User login
Semen cryopreservation viable for young transgender patients in small study
as transgender women, according to results of a small retrospective cohort study.
The lack of data on this topic, however, makes it difficult to determine how long an individual must be off gender-affirming therapy before spermatogenesis resumes, if it resumes, and what the long-term effects of gender-affirming therapy are.
“This information is critical to address as part of a multidisciplinary fertility discussion with youth and their guardians so that an informed decision can be made regarding fertility preservation use,” wrote Emily P. Barnard, DO, of UPMC Magee-Womens Hospital in Pittsburgh and her associates.
The researchers retrospectively collected data on transgender patients who sought fertility preservation between 2015 and 2018.
The 11 white transgender women (sex assigned male at birth) who followed up on adolescent medicine or pediatric endocrinology referrals for fertility preservation received their consultations between ages 16 and 24, with 19 years having been the median age at which they occurred. Gender dysphoria onset happened at a median age of 12 for the patients, who were evaluated for it at a median age of 17.
All but one patient submitted at least one semen sample, and eight ultimately cryopreserved their semen.
The eight samples from gender-affirming therapy–naive patients had abnormal morphology, with the median morphology having been 6% versus the normal range of greater than 13.0%. Otherwise, the samples collected were normal, but the authors noted that established semen analysis parameters don’t exist for adolescents and young adults.
All eight patients who had their semen cryopreserved, began gonadotropin-releasing hormone (GnRH) agonist therapy after cryopreservation, and four of those patients concurrently began taking estradiol.
One patient had already been taking intramuscular leuprolide acetate every 6 months and discontinued it to attempt fertility preservation. Spermatogenesis returned after 5 months of azoospermia, albeit with abnormal morphology (9%).
Another patient had been taking spironolactone and estradiol for 26 months before ceasing therapy to attempt fertility preservation. She remained azoospermic 4 months after stopping therapy and then moved forward with an orchiectomy.
“For many transgender patients, the potential need to discontinue GnRH agonist or gender-affirming therapy to allow for resumption of spermatogenesis may be a significant barrier to pursuing fertility preservation because cessation of therapy may result in exacerbation of gender dysphoria and progression of undesired male secondary sex characteristics,” the researchers wrote. “For individuals for whom this risk is not acceptable or if azoospermia is noted on semen analysis, there are several alternate options, including electroejaculation, testicular sperm extraction, and testicular tissue cryopreservation,” they continued. Electroejaculation with a transrectal probe is an option particularly for those who cannot masturbate or feel uncomfortable doing so, the authors explained.
For those who have not previously received gender-affirming therapy, the fertility preservation “process can be completed quickly, with collections occurring every 2 to 3 days to preserve several samples before initiating GnRH agonist or gender-affirming therapy,” they concluded.
SOURCE: Barnard EP et al. Pediatrics. 2019 Aug 5. doi: 10.1542/peds.2018-3943.
The lack of long-term data on various gender-affirming medical interventions, particularly hormone therapies, for transgender adolescents and young adults has led professional medical organizations to recommend patients receive fertility counseling before beginning any such therapies.
Yet few data exist on fertility preservation either. The study by Barnard et al. is the first to examine semen cryopreservation outcomes in adolescents and young adults assigned male at birth and asserting a female gender identity.
“There is often urgency to start medical affirming interventions (MAI) among transgender and gender-diverse adolescents and young adults (TGD-AYA) due to gender dysphoria and related psychological sequelae,” wrote Jason Rafferty, MD, MPH, in an accompanying editorial. “However, starting MAI immediately and delaying fertility services may lead to increased overall morbidity for some patients.”
Although multiple professional organizations recommend fertility counseling before MAI initiation, many transgender patients are not following this advice. Dr. Rafferty noted one study found only 20% of TGD-AYA discussed fertility with their physicians before beginning MAI, and only 13% discussed possible effects of MAI on fertility – yet 60% wanted to learn more.
“Barnard et al. review data suggesting TGD-AYA have low interest in fertility services, but many TGD-AYA questioned whether this may later change,” Dr. Rafferty wrote. “After starting MAIs, TGD-AYA report being more emotionally capable of considering future parenting because of increasing comfort with their bodies and romantic relationships.”
Various barriers also exist for TGD-AYA interested in fertility services, such as cost, lack of insurance coverage, low availability of services, increased dysphoria from the procedures, stereotypes, stigma, and interest in starting MAI as soon as possible.
“Under a reproductive justice framework, autonomy around family planning is a right that should not be limited by structural or systemic barriers,” Dr. Rafferty wrote. “Overall, there is a clinical and ethical imperative to better understand and provide access to fertility services for TGD-AYA.”
Jason Rafferty, MD, MPH, is a pediatrician and child psychiatrist who practices at the gender and sexuality clinic in Riverside and at the Adolescent Healthcare Center at Hasbro Children’s Hospital in Providence, R.I. His comments are summarized from an accompanying editorial (Pediatrics 2019 Aug 5. doi: 10.1542/peds.2019-2000).
The lack of long-term data on various gender-affirming medical interventions, particularly hormone therapies, for transgender adolescents and young adults has led professional medical organizations to recommend patients receive fertility counseling before beginning any such therapies.
Yet few data exist on fertility preservation either. The study by Barnard et al. is the first to examine semen cryopreservation outcomes in adolescents and young adults assigned male at birth and asserting a female gender identity.
“There is often urgency to start medical affirming interventions (MAI) among transgender and gender-diverse adolescents and young adults (TGD-AYA) due to gender dysphoria and related psychological sequelae,” wrote Jason Rafferty, MD, MPH, in an accompanying editorial. “However, starting MAI immediately and delaying fertility services may lead to increased overall morbidity for some patients.”
Although multiple professional organizations recommend fertility counseling before MAI initiation, many transgender patients are not following this advice. Dr. Rafferty noted one study found only 20% of TGD-AYA discussed fertility with their physicians before beginning MAI, and only 13% discussed possible effects of MAI on fertility – yet 60% wanted to learn more.
“Barnard et al. review data suggesting TGD-AYA have low interest in fertility services, but many TGD-AYA questioned whether this may later change,” Dr. Rafferty wrote. “After starting MAIs, TGD-AYA report being more emotionally capable of considering future parenting because of increasing comfort with their bodies and romantic relationships.”
Various barriers also exist for TGD-AYA interested in fertility services, such as cost, lack of insurance coverage, low availability of services, increased dysphoria from the procedures, stereotypes, stigma, and interest in starting MAI as soon as possible.
“Under a reproductive justice framework, autonomy around family planning is a right that should not be limited by structural or systemic barriers,” Dr. Rafferty wrote. “Overall, there is a clinical and ethical imperative to better understand and provide access to fertility services for TGD-AYA.”
Jason Rafferty, MD, MPH, is a pediatrician and child psychiatrist who practices at the gender and sexuality clinic in Riverside and at the Adolescent Healthcare Center at Hasbro Children’s Hospital in Providence, R.I. His comments are summarized from an accompanying editorial (Pediatrics 2019 Aug 5. doi: 10.1542/peds.2019-2000).
The lack of long-term data on various gender-affirming medical interventions, particularly hormone therapies, for transgender adolescents and young adults has led professional medical organizations to recommend patients receive fertility counseling before beginning any such therapies.
Yet few data exist on fertility preservation either. The study by Barnard et al. is the first to examine semen cryopreservation outcomes in adolescents and young adults assigned male at birth and asserting a female gender identity.
“There is often urgency to start medical affirming interventions (MAI) among transgender and gender-diverse adolescents and young adults (TGD-AYA) due to gender dysphoria and related psychological sequelae,” wrote Jason Rafferty, MD, MPH, in an accompanying editorial. “However, starting MAI immediately and delaying fertility services may lead to increased overall morbidity for some patients.”
Although multiple professional organizations recommend fertility counseling before MAI initiation, many transgender patients are not following this advice. Dr. Rafferty noted one study found only 20% of TGD-AYA discussed fertility with their physicians before beginning MAI, and only 13% discussed possible effects of MAI on fertility – yet 60% wanted to learn more.
“Barnard et al. review data suggesting TGD-AYA have low interest in fertility services, but many TGD-AYA questioned whether this may later change,” Dr. Rafferty wrote. “After starting MAIs, TGD-AYA report being more emotionally capable of considering future parenting because of increasing comfort with their bodies and romantic relationships.”
Various barriers also exist for TGD-AYA interested in fertility services, such as cost, lack of insurance coverage, low availability of services, increased dysphoria from the procedures, stereotypes, stigma, and interest in starting MAI as soon as possible.
“Under a reproductive justice framework, autonomy around family planning is a right that should not be limited by structural or systemic barriers,” Dr. Rafferty wrote. “Overall, there is a clinical and ethical imperative to better understand and provide access to fertility services for TGD-AYA.”
Jason Rafferty, MD, MPH, is a pediatrician and child psychiatrist who practices at the gender and sexuality clinic in Riverside and at the Adolescent Healthcare Center at Hasbro Children’s Hospital in Providence, R.I. His comments are summarized from an accompanying editorial (Pediatrics 2019 Aug 5. doi: 10.1542/peds.2019-2000).
as transgender women, according to results of a small retrospective cohort study.
The lack of data on this topic, however, makes it difficult to determine how long an individual must be off gender-affirming therapy before spermatogenesis resumes, if it resumes, and what the long-term effects of gender-affirming therapy are.
“This information is critical to address as part of a multidisciplinary fertility discussion with youth and their guardians so that an informed decision can be made regarding fertility preservation use,” wrote Emily P. Barnard, DO, of UPMC Magee-Womens Hospital in Pittsburgh and her associates.
The researchers retrospectively collected data on transgender patients who sought fertility preservation between 2015 and 2018.
The 11 white transgender women (sex assigned male at birth) who followed up on adolescent medicine or pediatric endocrinology referrals for fertility preservation received their consultations between ages 16 and 24, with 19 years having been the median age at which they occurred. Gender dysphoria onset happened at a median age of 12 for the patients, who were evaluated for it at a median age of 17.
All but one patient submitted at least one semen sample, and eight ultimately cryopreserved their semen.
The eight samples from gender-affirming therapy–naive patients had abnormal morphology, with the median morphology having been 6% versus the normal range of greater than 13.0%. Otherwise, the samples collected were normal, but the authors noted that established semen analysis parameters don’t exist for adolescents and young adults.
All eight patients who had their semen cryopreserved, began gonadotropin-releasing hormone (GnRH) agonist therapy after cryopreservation, and four of those patients concurrently began taking estradiol.
One patient had already been taking intramuscular leuprolide acetate every 6 months and discontinued it to attempt fertility preservation. Spermatogenesis returned after 5 months of azoospermia, albeit with abnormal morphology (9%).
Another patient had been taking spironolactone and estradiol for 26 months before ceasing therapy to attempt fertility preservation. She remained azoospermic 4 months after stopping therapy and then moved forward with an orchiectomy.
“For many transgender patients, the potential need to discontinue GnRH agonist or gender-affirming therapy to allow for resumption of spermatogenesis may be a significant barrier to pursuing fertility preservation because cessation of therapy may result in exacerbation of gender dysphoria and progression of undesired male secondary sex characteristics,” the researchers wrote. “For individuals for whom this risk is not acceptable or if azoospermia is noted on semen analysis, there are several alternate options, including electroejaculation, testicular sperm extraction, and testicular tissue cryopreservation,” they continued. Electroejaculation with a transrectal probe is an option particularly for those who cannot masturbate or feel uncomfortable doing so, the authors explained.
For those who have not previously received gender-affirming therapy, the fertility preservation “process can be completed quickly, with collections occurring every 2 to 3 days to preserve several samples before initiating GnRH agonist or gender-affirming therapy,” they concluded.
SOURCE: Barnard EP et al. Pediatrics. 2019 Aug 5. doi: 10.1542/peds.2018-3943.
as transgender women, according to results of a small retrospective cohort study.
The lack of data on this topic, however, makes it difficult to determine how long an individual must be off gender-affirming therapy before spermatogenesis resumes, if it resumes, and what the long-term effects of gender-affirming therapy are.
“This information is critical to address as part of a multidisciplinary fertility discussion with youth and their guardians so that an informed decision can be made regarding fertility preservation use,” wrote Emily P. Barnard, DO, of UPMC Magee-Womens Hospital in Pittsburgh and her associates.
The researchers retrospectively collected data on transgender patients who sought fertility preservation between 2015 and 2018.
The 11 white transgender women (sex assigned male at birth) who followed up on adolescent medicine or pediatric endocrinology referrals for fertility preservation received their consultations between ages 16 and 24, with 19 years having been the median age at which they occurred. Gender dysphoria onset happened at a median age of 12 for the patients, who were evaluated for it at a median age of 17.
All but one patient submitted at least one semen sample, and eight ultimately cryopreserved their semen.
The eight samples from gender-affirming therapy–naive patients had abnormal morphology, with the median morphology having been 6% versus the normal range of greater than 13.0%. Otherwise, the samples collected were normal, but the authors noted that established semen analysis parameters don’t exist for adolescents and young adults.
All eight patients who had their semen cryopreserved, began gonadotropin-releasing hormone (GnRH) agonist therapy after cryopreservation, and four of those patients concurrently began taking estradiol.
One patient had already been taking intramuscular leuprolide acetate every 6 months and discontinued it to attempt fertility preservation. Spermatogenesis returned after 5 months of azoospermia, albeit with abnormal morphology (9%).
Another patient had been taking spironolactone and estradiol for 26 months before ceasing therapy to attempt fertility preservation. She remained azoospermic 4 months after stopping therapy and then moved forward with an orchiectomy.
“For many transgender patients, the potential need to discontinue GnRH agonist or gender-affirming therapy to allow for resumption of spermatogenesis may be a significant barrier to pursuing fertility preservation because cessation of therapy may result in exacerbation of gender dysphoria and progression of undesired male secondary sex characteristics,” the researchers wrote. “For individuals for whom this risk is not acceptable or if azoospermia is noted on semen analysis, there are several alternate options, including electroejaculation, testicular sperm extraction, and testicular tissue cryopreservation,” they continued. Electroejaculation with a transrectal probe is an option particularly for those who cannot masturbate or feel uncomfortable doing so, the authors explained.
For those who have not previously received gender-affirming therapy, the fertility preservation “process can be completed quickly, with collections occurring every 2 to 3 days to preserve several samples before initiating GnRH agonist or gender-affirming therapy,” they concluded.
SOURCE: Barnard EP et al. Pediatrics. 2019 Aug 5. doi: 10.1542/peds.2018-3943.
FROM PEDIATRICS
COPD adds complexity to shared decision making for LDCT lung cancer screening
research suggests.
Jonathan M. Iaccarino, MD, of the pulmonary center at the Boston University, and coauthors reported the results of a secondary analysis of patient-level outcomes from 75,138 low-dose CT (LDCT) scans in 26,453 participants in the National Lung Screening Trial (Chest 2019 Jul 5. doi: 10.1016/j.chest.2019.06.016).
Currently, LDCT screening is recommended annually for high-risk smokers aged 55-80 years. The National Lung Screening Trial showed that this screening achieved a 20% relative reduction in lung cancer mortality and 6.7% relative reduction in overall mortality in this group. The guidelines stress the importance of shared decision making, with discussion of the risks and benefits of screening.
Dr. Iaccarino and colleagues point out that decision aids for shared decision making need to include important baseline characteristics, such as the presence of COPD, as these can complicate the risk and benefit analysis.
In this study, they found that 14.2% of LDCT scans performed led to a subsequent diagnostic study and 1.5% resulted in an invasive procedure. In addition, 0.3% of scans resulted in a procedure-related complication, and in 89 cases (0.1%), this procedure-related complication was serious.
At the patient level, nearly one-third (30.5%) received a diagnostic study, 4.2% underwent an invasive procedure – 41% of whom ultimately were found not to have lung cancer – 0.9% had a procedure-related complication, and 0.3% had a serious procedure related complication. Furthermore, among those who experienced a serious complication, 12.5% were found not to have lung cancer.
“Our study analyzes cumulative outcomes at the level of the individual patient over the three years of LDCT screening during the NLST, showing higher rates of diagnostic procedures, invasive procedures, complications and serious complications than apparent when data is presented at the level of the individual test,” the authors wrote.
The 4,632 participants with COPD were significantly more likely to undergo diagnostic studies (36.2%), have an invasive procedure (6%), experience a procedure-related complication (1.5%) and experience a serious procedure-related complication (0.6%) than were participants without COPD. However, they also had a significantly higher incidence of lung cancer diagnosis than did participants without COPD (6.1% vs. 3.6%).
“While most decision aids note the risks of screening may be increased in those with COPD, our study helps quantify these increased risks as well as the increased likelihood of a lung cancer diagnosis, a critical advance given that providing personalized (rather than generic) information results in more accurate risk perception and more informed choices among individuals considering screening,” the authors wrote. “With the significant change in the balance of benefits and risks of screening in patients with COPD, it is critical to adjust the shared decision-making discussions accordingly.”
They also noted that other comorbidities, such as heart disease, vascular disease, and other lung diseases, would likely affect the balance of risk and benefit of LDCT screening, and that there was a need for further exploration of screening in these patients.
Noting the study’s limitations, the authors pointed that their analysis focused on outcomes that were not the primary outcomes of the National Lung Screening trial, and that they relied on self-reported COPD diagnoses.
The study was supported by the American Society of Clinical Oncology, the Charles A. King Trust, and Edith Nourse Rogers Memorial Veterans Hospital. No conflicts of interest were declared.
SOURCE: Iaccarino JM et al. CHEST 2019 Jul 5. doi: 10.1016/j.chest.2019.06.016.
research suggests.
Jonathan M. Iaccarino, MD, of the pulmonary center at the Boston University, and coauthors reported the results of a secondary analysis of patient-level outcomes from 75,138 low-dose CT (LDCT) scans in 26,453 participants in the National Lung Screening Trial (Chest 2019 Jul 5. doi: 10.1016/j.chest.2019.06.016).
Currently, LDCT screening is recommended annually for high-risk smokers aged 55-80 years. The National Lung Screening Trial showed that this screening achieved a 20% relative reduction in lung cancer mortality and 6.7% relative reduction in overall mortality in this group. The guidelines stress the importance of shared decision making, with discussion of the risks and benefits of screening.
Dr. Iaccarino and colleagues point out that decision aids for shared decision making need to include important baseline characteristics, such as the presence of COPD, as these can complicate the risk and benefit analysis.
In this study, they found that 14.2% of LDCT scans performed led to a subsequent diagnostic study and 1.5% resulted in an invasive procedure. In addition, 0.3% of scans resulted in a procedure-related complication, and in 89 cases (0.1%), this procedure-related complication was serious.
