention in hospitals. “In medicine we tend to look at individual patterns and individual patient outcomes,” she said. “When you’re looking at infection prevention, you’re looking at health systems and their outcomes, and it’s much harder to randomize hospitals or a state or a country to one particular policy about how to protect patients from infections in hospitals.”
The latest guidelines follow IDSA’s previously released guidelines on treatment and management of COVID-19 patients. The panel also plans to release guidelines on use of diagnostics for COVID-19 care.
Dr. Lynch has no financial relationships to disclose. Dr. McGeer disclosed relationships with Pfizer, Merck, Sanofi Pasteur, Seqirus, GlaxoSmithKline and Cidara.
SOURCE: Lynch JB et al. IDSA. April 27, 2020.
The Infectious Disease Society of America has released new guidelines on the use and reuse of personal protective equipment, most of which address the use of face protection, for health care workers caring for COVID-19 patients. In releasing the guidelines, the IDSA expert guideline panel acknowledged gaps in evidence to support the recommendations, which is why they will be updated regularly as new evidence emerges.
“Our real goal here is to update these guidelines as a live document,” panel chair John Lynch III, MD, MPH, of the University of Washington, Seattle, said in a press briefing. “Looking at whatever research is coming out where it gets to the point where we find that the evidence is strong enough to make a change, I think we’ll need to readdress these recommendations.”
The panel tailored recommendations to the availability of supplies: conventional capacity for usual supplies; contingency capacity, when supplies are conserved, adapted and substituted with occasional reuse of select supplies; and crisis capacity, when critical supplies are lacking.
The guidelines contain the following eight recommendations for encounters with suspected or confirmed COVID-19 patients:
1) Either a surgical mask or N95 (or N99 or PAPR [powered & supplied air respiratory protection]) respirator for routine patient care in a conventional setting.
2) Either a surgical mask or reprocessed respirator as opposed to no mask for routine care in a contingency or crisis setting.
3) No recommendation on the use of double gloves vs. single gloves.
4) No recommendation on the use of shoe covers for any setting.
5) An N95 (or N99 or PAPR) respirator for aerosol-generating procedures in a conventional setting.
6) A reprocessed N95 respirator as opposed to a surgical mask for aerosol-generating procedures in a contingency or crisis setting.
7) Adding a face shield or surgical mask as a cover for an N95 respirator to allow for extended use during respirator shortages when performing aerosol-generating procedures in a contingency or crisis setting. This recommendation carries a caveat: It assumes correct doffing sequence and hand hygiene before and after taking off the face shield or surgical mask cover.
8) In the same scenario, adding a face shield or surgical mask over the N95 respirator so it can be reused, again assuming the correct sequence for hand hygiene.
The guideline was developed using the GRADE approach – for Grading of Recommendations Assessment, Development, and Evaluation – and a modified methodology for developing rapid recommendations. The levels of evidence supporting each recommendation vary from moderate for the first two to knowledge gap for the third and fourth to very low certainty for the last four.
“You can see that the eight recommendations that were made, a large part of them are really focused on masks, but there are a huge number of other disparate questions that need to be answered where there is really no good evidence basis,” Dr. Lynch said. “If we see any new evidence around that, we can at least provide commentary but I would really hope evidence-based recommendations around some of those interventions.”
Panel member Allison McGeer, MD, FRCPC, of the University of Toronto, explained the lack of evidence supporting infection prevention in hospitals. “In medicine we tend to look at individual patterns and individual patient outcomes,” she said. “When you’re looking at infection prevention, you’re looking at health systems and their outcomes, and it’s much harder to randomize hospitals or a state or a country to one particular policy about how to protect patients from infections in hospitals.”
The latest guidelines follow IDSA’s previously released guidelines on treatment and management of COVID-19 patients. The panel also plans to release guidelines on use of diagnostics for COVID-19 care.
Dr. Lynch has no financial relationships to disclose. Dr. McGeer disclosed relationships with Pfizer, Merck, Sanofi Pasteur, Seqirus, GlaxoSmithKline and Cidara.
SOURCE: Lynch JB et al. IDSA. April 27, 2020.
The Infectious Disease Society of America has released new guidelines on the use and reuse of personal protective equipment, most of which address the use of face protection, for health care workers caring for COVID-19 patients. In releasing the guidelines, the IDSA expert guideline panel acknowledged gaps in evidence to support the recommendations, which is why they will be updated regularly as new evidence emerges.
“Our real goal here is to update these guidelines as a live document,” panel chair John Lynch III, MD, MPH, of the University of Washington, Seattle, said in a press briefing. “Looking at whatever research is coming out where it gets to the point where we find that the evidence is strong enough to make a change, I think we’ll need to readdress these recommendations.”