At the patient level, nearly one-third (30.5%) received a diagnostic study, 4.2% underwent an invasive procedure – 41% of whom ultimately were found not to have lung cancer – 0.9% had a procedure-related complication, and 0.3% had a serious procedure related complication. Furthermore, among those who experienced a serious complication, 12.5% were found not to have lung cancer.
“Our study analyzes cumulative outcomes at the level of the individual patient over the three years of LDCT screening during the NLST, showing higher rates of diagnostic procedures, invasive procedures, complications and serious complications than apparent when data is presented at the level of the individual test,” the authors wrote.
The 4,632 participants with COPD were significantly more likely to undergo diagnostic studies (36.2%), have an invasive procedure (6%), experience a procedure-related complication (1.5%) and experience a serious procedure-related complication (0.6%) than were participants without COPD. However, they also had a significantly higher incidence of lung cancer diagnosis than did participants without COPD (6.1% vs. 3.6%).
“While most decision aids note the risks of screening may be increased in those with COPD, our study helps quantify these increased risks as well as the increased likelihood of a lung cancer diagnosis, a critical advance given that providing personalized (rather than generic) information results in more accurate risk perception and more informed choices among individuals considering screening,” the authors wrote. “With the significant change in the balance of benefits and risks of screening in patients with COPD, it is critical to adjust the shared decision-making discussions accordingly.”
They also noted that other comorbidities, such as heart disease, vascular disease, and other lung diseases, would likely affect the balance of risk and benefit of LDCT screening, and that there was a need for further exploration of screening in these patients.
Noting the study’s limitations, the authors pointed that their analysis focused on outcomes that were not the primary outcomes of the National Lung Screening trial, and that they relied on self-reported COPD diagnoses.
The study was supported by the American Society of Clinical Oncology, the Charles A. King Trust, and Edith Nourse Rogers Memorial Veterans Hospital. No conflicts of interest were declared.
SOURCE: Iaccarino JM et al. CHEST 2019 Jul 5. doi: 10.1016/j.chest.2019.06.016.
research suggests.
Jonathan M. Iaccarino, MD, of the pulmonary center at the Boston University, and coauthors reported the results of a secondary analysis of patient-level outcomes from 75,138 low-dose CT (LDCT) scans in 26,453 participants in the National Lung Screening Trial (Chest 2019 Jul 5. doi: 10.1016/j.chest.2019.06.016).
Currently, LDCT screening is recommended annually for high-risk smokers aged 55-80 years. The National Lung Screening Trial showed that this screening achieved a 20% relative reduction in lung cancer mortality and 6.7% relative reduction in overall mortality in this group. The guidelines stress the importance of shared decision making, with discussion of the risks and benefits of screening.
Dr. Iaccarino and colleagues point out that decision aids for shared decision making need to include important baseline characteristics, such as the presence of COPD, as these can complicate the risk and benefit analysis.
In this study, they found that 14.2% of LDCT scans performed led to a subsequent diagnostic study and 1.5% resulted in an invasive procedure. In addition, 0.3% of scans resulted in a procedure-related complication, and in 89 cases (0.1%), this procedure-related complication was serious.
At the patient level, nearly one-third (30.5%) received a diagnostic study, 4.2% underwent an invasive procedure – 41% of whom ultimately were found not to have lung cancer – 0.9% had a procedure-related complication, and 0.3% had a serious procedure related complication. Furthermore, among those who experienced a serious complication, 12.5% were found not to have lung cancer.
“Our study analyzes cumulative outcomes at the level of the individual patient over the three years of LDCT screening during the NLST, showing higher rates of diagnostic procedures, invasive procedures, complications and serious complications than apparent when data is presented at the level of the individual test,” the authors wrote.
The 4,632 participants with COPD were significantly more likely to undergo diagnostic studies (36.2%), have an invasive procedure (6%), experience a procedure-related complication (1.5%) and experience a serious procedure-related complication (0.6%) than were participants without COPD. However, they also had a significantly higher incidence of lung cancer diagnosis than did participants without COPD (6.1% vs. 3.6%).
“While most decision aids note the risks of screening may be increased in those with COPD, our study helps quantify these increased risks as well as the increased likelihood of a lung cancer diagnosis, a critical advance given that providing personalized (rather than generic) information results in more accurate risk perception and more informed choices among individuals considering screening,” the authors wrote. “With the significant change in the balance of benefits and risks of screening in patients with COPD, it is critical to adjust the shared decision-making discussions accordingly.”
They also noted that other comorbidities, such as heart disease, vascular disease, and other lung diseases, would likely affect the balance of risk and benefit of LDCT screening, and that there was a need for further exploration of screening in these patients.
Noting the study’s limitations, the authors pointed that their analysis focused on outcomes that were not the primary outcomes of the National Lung Screening trial, and that they relied on self-reported COPD diagnoses.
The study was supported by the American Society of Clinical Oncology, the Charles A. King Trust, and Edith Nourse Rogers Memorial Veterans Hospital. No conflicts of interest were declared.
SOURCE: Iaccarino JM et al. CHEST 2019 Jul 5. doi: 10.1016/j.chest.2019.06.016.
FROM CHEST
Gastrointestinal Stromal Tumors: Management of Advanced Disease
Most advanced gastrointestinal stromal tumors (GISTs) are due to a recurrence of localized disease, with only a small minority presenting with metastatic disease.1 Compared with chemotherapy, tyrosine kinase inhibitors (TKIs) have significantly improved the natural history of the disease, with median overall survival (OS) increasing from less than 1 year to about 5 years and approximately 1 in 5 patients achieving long-term survival.2 In addition, newer drugs in development and in clinical trials appear promising and have the potential to improve outcomes even further. This article reviews current evidence on options for treating metastatic or recurrent GISTs and GISTs that have progressed following initial therapy. The evaluation and diagnosis of GIST along with management of localized disease are reviewed in a separate article.
Case Presentation
A 64-year-old African American man underwent surgical resection of a 10-cm gastric mass, which pathology reported was positive for CD117, DOG1, and CD34 and negative for smooth muscle actin and S-100, consistent with a diagnosis of GIST. There were 10 mitoses per 50 HPF, and there was no intraoperative or intraperitoneal tumor rupture. The patient was treated with adjuvant imatinib, which was discontinued after 3 years due to grade 2 myalgias, periorbital edema, and macrocytic anemia. Surveillance included office visits every 3 to 6 months and a contrast CT abdomen and pelvis every 6 months. For the past 5 years, he has not had any clinical or radiographic evidence of disease recurrence. New imaging reveals multiple liver metastases and peritoneal implants. He feels fatigued and has lost about 10 lb since his last visit. He is 5 years out from his initial diagnosis and 2 years out from last receiving imatinib. His original tumor harbored a KIT exon 11 deletion.
What treatment should you recommend now?
Imatinib for Advanced GISTs
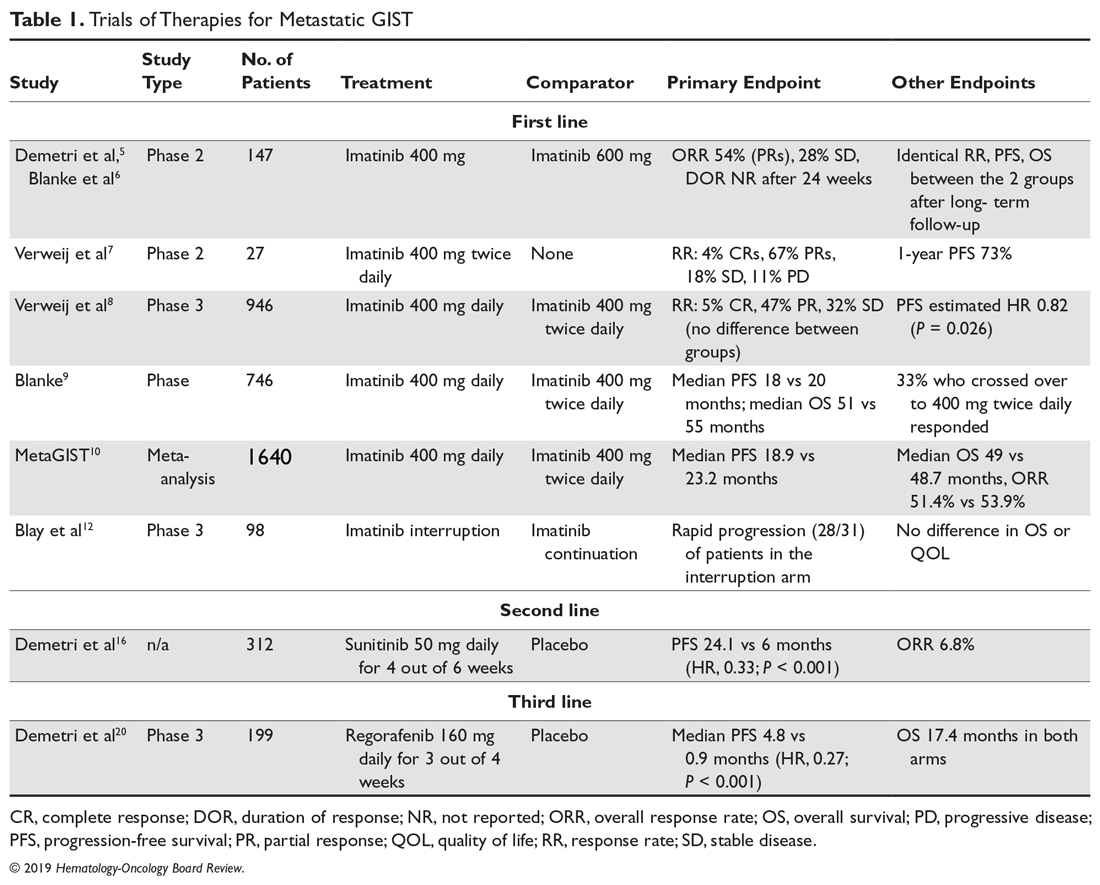
Before the first report of the efficacy of imatinib for metastatic GISTs in 2002, patients with advanced unresectable or metastatic GISTs were routinely treated with doxorubicin-based chemotherapy regimens, which were largely ineffective, with response rates (RRs) of around 5% and a median overall survival (OS) of less than 1 year.3,4 In 2002 a landmark phase 2 study revealed imatinib’s significant efficacy profile in advanced or metastatic GISTs, resulting in its approval by the US Food and Drug Administration (FDA).5 In this study, 147 patients with CD117-positive GISTs were randomly assigned to receive daily imatinib 400 mg or 600 mg for up to 36 months. The RRs were similar between the 2 groups (68.5% vs 67.6%), with a median time to response of 12 weeks and median duration of response of 118 days. Results of this study were much more favorable when compared to doxorubicin, rendering imatinib the new standard of care for advanced GISTs. A long-term follow-up of this study after a median of 63 months confirmed near identical RRs, progression-free survival (PFS), and median survival of 57 months among the 2 groups.6
Imatinib Daily Dosing
Although 400 mg of daily imatinib proved to be efficacious, it was unclear if a dose-response relationship existed for imatinib. An EORTC phase 2 study demonstrated a benefit of using a higher dose of imatinib at 400 mg twice daily, producing a RR of 71% (4% complete , 67% partial) and 1-year PFS of 73%, which appeared favorable compared with once-daily dosing and set the framework for larger phase 3 studies.7 Two phase 3 studies compared imatinib 400 mg once daily versus twice daily (until disease progression or unacceptable toxicity) among patients with CD117-positive advanced or metastatic GISTs. These studies were eventually combined into a meta-analysis (metaGIST) to compare RR, PFS and OS between the treatment groups. Both studies allowed cross-over to the 800 mg dose for patients who progressed on 400 mg daily.
The first study, conducted jointly by the EORTC, Italian Sarcoma Group, and Australasian Gastro-Intestinal Trials Group (EU-AUS),8 randomly assigned 946 patients to 400 mg once daily or twice daily. There were no differences in response rates between the groups, but the twice-daily group had a predicted 18% reduction in the hazard for progression compared with the once-daily group (estimated HR, 0.82; P = 0.026), which came at the expense of greater toxicities warranting dose reductions (60%) and treatment interruptions (64%). Cross-over to high-dose imatinib was feasible and safe, producing a partial response in 2%, stable disease in 27%, and a median PFS of 81 days. The second study was an intergroup study conducted jointly by SWOG, CALGB, NCI-C, and ECOG (S0033, US-CDN), with a nearly identical study design as the EU-AUS trial.9 The trial enrolled 746 patients. After a median follow up of 4.5 years, the median PFS and OS were not statistically different (18 vs 20 months and 55 vs 51 months, respectively). There were also no differences in response rates. One third of patients initially placed on the once-daily arm who crossed over after progression achieved a treatment response or stable disease.
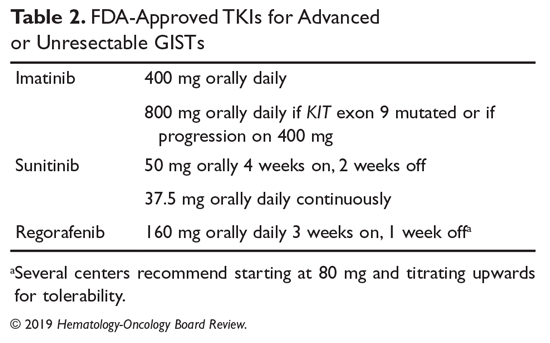
The combined EU-AUS and US-CDN analysis (metaGIST) included 1640 patients with a median age of 60 years and 58% of whom were men; 818 and 822 patients were assigned to the 400 mg and 800 mg total daily doses, respectively.10 The median follow-up was 37.5 months. There were no differences in OS (49 vs 48.7 months), median PFS (18.9 vs 23.2 months), or overall response rates (51.4% vs 53.9%). Patients who had crossed over (n = 347) to the 800 mg total daily dose arm had a 7.7-month average PFS while on the higher daily dose. An analysis was performed on 377 patients in the EU-AUS trial assessing the impact of mutational status on clinical outcomes among imatinib-treated patients. KIT exon 9 activating mutations were found to be a significant independent prognostic factor for death when compared with KIT exon 11 mutations. However, the adverse prognostic value of KIT exon 9 mutations was partially overcome with higher doses of imatinib, as those who received 800 mg total had a significantly better PFS, with a 61% relative risk reduction, than those who received 400 mg. Altogether, it was concluded that imatinib 400 mg once daily should be the standard-of-care first-line treatment for advanced or metastatic GISTs, unless a KIT exon 9 mutation is present, in which case imatinib 800 mg should be considered, if 400 mg is well tolerated. In addition, patients treated with frontline imatinib at 400 mg once daily, if tolerated well, should be considered for imatinib 800 mg upon progression of disease.
Despite there being problems with secondary resistance, significant progress has occurred in the treatment of metastatic disease over a short period of time. Prior to 2000, median OS for patients with metastatic GISTs was 9 months. With the introduction of imatinib and other TKIs, the median OS has increased to 5 years, with an estimated 10-year OS rate of approximately 20%.2
Imatinib Interruption
Since at this point, imatinib was a well-established standard of care for advanced GISTs, it was questioned whether imatinib therapy could be interrupted. At this time, treatment interruption in a stop-and-go fashion was deemed feasible in other metastatic solid tumors such as colorectal cancer (OPTIMOX1).11 The BFR French trial showed that stopping imatinib therapy in patients who had a response or stable disease after 1, 3, or 5 years was generally followed by relatively rapid tumor progression (approximately 50% of patients within 6 months), even when tumors were previously removed.12 Therefore, it is recommended that treatment in the metastatic setting should be continued indefinitely, unless there is disease progression. Hence, unlike with colorectal cancer or chronic myelogenous leukemia, as of now there is no role for imatinib interruption in metastatic GISTs.
Case Continued
The patient is started on imatinib 400 mg daily, and overall he tolerates therapy well. Interval CT imaging reveals a treatment response. Two years later, imaging reveals an increase in the tumor size and density with a new nodule present within a preexisting mass. There are no clinical trials in the area.
What defines tumor progression?
Disease Progression
When GISTs are responding to treatment, on imaging the tumors can become more cystic and less dense but with an increase in size. In addition, tumor progression may not always be associated with increased size—increased density of the tumor or a nodule within a mass that may indicate progression. If CT imaging is equivocal for progression, positron emission tomography (PET) can play a role in identifying true progression. It is critically important that tumor size and density are carefully assessed when performing interval imaging. Of note, radiofrequency ablation, cryotherapy, or chemoembolization can be used for symptomatic liver metastases or oligometastatic disease. When evaluating for progression, one needs to ask patients about compliance (ie, maintaining dose intensity related to side effects of therapy as well as the financial burden of treatment—copay toxicity).
What are mechanisms of secondary imatinib resistance?
Imatinib resistance can be subtle in patients with GISTs, manifesting with new nodular, enhancing foci enclosed within a preexisting mass (resistant clonal nodule), or can be clinically or radiographically overt.13 Imatinib resistance occurs through multiple mechanisms including acquisition of secondary activating KIT mutations in the intracellular ATP-binding domain (exons 13 and 14) and the activation loop (exons 17 and 18).14
What are the treatment options for this patient?
Second-line Therapy
Sunitinib malate is a multitargeted TKI that not only targets c-Kit and PDGFRA, but also has anti-angiogenic activity through inhibition of vascular endothelial growth factor receptors (VEGFR). Sunitinib gained FDA approval for the second-line treatment of advanced GISTs based on an international double-blind trial that randomized 312 patients with imatinib-resistant metastatic GISTs in a 2:1 fashion to receive sunitinib 50 mg daily for 4 weeks on and 2 weeks off or placebo.15,16 The trial was unblinded early at the planned interim analysis, which revealed a marked benefit, producing a 66% reduction in the hazard risk of progression (27.3 vs 6.4 weeks, HR, 0.33; P < 0.001). The most common treatment-related adverse events were fatigue, diarrhea, skin discoloration, nausea, and hand-foot syndrome. Another open-label phase 2 study assessed a continuous dosing schema of sunitinib 37.5 mg daily, which has been shown to be effective with less toxicity.17 Among the 60 patients enrolled, the primary endpoint of clinical benefit rate at 24 weeks was reached in 53%, which consisted of 13% partial responses and 40% stable disease. Most toxicities were grade 1 or 2 and easily manageable through standard interventions. This has been recommended as an alternative to the initial scheduled regimen.18 Part of sunitinib’s success is its activity against GISTs harboring secondary KIT exon 13 and 14 mutations, and possibly its anti-angiogenic activity.19 Sunitinib is particularly efficacious among GISTs harboring KIT exon 9 mutations.
Third-line Therapy
Patients who have progressed on prior imatinib and sunitinib can receive third-line regorafenib, a multi-TKI that differs chemically from sorafenib by a fluorouracil group (fluoro-sorafenib). FDA approval of regorafenib was based on the phase 3 GRID (GIST Regorafenib In progressive Disease) multicenter international trial.20 This trial randomly assigned 199 patients in a 2:1 fashion to receive regorafenib 160 mg daily for 21 days out of 28-day cycles plus best supportive care (BSC) versus placebo plus BSC. Cross-over was allowed. Regorafenib significantly reduced the hazard risk of progression by 73% compared with placebo (4.8 vs 0.9 months; HR, 0.27; P < 0.001). There was no difference in OS, which may be because of cross-over (median OS, 17.4 months in both arms). As a result, regorafenib is now considered standard third-line treatment for patients with metastatic GISTs. It has a less favorable toxicity profile than imatinib, with hand-foot syndrome, transaminitis, hypertension and fatigue being the most common treatment toxicities. In order to avoid noncompliance, it is recommended to start at 80 mg and carefully titrate upwards to the 160 mg dose.
A list of landmark studies for advanced GISTs is provided in Table 1.
A summary of FDA-approved drugs for treating GISTs is provided in Table 2.
Clinical Trials
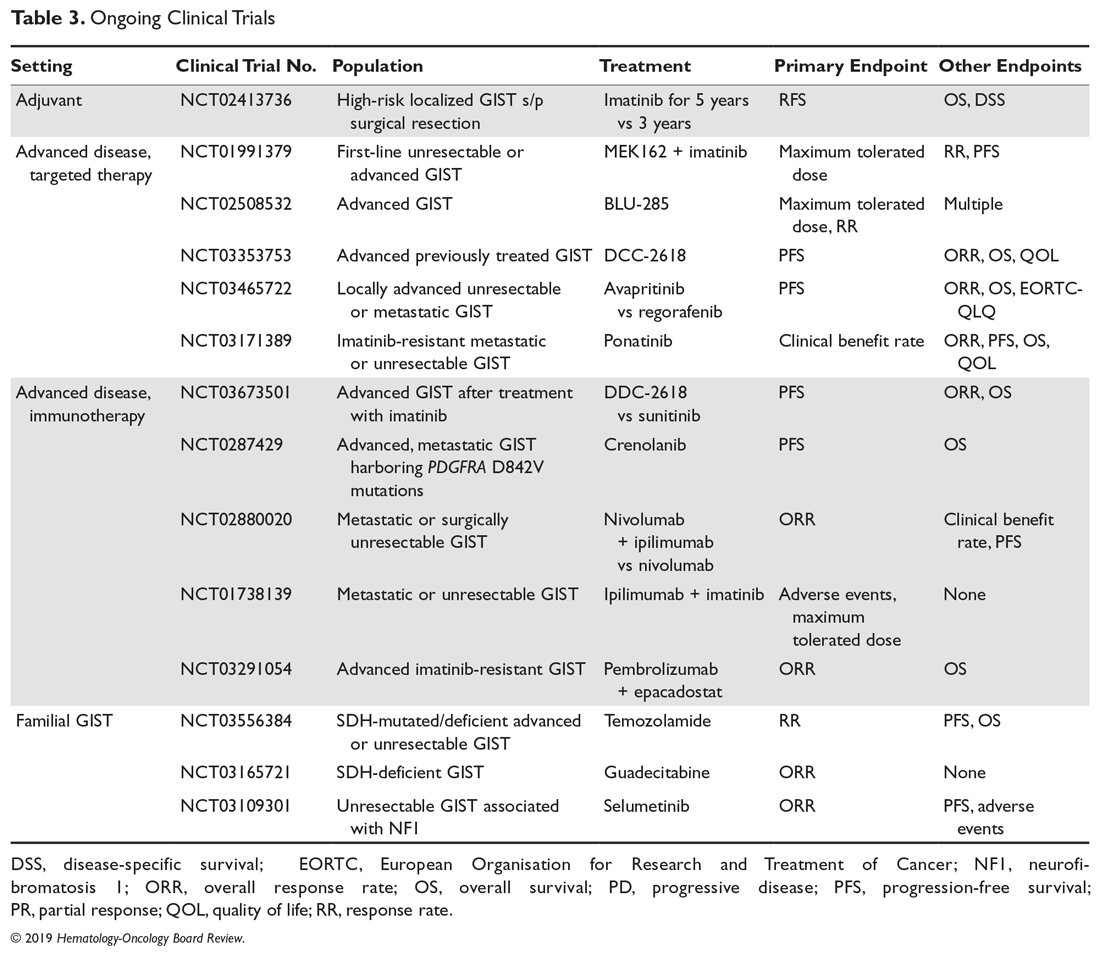
Clinical trial enrollment should be considered for all patients with advanced or unresectable GISTs throughout their treatment continuum. Owing to significant advances in genomic profiling through next-generation sequencing, multiple driver mutations have recently been identified, and targeted therapies are being explored in clinical trials.21 For example, the neurotrophic receptor tyrosine kinase (NTRK) gene appears to be mutated in a small number of advanced GISTs, and these can respond to the highly selective TRK inhibitor larotrectinib.22 Additionally, ongoing studies are assessing immunotherapies for sporadic GISTs and treatment for familial GISTs (Table 3). Some notable studies include those assessing the efficacy of agents that target KIT and PDGFR secondary mutations, including avapritinib (BLU-285) and DCC-2618, MEK inhibitors, and the multi-kinase inhibitor crenolanib for GISTs harboring the imatinib-resistant PDGFRA D842V mutation. There are also studies utilizing checkpoint inhibitors alone or in combination with imatinib.
Case Conclusion
Given the patient’s progression on imatinib, he is started on second-line sunitinib malate. He experiences grade 1 fatigue and hand-foot syndrome, which are managed supportively. After he has been on sunitinib for approximately 8 months, his disease progresses. He subsequently undergoes genomic profiling of his tumor and starts BLU-285 on a clinical trial.
Key Points
- For advanced and metastatic disease, TKIs have substantially improved the prognosis of KIT mutated GISTs, with 3 FDA-approved drugs: imatinib, sunitinib, and regorafenib. Imatinib 400 mg is the standard-of-care frontline therapy for locally advanced, unresectable, or metastatic imatinib-sensitive GISTs. If a patient has a KIT exon 9 mutation and 400 mg is well-tolerated, increasing to 800 mg is recommended. Imatinib should be continued indefinitely unless there is intolerance, a specific patient request for interruption, or progression of disease.
- When there is progression of disease in a patient with a sensitive mutation on 400 mg of imatinib, the dose can be increased to 800 mg.
- For patients who are imatinib-intolerant or have progression, standard second line is sunitinib.
- For patients who further progress or are sunitinib-intolerant, regorafenib is the standard third-line treatment.
- There needs to be close attention to side effects, drug and food interactions, and patient copay costs in order to maintain patient compliance while on TKI therapy.
- There are still major limitations in the systemic treatment of GISTs marked by their inherent genetic heterogeneity and secondary resistance. Continued translational and clinical research is needed in order to improve treatment for patients who develop secondary resistance or who have less common primary resistant mutations. Patients are encouraged to participate in clinical trials of new therapies.
Summary
GISTs are the most common mesenchymal tumors of the GI tract. They comprise an expanding landscape of tumors that are heterogenous in terms of natural history, mutations, and response to systemic treatments. The mainstay of treatment for localized GISTs is surgical resection followed by at least 3-years of adjuvant imatinib for patients with high-risk features who are imatinib-sensitive. Patients with GISTs harboring resistance mutations such as PDGFRA D842V or with SDH-deficient or NF1-associated GISTs should not receive adjuvant imatinib. Patients with more advanced GISTs and/or in difficult to resect sites harboring a sensitive mutation can be considered for neoadjuvant imatinib. Those with metastatic GISTs can receive first-, second-, and third-line imatinib, sunitinib, or regorafenib, respectively. Clinical trial enrollment should be encouraged for patients whose GISTs harbor primary imatinib-resistant mutations, and those with advanced or unresectable GISTs with secondary resistance.
1. Ma GL, Murphy JD, Martinez ME et al. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiol Biomarkers Prev. 2015;24:298-302.
2. Heinrich MC, Rankin C, Blanke CD, et al. Correlation of long-term results of imatinib in advanced gastrointestinal stromal tumors with next-generation sequencing results: analysis of phase 3 SWOG Intergroup Trial S0033. JAMA Oncol. 2017;3:944-952.
3. DeMatteo RP, Lewis JJ, Leung D, et al. Two hundred gastrointestinal stromal tumors recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51-58.
4. Goss GA, Merriam P, Manola J, et al. Clinical and pathological characteristics of gastrointestinal stromal tumors (GIST). Prog Proc Am Soc Clin Oncol. 2000;19:599a.
5. Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002; 347:472-480.
6. Blanke CD, Demetri GD, von Mehren M, et al. Long-term results from a randomized phase ii trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008;26:620-625.
7. Verweij J, van Oosterom A, Blay JY, et al. Imatinib mesylate (STI-571 Glivec, Gleevac) is an active agent for gastrointestinal stromal tumours, but does not yield responses in other soft-tissue sarcomas that are unselected for a molecular target. Results from an EORTC Soft Tissue and Bone Sarcoma Group phase II study. Eur J Cancer. 2003;39:2006-2011.
8. Verweij J, Casali PG, Zalcberg J, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomized trial. Lancet. 2004;364:1127-1134.
9. Blanke CD, Rankin C, Demetri GD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26:626-632.
10. Gastrointestinal Stromal Tumor Meta-Analysis Group (MetaGIST). Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1,640 patients. J Clin Oncol. 2010;28:1247-1253.
11. Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer –a GERCOR study. J Clin Oncol. 2006;24:394-400.
12. Blay JV, Cesne AL, Ray-Coquard I, et al. Prospective multicentric randomized phase iii study of imatinib in patients with advanced gastrointestinal stromal tumors comparing interruption versus continuation of treatment beyond 1 year: The French Sarcoma Group. J Clin Oncol. 2007;25:1107-1113.
13. Desai J, Shankar S, Heinrich MC, et al. Clonal evolution of resistance to imatinib in patients with metastatic gastrointestinal stromal tumors. Clin Cancer Res. 2007;13(18 Pt 1): 5398-5405.
14. Gramza AW, Corless CL, Heinrich MC. Resistance to tyrosine kinase inhibitors in gastrointestinal stromal tumors. Clin Cancer Res. 2009;15:7510-7518.
15. Sutent (sunitinib malate) [package insert]. New York, NY: Pfizer Labs; 2017.
16. Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomized controlled trial. Lancet. 2006;368:1329-1338.
17. George S, Blay JY, Casali PG, et al. Clinical evaluation of continuous daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib failure. Eur J Cancer. 2009;45:1959-1968.
18. Brennan MF, Antonescu CR, Maki RG. Management of Soft Tissue Sarcomas. Switzerland: Springer International Publishing; 2013.
19. Heinrich MC, Maki RG, Corless CL, et al. Primary and secondary kinase genotypes correlate with the biological and clinical activity of sunitinib in imatinib-resistant gastrointestinal stromal tumors. J Clin Oncol. 2008;26:5352-5359.
20. Demetri GD, Reichardt P, Kang YK, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295-302.
21. Wilky BA, Villalobos VM. Emerging role for precision therapy through next-generation sequencing for sarcomas. JCO Precision Oncology. 2018;2:1-4.
22. Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in trk fusion-positive cancers in adults and children. N Engl J Med. 2018;378:731-739.
Most advanced gastrointestinal stromal tumors (GISTs) are due to a recurrence of localized disease, with only a small minority presenting with metastatic disease.1 Compared with chemotherapy, tyrosine kinase inhibitors (TKIs) have significantly improved the natural history of the disease, with median overall survival (OS) increasing from less than 1 year to about 5 years and approximately 1 in 5 patients achieving long-term survival.2 In addition, newer drugs in development and in clinical trials appear promising and have the potential to improve outcomes even further. This article reviews current evidence on options for treating metastatic or recurrent GISTs and GISTs that have progressed following initial therapy. The evaluation and diagnosis of GIST along with management of localized disease are reviewed in a separate article.
Case Presentation
A 64-year-old African American man underwent surgical resection of a 10-cm gastric mass, which pathology reported was positive for CD117, DOG1, and CD34 and negative for smooth muscle actin and S-100, consistent with a diagnosis of GIST. There were 10 mitoses per 50 HPF, and there was no intraoperative or intraperitoneal tumor rupture. The patient was treated with adjuvant imatinib, which was discontinued after 3 years due to grade 2 myalgias, periorbital edema, and macrocytic anemia. Surveillance included office visits every 3 to 6 months and a contrast CT abdomen and pelvis every 6 months. For the past 5 years, he has not had any clinical or radiographic evidence of disease recurrence. New imaging reveals multiple liver metastases and peritoneal implants. He feels fatigued and has lost about 10 lb since his last visit. He is 5 years out from his initial diagnosis and 2 years out from last receiving imatinib. His original tumor harbored a KIT exon 11 deletion.
What treatment should you recommend now?
Imatinib for Advanced GISTs
Before the first report of the efficacy of imatinib for metastatic GISTs in 2002, patients with advanced unresectable or metastatic GISTs were routinely treated with doxorubicin-based chemotherapy regimens, which were largely ineffective, with response rates (RRs) of around 5% and a median overall survival (OS) of less than 1 year.3,4 In 2002 a landmark phase 2 study revealed imatinib’s significant efficacy profile in advanced or metastatic GISTs, resulting in its approval by the US Food and Drug Administration (FDA).5 In this study, 147 patients with CD117-positive GISTs were randomly assigned to receive daily imatinib 400 mg or 600 mg for up to 36 months. The RRs were similar between the 2 groups (68.5% vs 67.6%), with a median time to response of 12 weeks and median duration of response of 118 days. Results of this study were much more favorable when compared to doxorubicin, rendering imatinib the new standard of care for advanced GISTs. A long-term follow-up of this study after a median of 63 months confirmed near identical RRs, progression-free survival (PFS), and median survival of 57 months among the 2 groups.6
Imatinib Daily Dosing
Although 400 mg of daily imatinib proved to be efficacious, it was unclear if a dose-response relationship existed for imatinib. An EORTC phase 2 study demonstrated a benefit of using a higher dose of imatinib at 400 mg twice daily, producing a RR of 71% (4% complete , 67% partial) and 1-year PFS of 73%, which appeared favorable compared with once-daily dosing and set the framework for larger phase 3 studies.7 Two phase 3 studies compared imatinib 400 mg once daily versus twice daily (until disease progression or unacceptable toxicity) among patients with CD117-positive advanced or metastatic GISTs. These studies were eventually combined into a meta-analysis (metaGIST) to compare RR, PFS and OS between the treatment groups. Both studies allowed cross-over to the 800 mg dose for patients who progressed on 400 mg daily.
The first study, conducted jointly by the EORTC, Italian Sarcoma Group, and Australasian Gastro-Intestinal Trials Group (EU-AUS),8 randomly assigned 946 patients to 400 mg once daily or twice daily. There were no differences in response rates between the groups, but the twice-daily group had a predicted 18% reduction in the hazard for progression compared with the once-daily group (estimated HR, 0.82; P = 0.026), which came at the expense of greater toxicities warranting dose reductions (60%) and treatment interruptions (64%). Cross-over to high-dose imatinib was feasible and safe, producing a partial response in 2%, stable disease in 27%, and a median PFS of 81 days. The second study was an intergroup study conducted jointly by SWOG, CALGB, NCI-C, and ECOG (S0033, US-CDN), with a nearly identical study design as the EU-AUS trial.9 The trial enrolled 746 patients. After a median follow up of 4.5 years, the median PFS and OS were not statistically different (18 vs 20 months and 55 vs 51 months, respectively). There were also no differences in response rates. One third of patients initially placed on the once-daily arm who crossed over after progression achieved a treatment response or stable disease.
The combined EU-AUS and US-CDN analysis (metaGIST) included 1640 patients with a median age of 60 years and 58% of whom were men; 818 and 822 patients were assigned to the 400 mg and 800 mg total daily doses, respectively.10 The median follow-up was 37.5 months. There were no differences in OS (49 vs 48.7 months), median PFS (18.9 vs 23.2 months), or overall response rates (51.4% vs 53.9%). Patients who had crossed over (n = 347) to the 800 mg total daily dose arm had a 7.7-month average PFS while on the higher daily dose. An analysis was performed on 377 patients in the EU-AUS trial assessing the impact of mutational status on clinical outcomes among imatinib-treated patients. KIT exon 9 activating mutations were found to be a significant independent prognostic factor for death when compared with KIT exon 11 mutations. However, the adverse prognostic value of KIT exon 9 mutations was partially overcome with higher doses of imatinib, as those who received 800 mg total had a significantly better PFS, with a 61% relative risk reduction, than those who received 400 mg. Altogether, it was concluded that imatinib 400 mg once daily should be the standard-of-care first-line treatment for advanced or metastatic GISTs, unless a KIT exon 9 mutation is present, in which case imatinib 800 mg should be considered, if 400 mg is well tolerated. In addition, patients treated with frontline imatinib at 400 mg once daily, if tolerated well, should be considered for imatinib 800 mg upon progression of disease.
Despite there being problems with secondary resistance, significant progress has occurred in the treatment of metastatic disease over a short period of time. Prior to 2000, median OS for patients with metastatic GISTs was 9 months. With the introduction of imatinib and other TKIs, the median OS has increased to 5 years, with an estimated 10-year OS rate of approximately 20%.2
Imatinib Interruption
Since at this point, imatinib was a well-established standard of care for advanced GISTs, it was questioned whether imatinib therapy could be interrupted. At this time, treatment interruption in a stop-and-go fashion was deemed feasible in other metastatic solid tumors such as colorectal cancer (OPTIMOX1).11 The BFR French trial showed that stopping imatinib therapy in patients who had a response or stable disease after 1, 3, or 5 years was generally followed by relatively rapid tumor progression (approximately 50% of patients within 6 months), even when tumors were previously removed.12 Therefore, it is recommended that treatment in the metastatic setting should be continued indefinitely, unless there is disease progression. Hence, unlike with colorectal cancer or chronic myelogenous leukemia, as of now there is no role for imatinib interruption in metastatic GISTs.