The panel tailored recommendations to the availability of supplies: conventional capacity for usual supplies; contingency capacity, when supplies are conserved, adapted and substituted with occasional reuse of select supplies; and crisis capacity, when critical supplies are lacking.
The guidelines contain the following eight recommendations for encounters with suspected or confirmed COVID-19 patients:
1) Either a surgical mask or N95 (or N99 or PAPR [powered & supplied air respiratory protection]) respirator for routine patient care in a conventional setting.
2) Either a surgical mask or reprocessed respirator as opposed to no mask for routine care in a contingency or crisis setting.
3) No recommendation on the use of double gloves vs. single gloves.
4) No recommendation on the use of shoe covers for any setting.
5) An N95 (or N99 or PAPR) respirator for aerosol-generating procedures in a conventional setting.
6) A reprocessed N95 respirator as opposed to a surgical mask for aerosol-generating procedures in a contingency or crisis setting.
7) Adding a face shield or surgical mask as a cover for an N95 respirator to allow for extended use during respirator shortages when performing aerosol-generating procedures in a contingency or crisis setting. This recommendation carries a caveat: It assumes correct doffing sequence and hand hygiene before and after taking off the face shield or surgical mask cover.
8) In the same scenario, adding a face shield or surgical mask over the N95 respirator so it can be reused, again assuming the correct sequence for hand hygiene.
The guideline was developed using the GRADE approach – for Grading of Recommendations Assessment, Development, and Evaluation – and a modified methodology for developing rapid recommendations. The levels of evidence supporting each recommendation vary from moderate for the first two to knowledge gap for the third and fourth to very low certainty for the last four.
“You can see that the eight recommendations that were made, a large part of them are really focused on masks, but there are a huge number of other disparate questions that need to be answered where there is really no good evidence basis,” Dr. Lynch said. “If we see any new evidence around that, we can at least provide commentary but I would really hope evidence-based recommendations around some of those interventions.”
Panel member Allison McGeer, MD, FRCPC, of the University of Toronto, explained the lack of evidence supporting infection prevention in hospitals. “In medicine we tend to look at individual patterns and individual patient outcomes,” she said. “When you’re looking at infection prevention, you’re looking at health systems and their outcomes, and it’s much harder to randomize hospitals or a state or a country to one particular policy about how to protect patients from infections in hospitals.”
The latest guidelines follow IDSA’s previously released guidelines on treatment and management of COVID-19 patients. The panel also plans to release guidelines on use of diagnostics for COVID-19 care.
Dr. Lynch has no financial relationships to disclose. Dr. McGeer disclosed relationships with Pfizer, Merck, Sanofi Pasteur, Seqirus, GlaxoSmithKline and Cidara.
SOURCE: Lynch JB et al. IDSA. April 27, 2020.
FROM INFECTIOUS DISEASE SOCIETY OF AMERICA
New tetracycline antibiotic effective in community-acquired bacterial pneumonia
Background: Community-acquired pneumonia (CAP) is a leading cause of hospitalization and death, particularly in the elderly. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of CAP pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and atypical organisms, such as Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae.
Study design: Phase 3 randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: Hospitalized patients (98.8%) in non-ICU settings at 86 sites in Europe, North America, South America, the Middle East, Africa, and Asia.
Synopsis: The trial recruited 774 adults with three or more CAP symptoms (cough, purulent sputum production, dyspnea, or pleuritic chest pain) and at least two abnormal vital signs, one or more clinical signs or laboratory findings associated with CAP, radiologically confirmed pneumonia, and a Pneumonia Severity Index (PSI) of II, III, or IV (with higher class numbers indicating a greater risk of death). Exclusion criteria included having clinically significant liver or renal insufficiency or having an immunocompromised state. The patients were randomized to receive either omadacycline or moxifloxacin intravenously with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy. Atypical organisms were implicated in 67% of CAPS with known cause, while Streptococcus pneumoniae and Haemophilus influenzae were implicated in 20% and 12%, respectively. Omadacycline was noninferior to moxifloxacin with respect to early clinical response (81.1% vs 82.7%, respectively) and posttreatment clinical response rates (87.6% vs. 85.1%). Mean duration of IV therapy was 5.7 days, and the mean total duration of therapy was 9.6 days in both groups. The frequency of adverse events (primarily gastrointestinal) was similar between the two groups.
Exclusion of the most severe CAP and immunocompromised patients limits generalizability of these results.
Bottom line: Omadacycline provides similar clinical benefit as moxifloxacin in the treatment of selected patients with CAP.