Case Continued
The patient is started on imatinib 400 mg daily, and overall he tolerates therapy well. Interval CT imaging reveals a treatment response. Two years later, imaging reveals an increase in the tumor size and density with a new nodule present within a preexisting mass. There are no clinical trials in the area.
What defines tumor progression?
Disease Progression
When GISTs are responding to treatment, on imaging the tumors can become more cystic and less dense but with an increase in size. In addition, tumor progression may not always be associated with increased size—increased density of the tumor or a nodule within a mass that may indicate progression. If CT imaging is equivocal for progression, positron emission tomography (PET) can play a role in identifying true progression. It is critically important that tumor size and density are carefully assessed when performing interval imaging. Of note, radiofrequency ablation, cryotherapy, or chemoembolization can be used for symptomatic liver metastases or oligometastatic disease. When evaluating for progression, one needs to ask patients about compliance (ie, maintaining dose intensity related to side effects of therapy as well as the financial burden of treatment—copay toxicity).
What are mechanisms of secondary imatinib resistance?
Imatinib resistance can be subtle in patients with GISTs, manifesting with new nodular, enhancing foci enclosed within a preexisting mass (resistant clonal nodule), or can be clinically or radiographically overt.13 Imatinib resistance occurs through multiple mechanisms including acquisition of secondary activating KIT mutations in the intracellular ATP-binding domain (exons 13 and 14) and the activation loop (exons 17 and 18).14
What are the treatment options for this patient?
Second-line Therapy
Sunitinib malate is a multitargeted TKI that not only targets c-Kit and PDGFRA, but also has anti-angiogenic activity through inhibition of vascular endothelial growth factor receptors (VEGFR). Sunitinib gained FDA approval for the second-line treatment of advanced GISTs based on an international double-blind trial that randomized 312 patients with imatinib-resistant metastatic GISTs in a 2:1 fashion to receive sunitinib 50 mg daily for 4 weeks on and 2 weeks off or placebo.15,16 The trial was unblinded early at the planned interim analysis, which revealed a marked benefit, producing a 66% reduction in the hazard risk of progression (27.3 vs 6.4 weeks, HR, 0.33; P < 0.001). The most common treatment-related adverse events were fatigue, diarrhea, skin discoloration, nausea, and hand-foot syndrome. Another open-label phase 2 study assessed a continuous dosing schema of sunitinib 37.5 mg daily, which has been shown to be effective with less toxicity.17 Among the 60 patients enrolled, the primary endpoint of clinical benefit rate at 24 weeks was reached in 53%, which consisted of 13% partial responses and 40% stable disease. Most toxicities were grade 1 or 2 and easily manageable through standard interventions. This has been recommended as an alternative to the initial scheduled regimen.18 Part of sunitinib’s success is its activity against GISTs harboring secondary KIT exon 13 and 14 mutations, and possibly its anti-angiogenic activity.19 Sunitinib is particularly efficacious among GISTs harboring KIT exon 9 mutations.
Third-line Therapy
Patients who have progressed on prior imatinib and sunitinib can receive third-line regorafenib, a multi-TKI that differs chemically from sorafenib by a fluorouracil group (fluoro-sorafenib). FDA approval of regorafenib was based on the phase 3 GRID (GIST Regorafenib In progressive Disease) multicenter international trial.20 This trial randomly assigned 199 patients in a 2:1 fashion to receive regorafenib 160 mg daily for 21 days out of 28-day cycles plus best supportive care (BSC) versus placebo plus BSC. Cross-over was allowed. Regorafenib significantly reduced the hazard risk of progression by 73% compared with placebo (4.8 vs 0.9 months; HR, 0.27; P < 0.001). There was no difference in OS, which may be because of cross-over (median OS, 17.4 months in both arms). As a result, regorafenib is now considered standard third-line treatment for patients with metastatic GISTs. It has a less favorable toxicity profile than imatinib, with hand-foot syndrome, transaminitis, hypertension and fatigue being the most common treatment toxicities. In order to avoid noncompliance, it is recommended to start at 80 mg and carefully titrate upwards to the 160 mg dose.
A list of landmark studies for advanced GISTs is provided in Table 1.
A summary of FDA-approved drugs for treating GISTs is provided in Table 2.
Clinical Trials
Clinical trial enrollment should be considered for all patients with advanced or unresectable GISTs throughout their treatment continuum. Owing to significant advances in genomic profiling through next-generation sequencing, multiple driver mutations have recently been identified, and targeted therapies are being explored in clinical trials.21 For example, the neurotrophic receptor tyrosine kinase (NTRK) gene appears to be mutated in a small number of advanced GISTs, and these can respond to the highly selective TRK inhibitor larotrectinib.22 Additionally, ongoing studies are assessing immunotherapies for sporadic GISTs and treatment for familial GISTs (Table 3). Some notable studies include those assessing the efficacy of agents that target KIT and PDGFR secondary mutations, including avapritinib (BLU-285) and DCC-2618, MEK inhibitors, and the multi-kinase inhibitor crenolanib for GISTs harboring the imatinib-resistant PDGFRA D842V mutation. There are also studies utilizing checkpoint inhibitors alone or in combination with imatinib.
Case Conclusion
Given the patient’s progression on imatinib, he is started on second-line sunitinib malate. He experiences grade 1 fatigue and hand-foot syndrome, which are managed supportively. After he has been on sunitinib for approximately 8 months, his disease progresses. He subsequently undergoes genomic profiling of his tumor and starts BLU-285 on a clinical trial.
Key Points
- For advanced and metastatic disease, TKIs have substantially improved the prognosis of KIT mutated GISTs, with 3 FDA-approved drugs: imatinib, sunitinib, and regorafenib. Imatinib 400 mg is the standard-of-care frontline therapy for locally advanced, unresectable, or metastatic imatinib-sensitive GISTs. If a patient has a KIT exon 9 mutation and 400 mg is well-tolerated, increasing to 800 mg is recommended. Imatinib should be continued indefinitely unless there is intolerance, a specific patient request for interruption, or progression of disease.
- When there is progression of disease in a patient with a sensitive mutation on 400 mg of imatinib, the dose can be increased to 800 mg.
- For patients who are imatinib-intolerant or have progression, standard second line is sunitinib.
- For patients who further progress or are sunitinib-intolerant, regorafenib is the standard third-line treatment.
- There needs to be close attention to side effects, drug and food interactions, and patient copay costs in order to maintain patient compliance while on TKI therapy.
- There are still major limitations in the systemic treatment of GISTs marked by their inherent genetic heterogeneity and secondary resistance. Continued translational and clinical research is needed in order to improve treatment for patients who develop secondary resistance or who have less common primary resistant mutations. Patients are encouraged to participate in clinical trials of new therapies.
Summary
GISTs are the most common mesenchymal tumors of the GI tract. They comprise an expanding landscape of tumors that are heterogenous in terms of natural history, mutations, and response to systemic treatments. The mainstay of treatment for localized GISTs is surgical resection followed by at least 3-years of adjuvant imatinib for patients with high-risk features who are imatinib-sensitive. Patients with GISTs harboring resistance mutations such as PDGFRA D842V or with SDH-deficient or NF1-associated GISTs should not receive adjuvant imatinib. Patients with more advanced GISTs and/or in difficult to resect sites harboring a sensitive mutation can be considered for neoadjuvant imatinib. Those with metastatic GISTs can receive first-, second-, and third-line imatinib, sunitinib, or regorafenib, respectively. Clinical trial enrollment should be encouraged for patients whose GISTs harbor primary imatinib-resistant mutations, and those with advanced or unresectable GISTs with secondary resistance.
Most advanced gastrointestinal stromal tumors (GISTs) are due to a recurrence of localized disease, with only a small minority presenting with metastatic disease.1 Compared with chemotherapy, tyrosine kinase inhibitors (TKIs) have significantly improved the natural history of the disease, with median overall survival (OS) increasing from less than 1 year to about 5 years and approximately 1 in 5 patients achieving long-term survival.2 In addition, newer drugs in development and in clinical trials appear promising and have the potential to improve outcomes even further. This article reviews current evidence on options for treating metastatic or recurrent GISTs and GISTs that have progressed following initial therapy. The evaluation and diagnosis of GIST along with management of localized disease are reviewed in a separate article.
Case Presentation
A 64-year-old African American man underwent surgical resection of a 10-cm gastric mass, which pathology reported was positive for CD117, DOG1, and CD34 and negative for smooth muscle actin and S-100, consistent with a diagnosis of GIST. There were 10 mitoses per 50 HPF, and there was no intraoperative or intraperitoneal tumor rupture. The patient was treated with adjuvant imatinib, which was discontinued after 3 years due to grade 2 myalgias, periorbital edema, and macrocytic anemia. Surveillance included office visits every 3 to 6 months and a contrast CT abdomen and pelvis every 6 months. For the past 5 years, he has not had any clinical or radiographic evidence of disease recurrence. New imaging reveals multiple liver metastases and peritoneal implants. He feels fatigued and has lost about 10 lb since his last visit. He is 5 years out from his initial diagnosis and 2 years out from last receiving imatinib. His original tumor harbored a KIT exon 11 deletion.
What treatment should you recommend now?
Imatinib for Advanced GISTs
Before the first report of the efficacy of imatinib for metastatic GISTs in 2002, patients with advanced unresectable or metastatic GISTs were routinely treated with doxorubicin-based chemotherapy regimens, which were largely ineffective, with response rates (RRs) of around 5% and a median overall survival (OS) of less than 1 year.3,4 In 2002 a landmark phase 2 study revealed imatinib’s significant efficacy profile in advanced or metastatic GISTs, resulting in its approval by the US Food and Drug Administration (FDA).5 In this study, 147 patients with CD117-positive GISTs were randomly assigned to receive daily imatinib 400 mg or 600 mg for up to 36 months. The RRs were similar between the 2 groups (68.5% vs 67.6%), with a median time to response of 12 weeks and median duration of response of 118 days. Results of this study were much more favorable when compared to doxorubicin, rendering imatinib the new standard of care for advanced GISTs. A long-term follow-up of this study after a median of 63 months confirmed near identical RRs, progression-free survival (PFS), and median survival of 57 months among the 2 groups.6
Imatinib Daily Dosing
Although 400 mg of daily imatinib proved to be efficacious, it was unclear if a dose-response relationship existed for imatinib. An EORTC phase 2 study demonstrated a benefit of using a higher dose of imatinib at 400 mg twice daily, producing a RR of 71% (4% complete , 67% partial) and 1-year PFS of 73%, which appeared favorable compared with once-daily dosing and set the framework for larger phase 3 studies.7 Two phase 3 studies compared imatinib 400 mg once daily versus twice daily (until disease progression or unacceptable toxicity) among patients with CD117-positive advanced or metastatic GISTs. These studies were eventually combined into a meta-analysis (metaGIST) to compare RR, PFS and OS between the treatment groups. Both studies allowed cross-over to the 800 mg dose for patients who progressed on 400 mg daily.
The first study, conducted jointly by the EORTC, Italian Sarcoma Group, and Australasian Gastro-Intestinal Trials Group (EU-AUS),8 randomly assigned 946 patients to 400 mg once daily or twice daily. There were no differences in response rates between the groups, but the twice-daily group had a predicted 18% reduction in the hazard for progression compared with the once-daily group (estimated HR, 0.82; P = 0.026), which came at the expense of greater toxicities warranting dose reductions (60%) and treatment interruptions (64%). Cross-over to high-dose imatinib was feasible and safe, producing a partial response in 2%, stable disease in 27%, and a median PFS of 81 days. The second study was an intergroup study conducted jointly by SWOG, CALGB, NCI-C, and ECOG (S0033, US-CDN), with a nearly identical study design as the EU-AUS trial.9 The trial enrolled 746 patients. After a median follow up of 4.5 years, the median PFS and OS were not statistically different (18 vs 20 months and 55 vs 51 months, respectively). There were also no differences in response rates. One third of patients initially placed on the once-daily arm who crossed over after progression achieved a treatment response or stable disease.
The combined EU-AUS and US-CDN analysis (metaGIST) included 1640 patients with a median age of 60 years and 58% of whom were men; 818 and 822 patients were assigned to the 400 mg and 800 mg total daily doses, respectively.10 The median follow-up was 37.5 months. There were no differences in OS (49 vs 48.7 months), median PFS (18.9 vs 23.2 months), or overall response rates (51.4% vs 53.9%). Patients who had crossed over (n = 347) to the 800 mg total daily dose arm had a 7.7-month average PFS while on the higher daily dose. An analysis was performed on 377 patients in the EU-AUS trial assessing the impact of mutational status on clinical outcomes among imatinib-treated patients. KIT exon 9 activating mutations were found to be a significant independent prognostic factor for death when compared with KIT exon 11 mutations. However, the adverse prognostic value of KIT exon 9 mutations was partially overcome with higher doses of imatinib, as those who received 800 mg total had a significantly better PFS, with a 61% relative risk reduction, than those who received 400 mg. Altogether, it was concluded that imatinib 400 mg once daily should be the standard-of-care first-line treatment for advanced or metastatic GISTs, unless a KIT exon 9 mutation is present, in which case imatinib 800 mg should be considered, if 400 mg is well tolerated. In addition, patients treated with frontline imatinib at 400 mg once daily, if tolerated well, should be considered for imatinib 800 mg upon progression of disease.
Despite there being problems with secondary resistance, significant progress has occurred in the treatment of metastatic disease over a short period of time. Prior to 2000, median OS for patients with metastatic GISTs was 9 months. With the introduction of imatinib and other TKIs, the median OS has increased to 5 years, with an estimated 10-year OS rate of approximately 20%.2
Imatinib Interruption
Since at this point, imatinib was a well-established standard of care for advanced GISTs, it was questioned whether imatinib therapy could be interrupted. At this time, treatment interruption in a stop-and-go fashion was deemed feasible in other metastatic solid tumors such as colorectal cancer (OPTIMOX1).11 The BFR French trial showed that stopping imatinib therapy in patients who had a response or stable disease after 1, 3, or 5 years was generally followed by relatively rapid tumor progression (approximately 50% of patients within 6 months), even when tumors were previously removed.12 Therefore, it is recommended that treatment in the metastatic setting should be continued indefinitely, unless there is disease progression. Hence, unlike with colorectal cancer or chronic myelogenous leukemia, as of now there is no role for imatinib interruption in metastatic GISTs.
Case Continued
The patient is started on imatinib 400 mg daily, and overall he tolerates therapy well. Interval CT imaging reveals a treatment response. Two years later, imaging reveals an increase in the tumor size and density with a new nodule present within a preexisting mass. There are no clinical trials in the area.
What defines tumor progression?
Disease Progression
When GISTs are responding to treatment, on imaging the tumors can become more cystic and less dense but with an increase in size. In addition, tumor progression may not always be associated with increased size—increased density of the tumor or a nodule within a mass that may indicate progression. If CT imaging is equivocal for progression, positron emission tomography (PET) can play a role in identifying true progression. It is critically important that tumor size and density are carefully assessed when performing interval imaging. Of note, radiofrequency ablation, cryotherapy, or chemoembolization can be used for symptomatic liver metastases or oligometastatic disease. When evaluating for progression, one needs to ask patients about compliance (ie, maintaining dose intensity related to side effects of therapy as well as the financial burden of treatment—copay toxicity).
What are mechanisms of secondary imatinib resistance?
Imatinib resistance can be subtle in patients with GISTs, manifesting with new nodular, enhancing foci enclosed within a preexisting mass (resistant clonal nodule), or can be clinically or radiographically overt.13 Imatinib resistance occurs through multiple mechanisms including acquisition of secondary activating KIT mutations in the intracellular ATP-binding domain (exons 13 and 14) and the activation loop (exons 17 and 18).14
What are the treatment options for this patient?
Second-line Therapy
Sunitinib malate is a multitargeted TKI that not only targets c-Kit and PDGFRA, but also has anti-angiogenic activity through inhibition of vascular endothelial growth factor receptors (VEGFR). Sunitinib gained FDA approval for the second-line treatment of advanced GISTs based on an international double-blind trial that randomized 312 patients with imatinib-resistant metastatic GISTs in a 2:1 fashion to receive sunitinib 50 mg daily for 4 weeks on and 2 weeks off or placebo.15,16 The trial was unblinded early at the planned interim analysis, which revealed a marked benefit, producing a 66% reduction in the hazard risk of progression (27.3 vs 6.4 weeks, HR, 0.33; P < 0.001). The most common treatment-related adverse events were fatigue, diarrhea, skin discoloration, nausea, and hand-foot syndrome. Another open-label phase 2 study assessed a continuous dosing schema of sunitinib 37.5 mg daily, which has been shown to be effective with less toxicity.17 Among the 60 patients enrolled, the primary endpoint of clinical benefit rate at 24 weeks was reached in 53%, which consisted of 13% partial responses and 40% stable disease. Most toxicities were grade 1 or 2 and easily manageable through standard interventions. This has been recommended as an alternative to the initial scheduled regimen.18 Part of sunitinib’s success is its activity against GISTs harboring secondary KIT exon 13 and 14 mutations, and possibly its anti-angiogenic activity.19 Sunitinib is particularly efficacious among GISTs harboring KIT exon 9 mutations.
Third-line Therapy
Patients who have progressed on prior imatinib and sunitinib can receive third-line regorafenib, a multi-TKI that differs chemically from sorafenib by a fluorouracil group (fluoro-sorafenib). FDA approval of regorafenib was based on the phase 3 GRID (GIST Regorafenib In progressive Disease) multicenter international trial.20 This trial randomly assigned 199 patients in a 2:1 fashion to receive regorafenib 160 mg daily for 21 days out of 28-day cycles plus best supportive care (BSC) versus placebo plus BSC. Cross-over was allowed. Regorafenib significantly reduced the hazard risk of progression by 73% compared with placebo (4.8 vs 0.9 months; HR, 0.27; P < 0.001). There was no difference in OS, which may be because of cross-over (median OS, 17.4 months in both arms). As a result, regorafenib is now considered standard third-line treatment for patients with metastatic GISTs. It has a less favorable toxicity profile than imatinib, with hand-foot syndrome, transaminitis, hypertension and fatigue being the most common treatment toxicities. In order to avoid noncompliance, it is recommended to start at 80 mg and carefully titrate upwards to the 160 mg dose.
A list of landmark studies for advanced GISTs is provided in Table 1.
A summary of FDA-approved drugs for treating GISTs is provided in Table 2.
Clinical Trials
Clinical trial enrollment should be considered for all patients with advanced or unresectable GISTs throughout their treatment continuum. Owing to significant advances in genomic profiling through next-generation sequencing, multiple driver mutations have recently been identified, and targeted therapies are being explored in clinical trials.21 For example, the neurotrophic receptor tyrosine kinase (NTRK) gene appears to be mutated in a small number of advanced GISTs, and these can respond to the highly selective TRK inhibitor larotrectinib.22 Additionally, ongoing studies are assessing immunotherapies for sporadic GISTs and treatment for familial GISTs (Table 3). Some notable studies include those assessing the efficacy of agents that target KIT and PDGFR secondary mutations, including avapritinib (BLU-285) and DCC-2618, MEK inhibitors, and the multi-kinase inhibitor crenolanib for GISTs harboring the imatinib-resistant PDGFRA D842V mutation. There are also studies utilizing checkpoint inhibitors alone or in combination with imatinib.
Case Conclusion
Given the patient’s progression on imatinib, he is started on second-line sunitinib malate. He experiences grade 1 fatigue and hand-foot syndrome, which are managed supportively. After he has been on sunitinib for approximately 8 months, his disease progresses. He subsequently undergoes genomic profiling of his tumor and starts BLU-285 on a clinical trial.
Key Points
- For advanced and metastatic disease, TKIs have substantially improved the prognosis of KIT mutated GISTs, with 3 FDA-approved drugs: imatinib, sunitinib, and regorafenib. Imatinib 400 mg is the standard-of-care frontline therapy for locally advanced, unresectable, or metastatic imatinib-sensitive GISTs. If a patient has a KIT exon 9 mutation and 400 mg is well-tolerated, increasing to 800 mg is recommended. Imatinib should be continued indefinitely unless there is intolerance, a specific patient request for interruption, or progression of disease.
- When there is progression of disease in a patient with a sensitive mutation on 400 mg of imatinib, the dose can be increased to 800 mg.
- For patients who are imatinib-intolerant or have progression, standard second line is sunitinib.
- For patients who further progress or are sunitinib-intolerant, regorafenib is the standard third-line treatment.
- There needs to be close attention to side effects, drug and food interactions, and patient copay costs in order to maintain patient compliance while on TKI therapy.
- There are still major limitations in the systemic treatment of GISTs marked by their inherent genetic heterogeneity and secondary resistance. Continued translational and clinical research is needed in order to improve treatment for patients who develop secondary resistance or who have less common primary resistant mutations. Patients are encouraged to participate in clinical trials of new therapies.
Summary
GISTs are the most common mesenchymal tumors of the GI tract. They comprise an expanding landscape of tumors that are heterogenous in terms of natural history, mutations, and response to systemic treatments. The mainstay of treatment for localized GISTs is surgical resection followed by at least 3-years of adjuvant imatinib for patients with high-risk features who are imatinib-sensitive. Patients with GISTs harboring resistance mutations such as PDGFRA D842V or with SDH-deficient or NF1-associated GISTs should not receive adjuvant imatinib. Patients with more advanced GISTs and/or in difficult to resect sites harboring a sensitive mutation can be considered for neoadjuvant imatinib. Those with metastatic GISTs can receive first-, second-, and third-line imatinib, sunitinib, or regorafenib, respectively. Clinical trial enrollment should be encouraged for patients whose GISTs harbor primary imatinib-resistant mutations, and those with advanced or unresectable GISTs with secondary resistance.
1. Ma GL, Murphy JD, Martinez ME et al. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiol Biomarkers Prev. 2015;24:298-302.
2. Heinrich MC, Rankin C, Blanke CD, et al. Correlation of long-term results of imatinib in advanced gastrointestinal stromal tumors with next-generation sequencing results: analysis of phase 3 SWOG Intergroup Trial S0033. JAMA Oncol. 2017;3:944-952.
3. DeMatteo RP, Lewis JJ, Leung D, et al. Two hundred gastrointestinal stromal tumors recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51-58.
4. Goss GA, Merriam P, Manola J, et al. Clinical and pathological characteristics of gastrointestinal stromal tumors (GIST). Prog Proc Am Soc Clin Oncol. 2000;19:599a.
5. Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002; 347:472-480.
6. Blanke CD, Demetri GD, von Mehren M, et al. Long-term results from a randomized phase ii trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008;26:620-625.
7. Verweij J, van Oosterom A, Blay JY, et al. Imatinib mesylate (STI-571 Glivec, Gleevac) is an active agent for gastrointestinal stromal tumours, but does not yield responses in other soft-tissue sarcomas that are unselected for a molecular target. Results from an EORTC Soft Tissue and Bone Sarcoma Group phase II study. Eur J Cancer. 2003;39:2006-2011.
8. Verweij J, Casali PG, Zalcberg J, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomized trial. Lancet. 2004;364:1127-1134.
9. Blanke CD, Rankin C, Demetri GD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26:626-632.
10. Gastrointestinal Stromal Tumor Meta-Analysis Group (MetaGIST). Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1,640 patients. J Clin Oncol. 2010;28:1247-1253.
11. Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer –a GERCOR study. J Clin Oncol. 2006;24:394-400.
12. Blay JV, Cesne AL, Ray-Coquard I, et al. Prospective multicentric randomized phase iii study of imatinib in patients with advanced gastrointestinal stromal tumors comparing interruption versus continuation of treatment beyond 1 year: The French Sarcoma Group. J Clin Oncol. 2007;25:1107-1113.
13. Desai J, Shankar S, Heinrich MC, et al. Clonal evolution of resistance to imatinib in patients with metastatic gastrointestinal stromal tumors. Clin Cancer Res. 2007;13(18 Pt 1): 5398-5405.
14. Gramza AW, Corless CL, Heinrich MC. Resistance to tyrosine kinase inhibitors in gastrointestinal stromal tumors. Clin Cancer Res. 2009;15:7510-7518.
15. Sutent (sunitinib malate) [package insert]. New York, NY: Pfizer Labs; 2017.
16. Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomized controlled trial. Lancet. 2006;368:1329-1338.
17. George S, Blay JY, Casali PG, et al. Clinical evaluation of continuous daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib failure. Eur J Cancer. 2009;45:1959-1968.
18. Brennan MF, Antonescu CR, Maki RG. Management of Soft Tissue Sarcomas. Switzerland: Springer International Publishing; 2013.
19. Heinrich MC, Maki RG, Corless CL, et al. Primary and secondary kinase genotypes correlate with the biological and clinical activity of sunitinib in imatinib-resistant gastrointestinal stromal tumors. J Clin Oncol. 2008;26:5352-5359.
20. Demetri GD, Reichardt P, Kang YK, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295-302.
21. Wilky BA, Villalobos VM. Emerging role for precision therapy through next-generation sequencing for sarcomas. JCO Precision Oncology. 2018;2:1-4.
22. Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in trk fusion-positive cancers in adults and children. N Engl J Med. 2018;378:731-739.
1. Ma GL, Murphy JD, Martinez ME et al. Epidemiology of gastrointestinal stromal tumors in the era of histology codes: results of a population-based study. Cancer Epidemiol Biomarkers Prev. 2015;24:298-302.
2. Heinrich MC, Rankin C, Blanke CD, et al. Correlation of long-term results of imatinib in advanced gastrointestinal stromal tumors with next-generation sequencing results: analysis of phase 3 SWOG Intergroup Trial S0033. JAMA Oncol. 2017;3:944-952.
3. DeMatteo RP, Lewis JJ, Leung D, et al. Two hundred gastrointestinal stromal tumors recurrence patterns and prognostic factors for survival. Ann Surg. 2000;231:51-58.
4. Goss GA, Merriam P, Manola J, et al. Clinical and pathological characteristics of gastrointestinal stromal tumors (GIST). Prog Proc Am Soc Clin Oncol. 2000;19:599a.
5. Demetri GD, von Mehren M, Blanke CD, et al. Efficacy and safety of imatinib mesylate in advanced gastrointestinal stromal tumors. N Engl J Med. 2002; 347:472-480.
6. Blanke CD, Demetri GD, von Mehren M, et al. Long-term results from a randomized phase ii trial of standard- versus higher-dose imatinib mesylate for patients with unresectable or metastatic gastrointestinal stromal tumors expressing KIT. J Clin Oncol. 2008;26:620-625.
7. Verweij J, van Oosterom A, Blay JY, et al. Imatinib mesylate (STI-571 Glivec, Gleevac) is an active agent for gastrointestinal stromal tumours, but does not yield responses in other soft-tissue sarcomas that are unselected for a molecular target. Results from an EORTC Soft Tissue and Bone Sarcoma Group phase II study. Eur J Cancer. 2003;39:2006-2011.
8. Verweij J, Casali PG, Zalcberg J, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomized trial. Lancet. 2004;364:1127-1134.
9. Blanke CD, Rankin C, Demetri GD, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26:626-632.
10. Gastrointestinal Stromal Tumor Meta-Analysis Group (MetaGIST). Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1,640 patients. J Clin Oncol. 2010;28:1247-1253.
11. Tournigand C, Cervantes A, Figer A, et al. OPTIMOX1: a randomized study of FOLFOX4 or FOLFOX7 with oxaliplatin in a stop-and-Go fashion in advanced colorectal cancer –a GERCOR study. J Clin Oncol. 2006;24:394-400.
12. Blay JV, Cesne AL, Ray-Coquard I, et al. Prospective multicentric randomized phase iii study of imatinib in patients with advanced gastrointestinal stromal tumors comparing interruption versus continuation of treatment beyond 1 year: The French Sarcoma Group. J Clin Oncol. 2007;25:1107-1113.
13. Desai J, Shankar S, Heinrich MC, et al. Clonal evolution of resistance to imatinib in patients with metastatic gastrointestinal stromal tumors. Clin Cancer Res. 2007;13(18 Pt 1): 5398-5405.
14. Gramza AW, Corless CL, Heinrich MC. Resistance to tyrosine kinase inhibitors in gastrointestinal stromal tumors. Clin Cancer Res. 2009;15:7510-7518.
15. Sutent (sunitinib malate) [package insert]. New York, NY: Pfizer Labs; 2017.
16. Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomized controlled trial. Lancet. 2006;368:1329-1338.
17. George S, Blay JY, Casali PG, et al. Clinical evaluation of continuous daily dosing of sunitinib malate in patients with advanced gastrointestinal stromal tumour after imatinib failure. Eur J Cancer. 2009;45:1959-1968.
18. Brennan MF, Antonescu CR, Maki RG. Management of Soft Tissue Sarcomas. Switzerland: Springer International Publishing; 2013.
19. Heinrich MC, Maki RG, Corless CL, et al. Primary and secondary kinase genotypes correlate with the biological and clinical activity of sunitinib in imatinib-resistant gastrointestinal stromal tumors. J Clin Oncol. 2008;26:5352-5359.
20. Demetri GD, Reichardt P, Kang YK, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295-302.
21. Wilky BA, Villalobos VM. Emerging role for precision therapy through next-generation sequencing for sarcomas. JCO Precision Oncology. 2018;2:1-4.
22. Drilon A, Laetsch TW, Kummar S, et al. Efficacy of larotrectinib in trk fusion-positive cancers in adults and children. N Engl J Med. 2018;378:731-739.
Abbott issues recall on Ellipse ICDs
Abbott Laboratories has issued a recall of all Ellipse Implantable Cardioverter Defibrillators manufactured between April 5, 2019, and May 29, 2019, because of exposed aluminum wires within the device, potentially preventing defibrillation.
The Ellipse Implantable Cardioverter Defibrillators, formerly manufactured by St. Jude Medical (now a wholly-owned subsidiary of Abbott), provide pacing for patients with bradycardia and electric shock or pacing for patients with tachycardia. The device is implanted under the skin in the upper chest area with leads running into the heart.
The recall has been issued because electrical failures have occurred; Abbott has determined that these failures are caused by a faulty manufacturing process that left some aluminum wires in the leads partially exposed. Wires without proper insulation are likely to short, leaving the device without the ability to provide high voltage therapy.
Abbott is aware of no related reports of electrical failure in any of the devices that have already been implanted, the Food and Drug Administration announced, and no reports of patient harm, adverse events, or death have occurred. All affected devices that were implanted have either been replaced or are scheduled to be replaced, the agency said.
Abbott Laboratories has issued a recall of all Ellipse Implantable Cardioverter Defibrillators manufactured between April 5, 2019, and May 29, 2019, because of exposed aluminum wires within the device, potentially preventing defibrillation.
The Ellipse Implantable Cardioverter Defibrillators, formerly manufactured by St. Jude Medical (now a wholly-owned subsidiary of Abbott), provide pacing for patients with bradycardia and electric shock or pacing for patients with tachycardia. The device is implanted under the skin in the upper chest area with leads running into the heart.
The recall has been issued because electrical failures have occurred; Abbott has determined that these failures are caused by a faulty manufacturing process that left some aluminum wires in the leads partially exposed. Wires without proper insulation are likely to short, leaving the device without the ability to provide high voltage therapy.
Abbott is aware of no related reports of electrical failure in any of the devices that have already been implanted, the Food and Drug Administration announced, and no reports of patient harm, adverse events, or death have occurred. All affected devices that were implanted have either been replaced or are scheduled to be replaced, the agency said.
Abbott Laboratories has issued a recall of all Ellipse Implantable Cardioverter Defibrillators manufactured between April 5, 2019, and May 29, 2019, because of exposed aluminum wires within the device, potentially preventing defibrillation.
The Ellipse Implantable Cardioverter Defibrillators, formerly manufactured by St. Jude Medical (now a wholly-owned subsidiary of Abbott), provide pacing for patients with bradycardia and electric shock or pacing for patients with tachycardia. The device is implanted under the skin in the upper chest area with leads running into the heart.
The recall has been issued because electrical failures have occurred; Abbott has determined that these failures are caused by a faulty manufacturing process that left some aluminum wires in the leads partially exposed. Wires without proper insulation are likely to short, leaving the device without the ability to provide high voltage therapy.
Abbott is aware of no related reports of electrical failure in any of the devices that have already been implanted, the Food and Drug Administration announced, and no reports of patient harm, adverse events, or death have occurred. All affected devices that were implanted have either been replaced or are scheduled to be replaced, the agency said.
Professional coaching keeps doctors in the game
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
Physicians who receive professional coaching are less emotionally exhausted and less vulnerable to burnout, according to the results of a pilot study.
“This intervention adds to the growing literature of evidence-based approaches to promote physician well-being and should be considered a complementary strategy to be deployed in combination with other organizational approaches to improve system-level drivers of work-related stressors,” wrote Liselotte N. Dyrbye, MD, of the Mayo Clinic in Rochester, Minn., and coauthors in JAMA Internal Medicine.
Dr. Dyrbye and colleagues conducted a randomized pilot study of 88 Mayo Clinic physicians in the departments of medicine, family medicine, and pediatrics. Half (n = 44) received 3.5 hours of sessions facilitated by a professional coach. The other half (n = 44) served as controls. Participants’ well-being – in regard to burnout, quality of life, resilience, job satisfaction, engagement, and meaning at work – was surveyed at baseline and the study’s completion.
Physicians in the coaching group participated in a 1-hour initial telephone session, designed to establish a relationship between the physician and coach, as well as to assess needs, set goals, identify values, and create an action plan. During follow-up sessions, coaches would check in, help plan and set goals, and suggest strategies/changes to incorporate into daily life. Physicians were permitted to ask for support on any issue, but also were expected to see as many patients as their colleagues outside of the study.
After 6 months, physicians in the coaching group saw a significant decrease in emotional exhaustion by a mean of 5.2 points, compared with an increase of 1.5 points in the control group. At 5 months, absolute rates of high emotional exhaustion decreased by 19.5% in the coaching group and increased by 9.8% in the control group and absolute rates of overall burnout decreased by 17.1% in the coaching group and increased by 4.9% in the control group. Quality of life and resilience scores also improved, though there were no notable differences between groups in measures of job satisfaction, engagement, and meaning at work.
The authors noted their study’s limitations, which included a modest sample size and a volunteer group of participants.
In addition, the lower percentage of men in the study – 48 of 88 participants were women – may be a result of factors that deserve further investigation. Finally, burnout rates among volunteers were higher than those among other physicians, suggesting that “the study appealed to those in greatest need of the intervention.”
The study was funded by the Mayo Clinic department of medicine’s Program on Physician Well-Being and the Physician Foundation. Two of the authors – Dr. Dyrbye and Tait D. Shanafelt, MD, of Stanford (Calif.) University – reported being the coinventors of, and receiving royalties for, the Physician Well-Being Index, Medical Student Well-Being Index, Nurse Well-Being Index, and the Well-Being Index.
SOURCE: Dyrbye LN et al. JAMA Intern Med. 2019 Aug 5. doi: 10.1001/jamainternmed.2019.2425.
FROM JAMA INTERNAL MEDICINE
Antiepileptic drug outcomes have remained flat for 3 decades
BANGKOK – Since founding the Epilepsy Unit at Glasgow’s Western Infirmary 37 years ago, Martin J. Brodie, MD, has seen many changes in the field, including the introduction of more than a dozen new antiepileptic drugs (AEDs) in the past 2 decades.
And based upon this vast clinical experience coupled with his leadership of landmark studies, he has a message for his physician colleagues and their epilepsy patients. And it’s not pretty.
“Has the probability of achieving seizure freedom increased significantly in the last 3 decades? Regrettably, the answer is no,” he declared at the International Epilepsy Congress.
“Over all these years, in terms of seizure freedom there has been no real difference in outcome. There’s really quite a long way to go before we can say that we are doing all that well for people,” he said at the congress sponsored by the International League Against Epilepsy.
In the year 2000, he and his coinvestigators published a prospective, longitudinal, observational cohort study of 470 newly diagnosed patients with epilepsy treated at the Western Infirmary during 1982-1997, all with a minimum of 2 years’ follow-up. Sixty-one percent achieved complete freedom from seizures for at least 1 year on monotherapy, and another 3% did so on polytherapy, for a total rate of 64% (N Engl J Med. 2000 Feb 3;342[5]:314-19).
But these were patients who by and large were treated with older AEDs such as carbamazepine, which has since fallen by the wayside because of toxicities. Scottish neurologists now generally turn to lamotrigine (Lamictal), levetiracetam (Spritam), and other, newer AEDs. So Dr. Brodie and his coworkers recently published a follow-up study, this one featuring 30 years of longitudinal follow-up of 1,795 patients newly treated for epilepsy with AEDs, new and old, during 1982-2012. The investigators demonstrated that the seizure-free survival curves over time were virtually superimposable. In the larger, more recent study, remission was achieved in 55% of patients with AED monotherapy and in another 9% with polytherapy, for a total rate of 64%, identical to the rate in the 2000 study, and as was the case in the earlier study, 36% of patients remained uncontrolled (JAMA Neurol. 2018 Mar 1;75[3]:279-86).