Citation: Stets R et al. Omadacycline for community-acquired bacterial pneumonia. N Eng J Med. 2019;380:517-27.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Community-acquired pneumonia (CAP) is a leading cause of hospitalization and death, particularly in the elderly. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of CAP pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and atypical organisms, such as Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae.
Study design: Phase 3 randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: Hospitalized patients (98.8%) in non-ICU settings at 86 sites in Europe, North America, South America, the Middle East, Africa, and Asia.
Synopsis: The trial recruited 774 adults with three or more CAP symptoms (cough, purulent sputum production, dyspnea, or pleuritic chest pain) and at least two abnormal vital signs, one or more clinical signs or laboratory findings associated with CAP, radiologically confirmed pneumonia, and a Pneumonia Severity Index (PSI) of II, III, or IV (with higher class numbers indicating a greater risk of death). Exclusion criteria included having clinically significant liver or renal insufficiency or having an immunocompromised state. The patients were randomized to receive either omadacycline or moxifloxacin intravenously with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy. Atypical organisms were implicated in 67% of CAPS with known cause, while Streptococcus pneumoniae and Haemophilus influenzae were implicated in 20% and 12%, respectively. Omadacycline was noninferior to moxifloxacin with respect to early clinical response (81.1% vs 82.7%, respectively) and posttreatment clinical response rates (87.6% vs. 85.1%). Mean duration of IV therapy was 5.7 days, and the mean total duration of therapy was 9.6 days in both groups. The frequency of adverse events (primarily gastrointestinal) was similar between the two groups.
Exclusion of the most severe CAP and immunocompromised patients limits generalizability of these results.
Bottom line: Omadacycline provides similar clinical benefit as moxifloxacin in the treatment of selected patients with CAP.
Citation: Stets R et al. Omadacycline for community-acquired bacterial pneumonia. N Eng J Med. 2019;380:517-27.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Community-acquired pneumonia (CAP) is a leading cause of hospitalization and death, particularly in the elderly. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of CAP pathogens, including Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, and atypical organisms, such as Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydia pneumoniae.
Study design: Phase 3 randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: Hospitalized patients (98.8%) in non-ICU settings at 86 sites in Europe, North America, South America, the Middle East, Africa, and Asia.
Synopsis: The trial recruited 774 adults with three or more CAP symptoms (cough, purulent sputum production, dyspnea, or pleuritic chest pain) and at least two abnormal vital signs, one or more clinical signs or laboratory findings associated with CAP, radiologically confirmed pneumonia, and a Pneumonia Severity Index (PSI) of II, III, or IV (with higher class numbers indicating a greater risk of death). Exclusion criteria included having clinically significant liver or renal insufficiency or having an immunocompromised state. The patients were randomized to receive either omadacycline or moxifloxacin intravenously with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy. Atypical organisms were implicated in 67% of CAPS with known cause, while Streptococcus pneumoniae and Haemophilus influenzae were implicated in 20% and 12%, respectively. Omadacycline was noninferior to moxifloxacin with respect to early clinical response (81.1% vs 82.7%, respectively) and posttreatment clinical response rates (87.6% vs. 85.1%). Mean duration of IV therapy was 5.7 days, and the mean total duration of therapy was 9.6 days in both groups. The frequency of adverse events (primarily gastrointestinal) was similar between the two groups.
Exclusion of the most severe CAP and immunocompromised patients limits generalizability of these results.
Bottom line: Omadacycline provides similar clinical benefit as moxifloxacin in the treatment of selected patients with CAP.
Citation: Stets R et al. Omadacycline for community-acquired bacterial pneumonia. N Eng J Med. 2019;380:517-27.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
AAD offers guidance for reopening practices
Dermatology practices that are resuming in-person services amid the ongoing pandemic face a range of questions and concerns when it comes to restarting patient visits.
To address these questions and considerations, the . Among the subjects covered are how practices can properly prepare clinic space to ensure staff and patients are safe and how to organize and educate employees on social distancing and safety protocols.
“All along, [we have] had guidance to help practices continue taking care of patients for essential services,” George J. Hruza, MD, immediate past president of the AAD, said in an interview. “This is really an extension of those as some states are opening up and relaxing some of the restrictions on elective procedures. We wanted to help our practices that are going to be reopening or going back to more regular services so they have a bit of a road map.”
The first step to reopening and resuming services is understanding your community’s COVID-19 prevalence and keeping updated on transmission information from local and state authorities, according to the AAD guidance. Keep in mind the federal government has specified that there should be a downward trajectory of documented cases over a 14-day period before opening practices to elective visits and procedures.