“Overall, the way this population behaves, there’s no difference in efficacy and no difference in tolerability whether you’re using old drugs used properly or new drugs used properly,” said Dr. Brodie, professor of neurology at the University of Glasgow (Scotland).
It’s noteworthy that Sir William R. Gowers, the Londoner who has been called the greatest neurologist of all time, reported a 70% seizure-free rate in 1881, while Dr. Brodie and workers achieved a 64% rate in their 30-year study. “It’s interesting that the numbers are so bad, really, I suppose,” Dr. Brodie commented.
How about outcomes in pediatric epilepsy?
Dr. Brodie and coworkers recently published a 30-year prospective cohort study of 332 adolescent epilepsy patients newly diagnosed and treated at the Western Infirmary during 1982-2012. At the end of the study, 67% were seizure-free for at least the past year, a feat accomplished via monotherapy in 83% of cases. The seizure-free rate was 72% in those with generalized epilepsy, significantly better than the 60% figure in those with focal epilepsy. The efficacy rate was 74% with newer AED monotherapy and similar at 77% with monotherapy older drugs. Adverse event rates ranged from a low of 12% with lamotrigine to 56% with topiramate (Topamax), according to the findings published in Epilepsia (2019 Jun;60[6]:1083-90).
Roughly similar outcomes have been reported from Norway in a study of 600 children with epilepsy, median age 7 years, with a median follow-up of 5.8 years that is considerably shorter than that in the Glasgow pediatric study. Overall, 59% of the Norwegian children remained seizure free for at least 1 year, 30% developed drug-resistant epilepsy, and 11% followed an intermediate remitting/relapsing course (Pediatrics. 2018 Jun. doi: 10.1542/peds.2017-4016).
Why the decades of flat pharmacologic outcomes?
The consistently suboptimal seizure-free outcomes obtained over the past 30 years shouldn’t really be surprising, according to Dr. Brodie.
“Although we think we have lots of mechanisms of action and lots of differences between the drugs, they’re arguably all antiseizure drugs and not antiepilepsy drugs. We don’t treat the whale; we treat the spout. We don’t treat what we cannot see; we treat what we can see, which is the seizures, but we’re not influencing the long-term outcome,” the neurologist explained.
The compelling case for early epilepsy surgery
Epilepsy surgery remains underutilized, according to Dr. Brodie and other experts.
The International League Against Epilepsy defines drug-resistant epilepsy as failure to achieve sustained seizure freedom after adequate trials of two tolerated and appropriately chosen and used AED schedules. Dr. Brodie’s work was influential in creating that definition because his data demonstrated the sharply diminishing returns of additional drug trials.
“When do we consider epilepsy surgery? Arguably, the earlier, the better. After two drugs have failed appropriately, I don’t think anybody in this room would argue about that, although people in some of the other rooms might,” he said at the congress.
Influential in his thinking on this score were the impressive results of an early study, the first-ever randomized trial of surgery for epilepsy. In 80 patients with a 21-year history of drug-refractory temporal lobe epilepsy who were randomized to surgery or 1 year of AED therapy, at 1 year of follow-up blinded epileptologists rated 58% of surgically treated patients as free from seizures that impair awareness of self and surroundings, compared with just 8% in the AED group (N Engl J Med. 2001 Aug 2;345[5]:311-8).
“That’s a big outcome, and I’m very keen to ensure that my data continue to drive the push for early surgery,” according to the neurologist.
A Cochrane review of 177 studies totaling more than 16,000 patients concluded that 65% of epilepsy patients had good outcomes following surgery. Prognostic factors associated with better surgical outcomes included complete surgical resection of the epileptogenic focus, the presence of mesial temporal sclerosis, concordance of MRI and EEG findings, and an absence of cortical dysplasia (Cochrane Database Syst Rev. 2019;6:CD010541. doi: 10.1002/14651858.CD010541.pub3).
In addition, a systematic review and meta-analysis by Canadian investigators found that 72% of adults with lesional epilepsy identified by MRI or histopathology were seizure-free after surgery, compared with 36% of those with nonlesional epilepsy. The disparity in outcomes was similar in pediatric epilepsy patients, with seizure freedom after surgery in 74% of those with lesional disease versus 45% with nonlesional epilepsy (Epilepsy Res. 2010 May;89[2-3]:310-8).
Whither are neurostimulatory device therapies headed?
Dr. Brodie was quick to admit that as a pharmacologic researcher, device modalities including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation are outside his area of expertise. But he’s been following developments in the field with interest.
“These device therapies have shown efficacy in short-term randomized trials, but very few patients attain long-term seizure freedom. I think these are largely palliative techniques. I gave up on these techniques a long time ago because I felt it was a very costly way of reducing seizures by a relatively small margin, and really we need to go a little bit further than that. But I know there’s a lot of work going on at the moment,” he said.
Dr. Brodie reported serving on the scientific advisory boards of more than a half dozen pharmaceutical companies.
BANGKOK – Since founding the Epilepsy Unit at Glasgow’s Western Infirmary 37 years ago, Martin J. Brodie, MD, has seen many changes in the field, including the introduction of more than a dozen new antiepileptic drugs (AEDs) in the past 2 decades.
And based upon this vast clinical experience coupled with his leadership of landmark studies, he has a message for his physician colleagues and their epilepsy patients. And it’s not pretty.
“Has the probability of achieving seizure freedom increased significantly in the last 3 decades? Regrettably, the answer is no,” he declared at the International Epilepsy Congress.
“Over all these years, in terms of seizure freedom there has been no real difference in outcome. There’s really quite a long way to go before we can say that we are doing all that well for people,” he said at the congress sponsored by the International League Against Epilepsy.
In the year 2000, he and his coinvestigators published a prospective, longitudinal, observational cohort study of 470 newly diagnosed patients with epilepsy treated at the Western Infirmary during 1982-1997, all with a minimum of 2 years’ follow-up. Sixty-one percent achieved complete freedom from seizures for at least 1 year on monotherapy, and another 3% did so on polytherapy, for a total rate of 64% (N Engl J Med. 2000 Feb 3;342[5]:314-19).
But these were patients who by and large were treated with older AEDs such as carbamazepine, which has since fallen by the wayside because of toxicities. Scottish neurologists now generally turn to lamotrigine (Lamictal), levetiracetam (Spritam), and other, newer AEDs. So Dr. Brodie and his coworkers recently published a follow-up study, this one featuring 30 years of longitudinal follow-up of 1,795 patients newly treated for epilepsy with AEDs, new and old, during 1982-2012. The investigators demonstrated that the seizure-free survival curves over time were virtually superimposable. In the larger, more recent study, remission was achieved in 55% of patients with AED monotherapy and in another 9% with polytherapy, for a total rate of 64%, identical to the rate in the 2000 study, and as was the case in the earlier study, 36% of patients remained uncontrolled (JAMA Neurol. 2018 Mar 1;75[3]:279-86).
“Overall, the way this population behaves, there’s no difference in efficacy and no difference in tolerability whether you’re using old drugs used properly or new drugs used properly,” said Dr. Brodie, professor of neurology at the University of Glasgow (Scotland).
It’s noteworthy that Sir William R. Gowers, the Londoner who has been called the greatest neurologist of all time, reported a 70% seizure-free rate in 1881, while Dr. Brodie and workers achieved a 64% rate in their 30-year study. “It’s interesting that the numbers are so bad, really, I suppose,” Dr. Brodie commented.
How about outcomes in pediatric epilepsy?
Dr. Brodie and coworkers recently published a 30-year prospective cohort study of 332 adolescent epilepsy patients newly diagnosed and treated at the Western Infirmary during 1982-2012. At the end of the study, 67% were seizure-free for at least the past year, a feat accomplished via monotherapy in 83% of cases. The seizure-free rate was 72% in those with generalized epilepsy, significantly better than the 60% figure in those with focal epilepsy. The efficacy rate was 74% with newer AED monotherapy and similar at 77% with monotherapy older drugs. Adverse event rates ranged from a low of 12% with lamotrigine to 56% with topiramate (Topamax), according to the findings published in Epilepsia (2019 Jun;60[6]:1083-90).
Roughly similar outcomes have been reported from Norway in a study of 600 children with epilepsy, median age 7 years, with a median follow-up of 5.8 years that is considerably shorter than that in the Glasgow pediatric study. Overall, 59% of the Norwegian children remained seizure free for at least 1 year, 30% developed drug-resistant epilepsy, and 11% followed an intermediate remitting/relapsing course (Pediatrics. 2018 Jun. doi: 10.1542/peds.2017-4016).
Why the decades of flat pharmacologic outcomes?
The consistently suboptimal seizure-free outcomes obtained over the past 30 years shouldn’t really be surprising, according to Dr. Brodie.
“Although we think we have lots of mechanisms of action and lots of differences between the drugs, they’re arguably all antiseizure drugs and not antiepilepsy drugs. We don’t treat the whale; we treat the spout. We don’t treat what we cannot see; we treat what we can see, which is the seizures, but we’re not influencing the long-term outcome,” the neurologist explained.
The compelling case for early epilepsy surgery
Epilepsy surgery remains underutilized, according to Dr. Brodie and other experts.
The International League Against Epilepsy defines drug-resistant epilepsy as failure to achieve sustained seizure freedom after adequate trials of two tolerated and appropriately chosen and used AED schedules. Dr. Brodie’s work was influential in creating that definition because his data demonstrated the sharply diminishing returns of additional drug trials.
“When do we consider epilepsy surgery? Arguably, the earlier, the better. After two drugs have failed appropriately, I don’t think anybody in this room would argue about that, although people in some of the other rooms might,” he said at the congress.
Influential in his thinking on this score were the impressive results of an early study, the first-ever randomized trial of surgery for epilepsy. In 80 patients with a 21-year history of drug-refractory temporal lobe epilepsy who were randomized to surgery or 1 year of AED therapy, at 1 year of follow-up blinded epileptologists rated 58% of surgically treated patients as free from seizures that impair awareness of self and surroundings, compared with just 8% in the AED group (N Engl J Med. 2001 Aug 2;345[5]:311-8).
“That’s a big outcome, and I’m very keen to ensure that my data continue to drive the push for early surgery,” according to the neurologist.
A Cochrane review of 177 studies totaling more than 16,000 patients concluded that 65% of epilepsy patients had good outcomes following surgery. Prognostic factors associated with better surgical outcomes included complete surgical resection of the epileptogenic focus, the presence of mesial temporal sclerosis, concordance of MRI and EEG findings, and an absence of cortical dysplasia (Cochrane Database Syst Rev. 2019;6:CD010541. doi: 10.1002/14651858.CD010541.pub3).
In addition, a systematic review and meta-analysis by Canadian investigators found that 72% of adults with lesional epilepsy identified by MRI or histopathology were seizure-free after surgery, compared with 36% of those with nonlesional epilepsy. The disparity in outcomes was similar in pediatric epilepsy patients, with seizure freedom after surgery in 74% of those with lesional disease versus 45% with nonlesional epilepsy (Epilepsy Res. 2010 May;89[2-3]:310-8).
Whither are neurostimulatory device therapies headed?
Dr. Brodie was quick to admit that as a pharmacologic researcher, device modalities including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation are outside his area of expertise. But he’s been following developments in the field with interest.
“These device therapies have shown efficacy in short-term randomized trials, but very few patients attain long-term seizure freedom. I think these are largely palliative techniques. I gave up on these techniques a long time ago because I felt it was a very costly way of reducing seizures by a relatively small margin, and really we need to go a little bit further than that. But I know there’s a lot of work going on at the moment,” he said.
Dr. Brodie reported serving on the scientific advisory boards of more than a half dozen pharmaceutical companies.
BANGKOK – Since founding the Epilepsy Unit at Glasgow’s Western Infirmary 37 years ago, Martin J. Brodie, MD, has seen many changes in the field, including the introduction of more than a dozen new antiepileptic drugs (AEDs) in the past 2 decades.
And based upon this vast clinical experience coupled with his leadership of landmark studies, he has a message for his physician colleagues and their epilepsy patients. And it’s not pretty.
“Has the probability of achieving seizure freedom increased significantly in the last 3 decades? Regrettably, the answer is no,” he declared at the International Epilepsy Congress.
“Over all these years, in terms of seizure freedom there has been no real difference in outcome. There’s really quite a long way to go before we can say that we are doing all that well for people,” he said at the congress sponsored by the International League Against Epilepsy.
In the year 2000, he and his coinvestigators published a prospective, longitudinal, observational cohort study of 470 newly diagnosed patients with epilepsy treated at the Western Infirmary during 1982-1997, all with a minimum of 2 years’ follow-up. Sixty-one percent achieved complete freedom from seizures for at least 1 year on monotherapy, and another 3% did so on polytherapy, for a total rate of 64% (N Engl J Med. 2000 Feb 3;342[5]:314-19).
But these were patients who by and large were treated with older AEDs such as carbamazepine, which has since fallen by the wayside because of toxicities. Scottish neurologists now generally turn to lamotrigine (Lamictal), levetiracetam (Spritam), and other, newer AEDs. So Dr. Brodie and his coworkers recently published a follow-up study, this one featuring 30 years of longitudinal follow-up of 1,795 patients newly treated for epilepsy with AEDs, new and old, during 1982-2012. The investigators demonstrated that the seizure-free survival curves over time were virtually superimposable. In the larger, more recent study, remission was achieved in 55% of patients with AED monotherapy and in another 9% with polytherapy, for a total rate of 64%, identical to the rate in the 2000 study, and as was the case in the earlier study, 36% of patients remained uncontrolled (JAMA Neurol. 2018 Mar 1;75[3]:279-86).
“Overall, the way this population behaves, there’s no difference in efficacy and no difference in tolerability whether you’re using old drugs used properly or new drugs used properly,” said Dr. Brodie, professor of neurology at the University of Glasgow (Scotland).
It’s noteworthy that Sir William R. Gowers, the Londoner who has been called the greatest neurologist of all time, reported a 70% seizure-free rate in 1881, while Dr. Brodie and workers achieved a 64% rate in their 30-year study. “It’s interesting that the numbers are so bad, really, I suppose,” Dr. Brodie commented.
How about outcomes in pediatric epilepsy?
Dr. Brodie and coworkers recently published a 30-year prospective cohort study of 332 adolescent epilepsy patients newly diagnosed and treated at the Western Infirmary during 1982-2012. At the end of the study, 67% were seizure-free for at least the past year, a feat accomplished via monotherapy in 83% of cases. The seizure-free rate was 72% in those with generalized epilepsy, significantly better than the 60% figure in those with focal epilepsy. The efficacy rate was 74% with newer AED monotherapy and similar at 77% with monotherapy older drugs. Adverse event rates ranged from a low of 12% with lamotrigine to 56% with topiramate (Topamax), according to the findings published in Epilepsia (2019 Jun;60[6]:1083-90).
Roughly similar outcomes have been reported from Norway in a study of 600 children with epilepsy, median age 7 years, with a median follow-up of 5.8 years that is considerably shorter than that in the Glasgow pediatric study. Overall, 59% of the Norwegian children remained seizure free for at least 1 year, 30% developed drug-resistant epilepsy, and 11% followed an intermediate remitting/relapsing course (Pediatrics. 2018 Jun. doi: 10.1542/peds.2017-4016).
Why the decades of flat pharmacologic outcomes?
The consistently suboptimal seizure-free outcomes obtained over the past 30 years shouldn’t really be surprising, according to Dr. Brodie.
“Although we think we have lots of mechanisms of action and lots of differences between the drugs, they’re arguably all antiseizure drugs and not antiepilepsy drugs. We don’t treat the whale; we treat the spout. We don’t treat what we cannot see; we treat what we can see, which is the seizures, but we’re not influencing the long-term outcome,” the neurologist explained.
The compelling case for early epilepsy surgery
Epilepsy surgery remains underutilized, according to Dr. Brodie and other experts.
The International League Against Epilepsy defines drug-resistant epilepsy as failure to achieve sustained seizure freedom after adequate trials of two tolerated and appropriately chosen and used AED schedules. Dr. Brodie’s work was influential in creating that definition because his data demonstrated the sharply diminishing returns of additional drug trials.
“When do we consider epilepsy surgery? Arguably, the earlier, the better. After two drugs have failed appropriately, I don’t think anybody in this room would argue about that, although people in some of the other rooms might,” he said at the congress.
Influential in his thinking on this score were the impressive results of an early study, the first-ever randomized trial of surgery for epilepsy. In 80 patients with a 21-year history of drug-refractory temporal lobe epilepsy who were randomized to surgery or 1 year of AED therapy, at 1 year of follow-up blinded epileptologists rated 58% of surgically treated patients as free from seizures that impair awareness of self and surroundings, compared with just 8% in the AED group (N Engl J Med. 2001 Aug 2;345[5]:311-8).
“That’s a big outcome, and I’m very keen to ensure that my data continue to drive the push for early surgery,” according to the neurologist.
A Cochrane review of 177 studies totaling more than 16,000 patients concluded that 65% of epilepsy patients had good outcomes following surgery. Prognostic factors associated with better surgical outcomes included complete surgical resection of the epileptogenic focus, the presence of mesial temporal sclerosis, concordance of MRI and EEG findings, and an absence of cortical dysplasia (Cochrane Database Syst Rev. 2019;6:CD010541. doi: 10.1002/14651858.CD010541.pub3).
In addition, a systematic review and meta-analysis by Canadian investigators found that 72% of adults with lesional epilepsy identified by MRI or histopathology were seizure-free after surgery, compared with 36% of those with nonlesional epilepsy. The disparity in outcomes was similar in pediatric epilepsy patients, with seizure freedom after surgery in 74% of those with lesional disease versus 45% with nonlesional epilepsy (Epilepsy Res. 2010 May;89[2-3]:310-8).
Whither are neurostimulatory device therapies headed?
Dr. Brodie was quick to admit that as a pharmacologic researcher, device modalities including vagus nerve stimulation, responsive neurostimulation, and deep brain stimulation are outside his area of expertise. But he’s been following developments in the field with interest.
“These device therapies have shown efficacy in short-term randomized trials, but very few patients attain long-term seizure freedom. I think these are largely palliative techniques. I gave up on these techniques a long time ago because I felt it was a very costly way of reducing seizures by a relatively small margin, and really we need to go a little bit further than that. But I know there’s a lot of work going on at the moment,” he said.
Dr. Brodie reported serving on the scientific advisory boards of more than a half dozen pharmaceutical companies.
EXPERT ANALYSIS FROM IEC 2019
Should You Switch the DAPT Agent a Month After ACS?
A 60-year-old man visits your clinic 30 days after he was hospitalized for acute coronary syndrome (ACS) due to ST-elevation myocardial infarction (STEMI). The patient underwent percutaneous coronary intervention (PCI) with placement of a stent and received aspirin and a loading dose of ticagrelor for antiplatelet therapy. He was discharged on dual antiplatelet therapy (DAPT) consisting of daily aspirin and ticagrelor. He asks about the risk for bleeding associated with these medications. Should you recommend any changes?
Platelet inhibition during and after ACS to prevent recurrent ischemic events is a cornerstone of treatment for patients after a myocardial infarction (MI).2 Current American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommend that patients with coronary artery disease who recently had an MI continue DAPT with aspirin and a P2Y12 blocker (clopidogrel, ticlopidine, ticagrelor, prasugrel, or cangrelor) for 12 months following ACS to reduce recurrent ischemia.2-4
Studies have shown that using the newer P2Y12 inhibitors (prasugrel and ticagrelor) after PCI leads to a significant reduction in recurrent ischemic events, compared with clopidogrel.5-7 These data prompted a guideline change recommending the use of the newer agents over clopidogrel for 12 months following PCI.2 Follow-up studies show strong evidence for the use of the newer P2Y12 agents in the first month following PCI, but they also demonstrate an increased bleeding risk in the maintenance phase (from 30 days to 12 months post-PCI).6,7 This increased risk is the basis for the study by Cuisset et al, which examined switching from a newer P2Y12 agent to clopidogrel after the initial 30-day period following PCI.
STUDY SUMMARY
Switched DAPT is superior
This open-label RCT (N = 646) evaluated changing DAPT from aspirin plus a newer P2Y12 blocker (prasugrel or ticagrelor) to a combination of aspirin and clopidogrel after the first month of DAPT post-ACS.1 Prior to PCI, patients received a loading dose of ticagrelor (180 mg) or prasugrel (60 mg). Subsequently, all patients took aspirin (75 mg/d) and either prasugrel (10 mg/d) or ticagrelor (90 mg bid) for 1 month. After 30 days, participants who had no adverse events were randomly assigned in a 1:1 ratio to continue the aspirin and newer P2Y12 blocker regimen or switch to aspirin and clopidogrel (75 mg/d). In the following year, researchers examined the composite outcome of cardiovascular death, urgent revascularization, stroke, and major bleeding (defined by a Bleeding Academic Research Consortium [BARC] classification ≥ Type 2 at 1-year post-ACS).
Of the participants (average age, 60), 40% had a STEMI and 60% had a non-STEMI. Overall, 43% of patients were prescribed ticagrelor and 57% prasugrel. At 1 year, 86% of the switched-DAPT group and 75% of the unchanged-DAPT group were still taking their medication. The composite outcome at 1-year follow-up was lower in the switched group compared with the unchanged group (13.4% vs 26.3%; hazard ratio [HR], 0.48; 95% confidence interval [CI], 0.34-0.68; number needed to treat [NNT], 8).
Bleeding events (ranging from minimal to fatal) were lower in the switched group (9.3% vs 23.5%; HR, 0.39; 95% CI, 0.27-0.57; NNT, 7) and events identified as BARC ≥ Type 2 (defined as needing medical treatment) were also lower in this group (4% vs 14.9%; HR, 0.30, 95% CI, 0.18-0.50; NNT, 9). There were no significant differences in reported recurrent cardiovascular ischemic events (9.3% vs 11.5%; HR, 0.80, 95% CI, 0.50-1.29).
WHAT’S NEW
Less bleeding, no increase in ischemic events
Cardiology guidelines recommend the newer P2Y12 blockers as part of DAPT after ACS, but this trial showed switching to clopidogrel for DAPT after 30 days of treatment lowers bleeding events with no difference in recurrent ischemic events.2-4
Continue to: CAVEATS
CAVEATS
Less-than-ideal study methods
In this open-label and unblinded study, the investigators adjudicating critical events were blinded to the treatment allocation. However, patients could self-report minor bleeding and medication discontinuation for which no consultation was sought. In addition, the investigators used opaque envelopes—a less-than-ideal method—to conceal allocation at enrollment.
CHALLENGES TO IMPLEMENTATION
PCP may not change cardiologist’s prescription
Implementing this practice is facilitated by the comparatively lower cost of clopidogrel versus the newer P2Y12 blockers. However, after ACS and PCI treatment, cardiologists usually initiate antiplatelet therapy and may continue to manage patients after discharge. The primary care provider (PCP) may not be responsible for the DAPT switch initially; furthermore, ordering a switch may require coordination if the PCP is hesitant to change the cardiologist’s prescription. Lastly, guidelines currently recommend using the newer P2Y12 blockers for 12 months.2 CR
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[3]:162,164).
1. Cuisset T, Deharo P, Quilici J, et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: the TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur Heart J. 2017;38(41):3070-3078.
2. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016;68(10):1082-1115.
3. Steg PG, James SK, Atar D, et al; Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569-2619.
4. Roffi M, Patrono C, Collet J-P, et al; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2015;37(3):267-315.
5. Antman EM, Wiviott SD, Murphy SA, et al. Early and late benefits of prasugrel in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a TRITON-TIMI 38 (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) analysis. J Am Coll Cardiol. 2008;51(21): 2028-2033.
6. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
7. Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001-2015.
A 60-year-old man visits your clinic 30 days after he was hospitalized for acute coronary syndrome (ACS) due to ST-elevation myocardial infarction (STEMI). The patient underwent percutaneous coronary intervention (PCI) with placement of a stent and received aspirin and a loading dose of ticagrelor for antiplatelet therapy. He was discharged on dual antiplatelet therapy (DAPT) consisting of daily aspirin and ticagrelor. He asks about the risk for bleeding associated with these medications. Should you recommend any changes?
Platelet inhibition during and after ACS to prevent recurrent ischemic events is a cornerstone of treatment for patients after a myocardial infarction (MI).2 Current American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommend that patients with coronary artery disease who recently had an MI continue DAPT with aspirin and a P2Y12 blocker (clopidogrel, ticlopidine, ticagrelor, prasugrel, or cangrelor) for 12 months following ACS to reduce recurrent ischemia.2-4
Studies have shown that using the newer P2Y12 inhibitors (prasugrel and ticagrelor) after PCI leads to a significant reduction in recurrent ischemic events, compared with clopidogrel.5-7 These data prompted a guideline change recommending the use of the newer agents over clopidogrel for 12 months following PCI.2 Follow-up studies show strong evidence for the use of the newer P2Y12 agents in the first month following PCI, but they also demonstrate an increased bleeding risk in the maintenance phase (from 30 days to 12 months post-PCI).6,7 This increased risk is the basis for the study by Cuisset et al, which examined switching from a newer P2Y12 agent to clopidogrel after the initial 30-day period following PCI.
STUDY SUMMARY
Switched DAPT is superior
This open-label RCT (N = 646) evaluated changing DAPT from aspirin plus a newer P2Y12 blocker (prasugrel or ticagrelor) to a combination of aspirin and clopidogrel after the first month of DAPT post-ACS.1 Prior to PCI, patients received a loading dose of ticagrelor (180 mg) or prasugrel (60 mg). Subsequently, all patients took aspirin (75 mg/d) and either prasugrel (10 mg/d) or ticagrelor (90 mg bid) for 1 month. After 30 days, participants who had no adverse events were randomly assigned in a 1:1 ratio to continue the aspirin and newer P2Y12 blocker regimen or switch to aspirin and clopidogrel (75 mg/d). In the following year, researchers examined the composite outcome of cardiovascular death, urgent revascularization, stroke, and major bleeding (defined by a Bleeding Academic Research Consortium [BARC] classification ≥ Type 2 at 1-year post-ACS).
Of the participants (average age, 60), 40% had a STEMI and 60% had a non-STEMI. Overall, 43% of patients were prescribed ticagrelor and 57% prasugrel. At 1 year, 86% of the switched-DAPT group and 75% of the unchanged-DAPT group were still taking their medication. The composite outcome at 1-year follow-up was lower in the switched group compared with the unchanged group (13.4% vs 26.3%; hazard ratio [HR], 0.48; 95% confidence interval [CI], 0.34-0.68; number needed to treat [NNT], 8).
Bleeding events (ranging from minimal to fatal) were lower in the switched group (9.3% vs 23.5%; HR, 0.39; 95% CI, 0.27-0.57; NNT, 7) and events identified as BARC ≥ Type 2 (defined as needing medical treatment) were also lower in this group (4% vs 14.9%; HR, 0.30, 95% CI, 0.18-0.50; NNT, 9). There were no significant differences in reported recurrent cardiovascular ischemic events (9.3% vs 11.5%; HR, 0.80, 95% CI, 0.50-1.29).
WHAT’S NEW
Less bleeding, no increase in ischemic events
Cardiology guidelines recommend the newer P2Y12 blockers as part of DAPT after ACS, but this trial showed switching to clopidogrel for DAPT after 30 days of treatment lowers bleeding events with no difference in recurrent ischemic events.2-4
Continue to: CAVEATS
CAVEATS
Less-than-ideal study methods
In this open-label and unblinded study, the investigators adjudicating critical events were blinded to the treatment allocation. However, patients could self-report minor bleeding and medication discontinuation for which no consultation was sought. In addition, the investigators used opaque envelopes—a less-than-ideal method—to conceal allocation at enrollment.
CHALLENGES TO IMPLEMENTATION
PCP may not change cardiologist’s prescription
Implementing this practice is facilitated by the comparatively lower cost of clopidogrel versus the newer P2Y12 blockers. However, after ACS and PCI treatment, cardiologists usually initiate antiplatelet therapy and may continue to manage patients after discharge. The primary care provider (PCP) may not be responsible for the DAPT switch initially; furthermore, ordering a switch may require coordination if the PCP is hesitant to change the cardiologist’s prescription. Lastly, guidelines currently recommend using the newer P2Y12 blockers for 12 months.2 CR
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[3]:162,164).
A 60-year-old man visits your clinic 30 days after he was hospitalized for acute coronary syndrome (ACS) due to ST-elevation myocardial infarction (STEMI). The patient underwent percutaneous coronary intervention (PCI) with placement of a stent and received aspirin and a loading dose of ticagrelor for antiplatelet therapy. He was discharged on dual antiplatelet therapy (DAPT) consisting of daily aspirin and ticagrelor. He asks about the risk for bleeding associated with these medications. Should you recommend any changes?
Platelet inhibition during and after ACS to prevent recurrent ischemic events is a cornerstone of treatment for patients after a myocardial infarction (MI).2 Current American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommend that patients with coronary artery disease who recently had an MI continue DAPT with aspirin and a P2Y12 blocker (clopidogrel, ticlopidine, ticagrelor, prasugrel, or cangrelor) for 12 months following ACS to reduce recurrent ischemia.2-4
Studies have shown that using the newer P2Y12 inhibitors (prasugrel and ticagrelor) after PCI leads to a significant reduction in recurrent ischemic events, compared with clopidogrel.5-7 These data prompted a guideline change recommending the use of the newer agents over clopidogrel for 12 months following PCI.2 Follow-up studies show strong evidence for the use of the newer P2Y12 agents in the first month following PCI, but they also demonstrate an increased bleeding risk in the maintenance phase (from 30 days to 12 months post-PCI).6,7 This increased risk is the basis for the study by Cuisset et al, which examined switching from a newer P2Y12 agent to clopidogrel after the initial 30-day period following PCI.
STUDY SUMMARY
Switched DAPT is superior
This open-label RCT (N = 646) evaluated changing DAPT from aspirin plus a newer P2Y12 blocker (prasugrel or ticagrelor) to a combination of aspirin and clopidogrel after the first month of DAPT post-ACS.1 Prior to PCI, patients received a loading dose of ticagrelor (180 mg) or prasugrel (60 mg). Subsequently, all patients took aspirin (75 mg/d) and either prasugrel (10 mg/d) or ticagrelor (90 mg bid) for 1 month. After 30 days, participants who had no adverse events were randomly assigned in a 1:1 ratio to continue the aspirin and newer P2Y12 blocker regimen or switch to aspirin and clopidogrel (75 mg/d). In the following year, researchers examined the composite outcome of cardiovascular death, urgent revascularization, stroke, and major bleeding (defined by a Bleeding Academic Research Consortium [BARC] classification ≥ Type 2 at 1-year post-ACS).
Of the participants (average age, 60), 40% had a STEMI and 60% had a non-STEMI. Overall, 43% of patients were prescribed ticagrelor and 57% prasugrel. At 1 year, 86% of the switched-DAPT group and 75% of the unchanged-DAPT group were still taking their medication. The composite outcome at 1-year follow-up was lower in the switched group compared with the unchanged group (13.4% vs 26.3%; hazard ratio [HR], 0.48; 95% confidence interval [CI], 0.34-0.68; number needed to treat [NNT], 8).
Bleeding events (ranging from minimal to fatal) were lower in the switched group (9.3% vs 23.5%; HR, 0.39; 95% CI, 0.27-0.57; NNT, 7) and events identified as BARC ≥ Type 2 (defined as needing medical treatment) were also lower in this group (4% vs 14.9%; HR, 0.30, 95% CI, 0.18-0.50; NNT, 9). There were no significant differences in reported recurrent cardiovascular ischemic events (9.3% vs 11.5%; HR, 0.80, 95% CI, 0.50-1.29).
WHAT’S NEW
Less bleeding, no increase in ischemic events
Cardiology guidelines recommend the newer P2Y12 blockers as part of DAPT after ACS, but this trial showed switching to clopidogrel for DAPT after 30 days of treatment lowers bleeding events with no difference in recurrent ischemic events.2-4
Continue to: CAVEATS
CAVEATS
Less-than-ideal study methods
In this open-label and unblinded study, the investigators adjudicating critical events were blinded to the treatment allocation. However, patients could self-report minor bleeding and medication discontinuation for which no consultation was sought. In addition, the investigators used opaque envelopes—a less-than-ideal method—to conceal allocation at enrollment.
CHALLENGES TO IMPLEMENTATION
PCP may not change cardiologist’s prescription
Implementing this practice is facilitated by the comparatively lower cost of clopidogrel versus the newer P2Y12 blockers. However, after ACS and PCI treatment, cardiologists usually initiate antiplatelet therapy and may continue to manage patients after discharge. The primary care provider (PCP) may not be responsible for the DAPT switch initially; furthermore, ordering a switch may require coordination if the PCP is hesitant to change the cardiologist’s prescription. Lastly, guidelines currently recommend using the newer P2Y12 blockers for 12 months.2 CR
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2019. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquiries Network and The Journal of Family Practice (2019;68[3]:162,164).
1. Cuisset T, Deharo P, Quilici J, et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: the TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur Heart J. 2017;38(41):3070-3078.
2. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016;68(10):1082-1115.
3. Steg PG, James SK, Atar D, et al; Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569-2619.
4. Roffi M, Patrono C, Collet J-P, et al; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2015;37(3):267-315.
5. Antman EM, Wiviott SD, Murphy SA, et al. Early and late benefits of prasugrel in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a TRITON-TIMI 38 (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) analysis. J Am Coll Cardiol. 2008;51(21): 2028-2033.
6. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
7. Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001-2015.
1. Cuisset T, Deharo P, Quilici J, et al. Benefit of switching dual antiplatelet therapy after acute coronary syndrome: the TOPIC (timing of platelet inhibition after acute coronary syndrome) randomized study. Eur Heart J. 2017;38(41):3070-3078.
2. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016;68(10):1082-1115.
3. Steg PG, James SK, Atar D, et al; Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC). ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33(20):2569-2619.
4. Roffi M, Patrono C, Collet J-P, et al; ESC Scientific Document Group. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2015;37(3):267-315.
5. Antman EM, Wiviott SD, Murphy SA, et al. Early and late benefits of prasugrel in patients with acute coronary syndromes undergoing percutaneous coronary intervention: a TRITON-TIMI 38 (TRial to Assess Improvement in Therapeutic Outcomes by Optimizing Platelet InhibitioN with Prasugrel-Thrombolysis In Myocardial Infarction) analysis. J Am Coll Cardiol. 2008;51(21): 2028-2033.
6. Wallentin L, Becker RC, Budaj A, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361(11):1045-1057.
7. Wiviott SD, Braunwald E, McCabe CH, et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357(20):2001-2015.
Benefit of chemo + RT for high-risk endometrial cancer increases with time
Benefits of adding chemotherapy to pelvic radiotherapy in localized high-risk endometrial cancer increase with follow-up, finds an updated analysis of the randomized PORTEC-3 trial.
The relative risk-benefit profile of chemoradiotherapy is uncertain, with some evidence suggesting it varies according to disease histology and stage, noted lead investigator Stephanie de Boer, MD, department of radiation oncology, Leiden (the Netherlands) University Medical Center, and coinvestigators.
PORTEC-3, a multicenter phase 3 trial, enrolled women who had undergone surgery for high-risk endometrial cancer: FIGO 2009 stage I, endometrioid grade 3 cancer with deep myometrial invasion, lymphovascular space invasion, or both; stage II or III disease; or stage I to III disease with serous or clear cell histology. In all, 660 women were evenly assigned to external-beam radiotherapy alone (48.6 Gy in 1.8-Gy fractions, on 5 days per week) or radiotherapy and chemotherapy (two cycles of cisplatin given during radiotherapy, followed by four cycles of carboplatin and paclitaxel).
A previous analysis, at a median follow-up of 60.2 months (5.0 years), showed a significant 5-year failure-free survival benefit of chemoradiotherapy over radiotherapy (hazard ratio [HR], 0.71; P = .022) but only a trend toward an overall survival benefit (Lancet Oncol. 2018;19[3]:295-309).
The updated analysis, now at a median follow-up of 72.6 months (6.1 years), was reported in Lancet Oncology and showed that chemoradiotherapy was still significantly superior to radiotherapy alone in terms of 5-year failure-free survival (76.5% vs. 69.1%; adjusted HR, 0.70; P = .016) but was now also significantly superior in terms of 5-year overall survival (81.4% vs. 76.1%; adjusted HR, 0.70; P = .034)
The 5-year probability of distant metastasis was lower with chemoradiotherapy than with radiotherapy alone (21.4% vs. 29.1%; HR, 0.74; P = .047). The two groups did not differ significantly with respect to isolated vaginal recurrence as first site (0.3% in each group) or isolated pelvic recurrence as first site (0.9% in each group).