Preparing the practice through sanitation and reorganizing to minimize patient contact is also essential when reopening or resuming services. This includes cleaning and disinfecting based on World Health Organization standards, adding markings where necessary to maintain appropriate social distance, and supplying additional hand sanitizers and wipes for patients and staff, according to the guidance.
A top challenge as practices reopen is making patients feel comfortable with coming back to the practice for in-person care, said Dr. Hruza, who practices in St. Louis and is president of the Missouri State Medical Association. The AAD’s road map recommends informing patients about the reopening or reexpansion of elective procedures and communicating the steps the practice is taking to prevent COVID-19 infections and keep patients safe. It may be necessary to start with fewer patients than normal to adjust to the new safety steps until it becomes routine, according to the guidance.
Educating staff on social distancing and personal protective equipment (PPE) also is key. Staff should wear PPE for office staff meetings or sit at least 6 feet apart, according to the AAD guidelines. Practices also must determine what procedures may require additional PPE.
“If you’re doing some laser procedures, there may be a little more of a problem with tissue getting into the air or in the environment, so you may need to increase your protections a bit more,” Dr. Hruza said. “That may be a setting where you want to wear a N95 [mask].”
The AAD advises that practices be prepared to take necessary steps if a resurgence of COVID-19 cases in their community or clinic arises after reopening. Follow recommendations as they develop, be flexible, and be prepared to respond and reschedule patients, if necessary, Dr. Hruza said.
Dermatology practices that are resuming in-person services amid the ongoing pandemic face a range of questions and concerns when it comes to restarting patient visits.
To address these questions and considerations, the . Among the subjects covered are how practices can properly prepare clinic space to ensure staff and patients are safe and how to organize and educate employees on social distancing and safety protocols.
“All along, [we have] had guidance to help practices continue taking care of patients for essential services,” George J. Hruza, MD, immediate past president of the AAD, said in an interview. “This is really an extension of those as some states are opening up and relaxing some of the restrictions on elective procedures. We wanted to help our practices that are going to be reopening or going back to more regular services so they have a bit of a road map.”
The first step to reopening and resuming services is understanding your community’s COVID-19 prevalence and keeping updated on transmission information from local and state authorities, according to the AAD guidance. Keep in mind the federal government has specified that there should be a downward trajectory of documented cases over a 14-day period before opening practices to elective visits and procedures.
Preparing the practice through sanitation and reorganizing to minimize patient contact is also essential when reopening or resuming services. This includes cleaning and disinfecting based on World Health Organization standards, adding markings where necessary to maintain appropriate social distance, and supplying additional hand sanitizers and wipes for patients and staff, according to the guidance.
A top challenge as practices reopen is making patients feel comfortable with coming back to the practice for in-person care, said Dr. Hruza, who practices in St. Louis and is president of the Missouri State Medical Association. The AAD’s road map recommends informing patients about the reopening or reexpansion of elective procedures and communicating the steps the practice is taking to prevent COVID-19 infections and keep patients safe. It may be necessary to start with fewer patients than normal to adjust to the new safety steps until it becomes routine, according to the guidance.
Educating staff on social distancing and personal protective equipment (PPE) also is key. Staff should wear PPE for office staff meetings or sit at least 6 feet apart, according to the AAD guidelines. Practices also must determine what procedures may require additional PPE.
“If you’re doing some laser procedures, there may be a little more of a problem with tissue getting into the air or in the environment, so you may need to increase your protections a bit more,” Dr. Hruza said. “That may be a setting where you want to wear a N95 [mask].”
The AAD advises that practices be prepared to take necessary steps if a resurgence of COVID-19 cases in their community or clinic arises after reopening. Follow recommendations as they develop, be flexible, and be prepared to respond and reschedule patients, if necessary, Dr. Hruza said.
Dermatology practices that are resuming in-person services amid the ongoing pandemic face a range of questions and concerns when it comes to restarting patient visits.
To address these questions and considerations, the . Among the subjects covered are how practices can properly prepare clinic space to ensure staff and patients are safe and how to organize and educate employees on social distancing and safety protocols.
“All along, [we have] had guidance to help practices continue taking care of patients for essential services,” George J. Hruza, MD, immediate past president of the AAD, said in an interview. “This is really an extension of those as some states are opening up and relaxing some of the restrictions on elective procedures. We wanted to help our practices that are going to be reopening or going back to more regular services so they have a bit of a road map.”
The first step to reopening and resuming services is understanding your community’s COVID-19 prevalence and keeping updated on transmission information from local and state authorities, according to the AAD guidance. Keep in mind the federal government has specified that there should be a downward trajectory of documented cases over a 14-day period before opening practices to elective visits and procedures.