Only a single patient, in the chemoradiotherapy group, experienced a grade 4 adverse event (ileus or obstruction). The chemoradiotherapy and radiotherapy-only groups were similar on the rate of grade 3 adverse events (8% vs. 5%; P = .24), the most common of which was hypertension. However, the former had a higher rate of grade 2 or worse adverse events (38% vs. 23%; P = .002), such as persistent sensory neuropathy (6% vs. 0%). None of the patients died from treatment-related causes.
“Combined adjuvant chemotherapy and radiotherapy should be discussed and recommended as a new standard of care, especially for women with stage III endometrial cancer or serous cancers, or both,” Dr. de Boer and coinvestigators maintained. “Shared decision making between doctors and their patients remains essential to weigh the costs and benefits for individual patients.
“Molecular analysis has the potential to improve risk stratification and should be used to identify subgroups that can derive the greatest benefit from chemotherapy and to select patients for targeted therapies; molecular studies on tissue samples donated by PORTEC-3 trial participants are ongoing,” they noted.
Dr. de Boer disclosed no competing interests in relation to the study. The study was supported in part by the Dutch Cancer Society, Cancer Research UK, National Health and Medical Research Council, Cancer Australia, the Italian Medicines Agency, and the Canadian Cancer Society Research Institute.
SOURCE: de Boer SM et al. Lancet Oncol. 2019 July 22. doi: 10.1016/S1470-2045(19)30395-X.
Results of PORTEC-3 are potentially practice changing but generate several questions relevant to optimizing adjuvant therapy for high-risk endometrial cancer, Marcus Randall, MD, contends in a commentary (Lancet Oncol. 2019 Jul 22. doi: 10.1016/S1470-2045[19]30416-4).
One question is applicability of the findings across trial subgroups, which is still uncertain. “However, taking into account the statistical limitations of subgroup analyses, the therapeutic benefit of combined chemotherapy and radiotherapy (vs. radiotherapy alone) appeared to remain confined to patients with stage III disease and those with serous carcinomas of all stages,” he noted.
Another question is whether chemotherapy alone is sufficient. Here, results from trials conducted by the Gynecologic Oncology Group (now NRG Oncology) suggest that omitting pelvic radiotherapy increases the risk of locoregional failure, according to Dr. Randall.
A final question is whether there is a preferred approach for combining chemotherapy with radiotherapy. “Increasing evidence supports the use of upfront systemic therapy, when combined with radiotherapy, as a strategy to maximise both systemic and local control. ... Many clinicians often use this regimen as a preferred adjuvant approach in locally advanced endometrial cancer,” he noted.
“Based on outstanding work done by the PORTEC Study Group and others, we have made good progress in improving outcomes for women with high-risk and locally advanced endometrial cancers. However, we are not there yet,” Dr. Randall concludes.
Marcus Randall, MD, is with the department of radiation medicine, University of Kentucky, Lexington. He has no disclosures related to the commentary.
Results of PORTEC-3 are potentially practice changing but generate several questions relevant to optimizing adjuvant therapy for high-risk endometrial cancer, Marcus Randall, MD, contends in a commentary (Lancet Oncol. 2019 Jul 22. doi: 10.1016/S1470-2045[19]30416-4).
One question is applicability of the findings across trial subgroups, which is still uncertain. “However, taking into account the statistical limitations of subgroup analyses, the therapeutic benefit of combined chemotherapy and radiotherapy (vs. radiotherapy alone) appeared to remain confined to patients with stage III disease and those with serous carcinomas of all stages,” he noted.
Another question is whether chemotherapy alone is sufficient. Here, results from trials conducted by the Gynecologic Oncology Group (now NRG Oncology) suggest that omitting pelvic radiotherapy increases the risk of locoregional failure, according to Dr. Randall.
A final question is whether there is a preferred approach for combining chemotherapy with radiotherapy. “Increasing evidence supports the use of upfront systemic therapy, when combined with radiotherapy, as a strategy to maximise both systemic and local control. ... Many clinicians often use this regimen as a preferred adjuvant approach in locally advanced endometrial cancer,” he noted.
“Based on outstanding work done by the PORTEC Study Group and others, we have made good progress in improving outcomes for women with high-risk and locally advanced endometrial cancers. However, we are not there yet,” Dr. Randall concludes.
Marcus Randall, MD, is with the department of radiation medicine, University of Kentucky, Lexington. He has no disclosures related to the commentary.
Results of PORTEC-3 are potentially practice changing but generate several questions relevant to optimizing adjuvant therapy for high-risk endometrial cancer, Marcus Randall, MD, contends in a commentary (Lancet Oncol. 2019 Jul 22. doi: 10.1016/S1470-2045[19]30416-4).
One question is applicability of the findings across trial subgroups, which is still uncertain. “However, taking into account the statistical limitations of subgroup analyses, the therapeutic benefit of combined chemotherapy and radiotherapy (vs. radiotherapy alone) appeared to remain confined to patients with stage III disease and those with serous carcinomas of all stages,” he noted.
Another question is whether chemotherapy alone is sufficient. Here, results from trials conducted by the Gynecologic Oncology Group (now NRG Oncology) suggest that omitting pelvic radiotherapy increases the risk of locoregional failure, according to Dr. Randall.
A final question is whether there is a preferred approach for combining chemotherapy with radiotherapy. “Increasing evidence supports the use of upfront systemic therapy, when combined with radiotherapy, as a strategy to maximise both systemic and local control. ... Many clinicians often use this regimen as a preferred adjuvant approach in locally advanced endometrial cancer,” he noted.
“Based on outstanding work done by the PORTEC Study Group and others, we have made good progress in improving outcomes for women with high-risk and locally advanced endometrial cancers. However, we are not there yet,” Dr. Randall concludes.
Marcus Randall, MD, is with the department of radiation medicine, University of Kentucky, Lexington. He has no disclosures related to the commentary.
Benefits of adding chemotherapy to pelvic radiotherapy in localized high-risk endometrial cancer increase with follow-up, finds an updated analysis of the randomized PORTEC-3 trial.
The relative risk-benefit profile of chemoradiotherapy is uncertain, with some evidence suggesting it varies according to disease histology and stage, noted lead investigator Stephanie de Boer, MD, department of radiation oncology, Leiden (the Netherlands) University Medical Center, and coinvestigators.
PORTEC-3, a multicenter phase 3 trial, enrolled women who had undergone surgery for high-risk endometrial cancer: FIGO 2009 stage I, endometrioid grade 3 cancer with deep myometrial invasion, lymphovascular space invasion, or both; stage II or III disease; or stage I to III disease with serous or clear cell histology. In all, 660 women were evenly assigned to external-beam radiotherapy alone (48.6 Gy in 1.8-Gy fractions, on 5 days per week) or radiotherapy and chemotherapy (two cycles of cisplatin given during radiotherapy, followed by four cycles of carboplatin and paclitaxel).
A previous analysis, at a median follow-up of 60.2 months (5.0 years), showed a significant 5-year failure-free survival benefit of chemoradiotherapy over radiotherapy (hazard ratio [HR], 0.71; P = .022) but only a trend toward an overall survival benefit (Lancet Oncol. 2018;19[3]:295-309).
The updated analysis, now at a median follow-up of 72.6 months (6.1 years), was reported in Lancet Oncology and showed that chemoradiotherapy was still significantly superior to radiotherapy alone in terms of 5-year failure-free survival (76.5% vs. 69.1%; adjusted HR, 0.70; P = .016) but was now also significantly superior in terms of 5-year overall survival (81.4% vs. 76.1%; adjusted HR, 0.70; P = .034)
The 5-year probability of distant metastasis was lower with chemoradiotherapy than with radiotherapy alone (21.4% vs. 29.1%; HR, 0.74; P = .047). The two groups did not differ significantly with respect to isolated vaginal recurrence as first site (0.3% in each group) or isolated pelvic recurrence as first site (0.9% in each group).
Only a single patient, in the chemoradiotherapy group, experienced a grade 4 adverse event (ileus or obstruction). The chemoradiotherapy and radiotherapy-only groups were similar on the rate of grade 3 adverse events (8% vs. 5%; P = .24), the most common of which was hypertension. However, the former had a higher rate of grade 2 or worse adverse events (38% vs. 23%; P = .002), such as persistent sensory neuropathy (6% vs. 0%). None of the patients died from treatment-related causes.
“Combined adjuvant chemotherapy and radiotherapy should be discussed and recommended as a new standard of care, especially for women with stage III endometrial cancer or serous cancers, or both,” Dr. de Boer and coinvestigators maintained. “Shared decision making between doctors and their patients remains essential to weigh the costs and benefits for individual patients.
“Molecular analysis has the potential to improve risk stratification and should be used to identify subgroups that can derive the greatest benefit from chemotherapy and to select patients for targeted therapies; molecular studies on tissue samples donated by PORTEC-3 trial participants are ongoing,” they noted.
Dr. de Boer disclosed no competing interests in relation to the study. The study was supported in part by the Dutch Cancer Society, Cancer Research UK, National Health and Medical Research Council, Cancer Australia, the Italian Medicines Agency, and the Canadian Cancer Society Research Institute.
SOURCE: de Boer SM et al. Lancet Oncol. 2019 July 22. doi: 10.1016/S1470-2045(19)30395-X.
Benefits of adding chemotherapy to pelvic radiotherapy in localized high-risk endometrial cancer increase with follow-up, finds an updated analysis of the randomized PORTEC-3 trial.
The relative risk-benefit profile of chemoradiotherapy is uncertain, with some evidence suggesting it varies according to disease histology and stage, noted lead investigator Stephanie de Boer, MD, department of radiation oncology, Leiden (the Netherlands) University Medical Center, and coinvestigators.
PORTEC-3, a multicenter phase 3 trial, enrolled women who had undergone surgery for high-risk endometrial cancer: FIGO 2009 stage I, endometrioid grade 3 cancer with deep myometrial invasion, lymphovascular space invasion, or both; stage II or III disease; or stage I to III disease with serous or clear cell histology. In all, 660 women were evenly assigned to external-beam radiotherapy alone (48.6 Gy in 1.8-Gy fractions, on 5 days per week) or radiotherapy and chemotherapy (two cycles of cisplatin given during radiotherapy, followed by four cycles of carboplatin and paclitaxel).
A previous analysis, at a median follow-up of 60.2 months (5.0 years), showed a significant 5-year failure-free survival benefit of chemoradiotherapy over radiotherapy (hazard ratio [HR], 0.71; P = .022) but only a trend toward an overall survival benefit (Lancet Oncol. 2018;19[3]:295-309).
The updated analysis, now at a median follow-up of 72.6 months (6.1 years), was reported in Lancet Oncology and showed that chemoradiotherapy was still significantly superior to radiotherapy alone in terms of 5-year failure-free survival (76.5% vs. 69.1%; adjusted HR, 0.70; P = .016) but was now also significantly superior in terms of 5-year overall survival (81.4% vs. 76.1%; adjusted HR, 0.70; P = .034)
The 5-year probability of distant metastasis was lower with chemoradiotherapy than with radiotherapy alone (21.4% vs. 29.1%; HR, 0.74; P = .047). The two groups did not differ significantly with respect to isolated vaginal recurrence as first site (0.3% in each group) or isolated pelvic recurrence as first site (0.9% in each group).
Only a single patient, in the chemoradiotherapy group, experienced a grade 4 adverse event (ileus or obstruction). The chemoradiotherapy and radiotherapy-only groups were similar on the rate of grade 3 adverse events (8% vs. 5%; P = .24), the most common of which was hypertension. However, the former had a higher rate of grade 2 or worse adverse events (38% vs. 23%; P = .002), such as persistent sensory neuropathy (6% vs. 0%). None of the patients died from treatment-related causes.
“Combined adjuvant chemotherapy and radiotherapy should be discussed and recommended as a new standard of care, especially for women with stage III endometrial cancer or serous cancers, or both,” Dr. de Boer and coinvestigators maintained. “Shared decision making between doctors and their patients remains essential to weigh the costs and benefits for individual patients.
“Molecular analysis has the potential to improve risk stratification and should be used to identify subgroups that can derive the greatest benefit from chemotherapy and to select patients for targeted therapies; molecular studies on tissue samples donated by PORTEC-3 trial participants are ongoing,” they noted.
Dr. de Boer disclosed no competing interests in relation to the study. The study was supported in part by the Dutch Cancer Society, Cancer Research UK, National Health and Medical Research Council, Cancer Australia, the Italian Medicines Agency, and the Canadian Cancer Society Research Institute.
SOURCE: de Boer SM et al. Lancet Oncol. 2019 July 22. doi: 10.1016/S1470-2045(19)30395-X.
FROM LANCET ONCOLOGY
Commentary: Medical educators must do more to prevent physician suicides
while describing two exemplars at providing physicians with mental health support, in a recently published commentary.
“I want to call attention to the gap between what educators think and say is available, in terms of mental health support, and what trainees experience,” Dr. Poorman said in a statement on her piece in the Journal of Patient Safety and Risk Management. She shared the results of an anonymous depression survey of interns, which showed that 41.8% of participants screened positive for depression. Dr. Poorman also provided statistics on physician suicide, including that at least 66 residents killed themselves between 2000 and 2014, according to ACGME, and that another source estimated that 300-400 physician suicide deaths occur annually.
“When it comes to mental illness and suicide, we are all at risk, but we too often lacked compassion in the way we approach our colleagues. We have lacked the courage to fight the stigma that is killing us. We have not asked whether our unwillingness to reform medical training has eroded the empathy of generations of doctors. We have not done enough to fight medical boards that ask doctors about mental health diagnoses in the same way they ask if we have domestic violence charges,” wrote Dr. Poorman, who practices at a University of Washington neighborhood clinic in Kent.
“A focus on the occupational risks we face would shift us away from ‘wellness’ and ‘resilience,’ and place the onus on schools, training programs, and hospitals to do better for providers and patients,” continued Dr. Poorman, who serves on the editorial advisory board of Internal Medicine News.
She commended Oregon Health and Science University, Portland, and Stanford (Calif.) University’s divisions of general surgery for providing “rigorously confidential mental health support” through a wellness and suicide prevention program for residents and faculty, and a wellness program for residents “that emphasizes relationships, structural support, and psychological safety,” respectively. Dr. Poorman also applauded both for speaking openly about physician suicides.
SOURCE: Poorman E. J Patient Saf Risk Manag. 2019 Aug 5. doi: 10.1177/2516043519866993.
This article was updated 8/5/19.
while describing two exemplars at providing physicians with mental health support, in a recently published commentary.
“I want to call attention to the gap between what educators think and say is available, in terms of mental health support, and what trainees experience,” Dr. Poorman said in a statement on her piece in the Journal of Patient Safety and Risk Management. She shared the results of an anonymous depression survey of interns, which showed that 41.8% of participants screened positive for depression. Dr. Poorman also provided statistics on physician suicide, including that at least 66 residents killed themselves between 2000 and 2014, according to ACGME, and that another source estimated that 300-400 physician suicide deaths occur annually.
“When it comes to mental illness and suicide, we are all at risk, but we too often lacked compassion in the way we approach our colleagues. We have lacked the courage to fight the stigma that is killing us. We have not asked whether our unwillingness to reform medical training has eroded the empathy of generations of doctors. We have not done enough to fight medical boards that ask doctors about mental health diagnoses in the same way they ask if we have domestic violence charges,” wrote Dr. Poorman, who practices at a University of Washington neighborhood clinic in Kent.
“A focus on the occupational risks we face would shift us away from ‘wellness’ and ‘resilience,’ and place the onus on schools, training programs, and hospitals to do better for providers and patients,” continued Dr. Poorman, who serves on the editorial advisory board of Internal Medicine News.
She commended Oregon Health and Science University, Portland, and Stanford (Calif.) University’s divisions of general surgery for providing “rigorously confidential mental health support” through a wellness and suicide prevention program for residents and faculty, and a wellness program for residents “that emphasizes relationships, structural support, and psychological safety,” respectively. Dr. Poorman also applauded both for speaking openly about physician suicides.
SOURCE: Poorman E. J Patient Saf Risk Manag. 2019 Aug 5. doi: 10.1177/2516043519866993.
This article was updated 8/5/19.
while describing two exemplars at providing physicians with mental health support, in a recently published commentary.
“I want to call attention to the gap between what educators think and say is available, in terms of mental health support, and what trainees experience,” Dr. Poorman said in a statement on her piece in the Journal of Patient Safety and Risk Management. She shared the results of an anonymous depression survey of interns, which showed that 41.8% of participants screened positive for depression. Dr. Poorman also provided statistics on physician suicide, including that at least 66 residents killed themselves between 2000 and 2014, according to ACGME, and that another source estimated that 300-400 physician suicide deaths occur annually.
“When it comes to mental illness and suicide, we are all at risk, but we too often lacked compassion in the way we approach our colleagues. We have lacked the courage to fight the stigma that is killing us. We have not asked whether our unwillingness to reform medical training has eroded the empathy of generations of doctors. We have not done enough to fight medical boards that ask doctors about mental health diagnoses in the same way they ask if we have domestic violence charges,” wrote Dr. Poorman, who practices at a University of Washington neighborhood clinic in Kent.
“A focus on the occupational risks we face would shift us away from ‘wellness’ and ‘resilience,’ and place the onus on schools, training programs, and hospitals to do better for providers and patients,” continued Dr. Poorman, who serves on the editorial advisory board of Internal Medicine News.
She commended Oregon Health and Science University, Portland, and Stanford (Calif.) University’s divisions of general surgery for providing “rigorously confidential mental health support” through a wellness and suicide prevention program for residents and faculty, and a wellness program for residents “that emphasizes relationships, structural support, and psychological safety,” respectively. Dr. Poorman also applauded both for speaking openly about physician suicides.
SOURCE: Poorman E. J Patient Saf Risk Manag. 2019 Aug 5. doi: 10.1177/2516043519866993.
This article was updated 8/5/19.
FROM THE JOURNAL OF PATIENT SAFETY AND RISK MANAGEMENT
MS Highlights From the AAN & CMSC Annual Meetings
This supplement to Neurology Reviews compiles MS-related news briefs from the 2019 annual meetings of the American Academy of Neurology, held in Philadelphia in early May, and the Consortium of Multiple Sclerosis Centers, held in Seattle in late May.
This supplement to Neurology Reviews compiles MS-related news briefs from the 2019 annual meetings of the American Academy of Neurology, held in Philadelphia in early May, and the Consortium of Multiple Sclerosis Centers, held in Seattle in late May.
This supplement to Neurology Reviews compiles MS-related news briefs from the 2019 annual meetings of the American Academy of Neurology, held in Philadelphia in early May, and the Consortium of Multiple Sclerosis Centers, held in Seattle in late May.