Preparing the practice through sanitation and reorganizing to minimize patient contact is also essential when reopening or resuming services. This includes cleaning and disinfecting based on World Health Organization standards, adding markings where necessary to maintain appropriate social distance, and supplying additional hand sanitizers and wipes for patients and staff, according to the guidance.
A top challenge as practices reopen is making patients feel comfortable with coming back to the practice for in-person care, said Dr. Hruza, who practices in St. Louis and is president of the Missouri State Medical Association. The AAD’s road map recommends informing patients about the reopening or reexpansion of elective procedures and communicating the steps the practice is taking to prevent COVID-19 infections and keep patients safe. It may be necessary to start with fewer patients than normal to adjust to the new safety steps until it becomes routine, according to the guidance.
Educating staff on social distancing and personal protective equipment (PPE) also is key. Staff should wear PPE for office staff meetings or sit at least 6 feet apart, according to the AAD guidelines. Practices also must determine what procedures may require additional PPE.
“If you’re doing some laser procedures, there may be a little more of a problem with tissue getting into the air or in the environment, so you may need to increase your protections a bit more,” Dr. Hruza said. “That may be a setting where you want to wear a N95 [mask].”
The AAD advises that practices be prepared to take necessary steps if a resurgence of COVID-19 cases in their community or clinic arises after reopening. Follow recommendations as they develop, be flexible, and be prepared to respond and reschedule patients, if necessary, Dr. Hruza said.
CGRP inhibitors receive reassuring real-world safety report
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
Stephen D. Silberstein, MD, reported online as part of the 2020 American Academy of Neurology Science Highlights.
He presented a retrospective analysis of spontaneous postmarketing reports to the Food and Drug Administration Adverse Events Reporting System (FAERS) for Aimovig (erenumab-aooe), Ajovy (fremanezumab-vfrm), and Emgality (galcanezumab-gnlm).
The top-10 lists of adverse events for all three monoclonal antibodies targeting CGRP were skewed heavily towards injection-site reactions, such as injection-site pain, itching, swelling, and erythema. The rates were relatively low. For example, injection-site pain was reported at a rate of 2.94 cases per 1,000 patients exposed to erenumab, 0.8/1,000 for fremanezumab, and 4.9/1,000 for galcanezumab, according to Dr. Silberstein, professor of neurology and director of the headache center at Sidney Kimmel Medical College, Philadelphia.
Migraine, headache, and drug ineffectiveness were in the top 10 for all three medications, as is typical in FAERS reports, since no drug is effective in everyone. These events were reported at rates of 1-5/1,000 exposed patients. Constipation was reported in association with the use of erenumab at a rate of 4.9 cases/1,000 patients, but did not reach the top-10 lists for the other two CGRP antagonists.
Notably, cardiovascular events were not among the top-10 adverse events reported for any of the novel preventive agents.
“These results will be practice changing, since some physicians have been holding back from prescribing these drugs pending the results of this sort of longer-term safety data,” Dr. Silberstein predicted in an interview.
Asked to comment on the FAERS study, neurologist Holly Yancy, DO, said that she found the findings unsurprising because the adverse effects were essentially as expected based upon the earlier favorable clinical trials experience.
“These medications are living up to the expectations for good tolerability that were in place when they were initially approved by the FDA just under 2 years ago,” said Dr. Yancy, a headache specialist at the Banner–University Medicine Neuroscience Institute in Phoenix.
“Injection-site reactions were anticipated. Clinically, I’ve found that if the medications reduce migraine days and severity, patients find the risk of temporary pain, redness, or itching at the injection site is an easy trade off,” she added.
CGRP is a vasoactive peptide. There has been a theoretic concern that its pharmacologic inhibition for prevention of migraine could lead to an increased risk of adverse cardiovascular events, especially in individuals with coronary disease or a history of stroke. The absence of any such signal during the first 6 months of widespread clinical use of the CGRP inhibitors is highly encouraging, although this is an issue that warrants longer-term study, Dr. Yancy continued.
These drugs, which were expressly designed for migraine prevention, are a considerable advance over what was previously available in her view. They’re equally or more effective and considerably better tolerated than the preventive medications physicians had long been using off label, including antidepressants, antiepileptics, and cardiac drugs.
Dr. Silberstein reported financial relationships with close to two dozen pharmaceutical companies. Dr. Yancy reported serving on speakers’ bureaus for Amgen and Novartis.
SOURCE: Silverstein SD et al. AAN 2020, Abstract S58.008.
FROM AAN 2020