User login
Staged hemispheric embolization: How to treat hemimegalencephaly within days of birth
BALTIMORE – About one in 4,000 children are born with hemimegalencephaly, meaning one brain hemisphere is abnormally formed and larger than the other.
The abnormal hemisphere causes seizures, and when they become intractable, the standard of care is to remove it as soon as possible; the longer the abnormal hemisphere is left in, the worse children do developmentally, and the less likely hemispherectomy will stop the seizures.
A problem comes up, however, when children become intractable before they’re 3 months old: “Neurosurgeons won’t touch them,” said Taeun Chang, MD, a neonatal neurointensivist at Children’s National Medical Center in Washington.
Newborns’ coagulation systems aren’t fully developed, and the risk of fatal hemorrhage is too high, she explained.
Out of what she said was a sense of “desperation” to address the situation, Dr. Chang has spearheaded a new approach for newborns at Children’s National, serial glue embolization to induce targeted strokes in the affected hemisphere. She reported on the first five cases at the American Epilepsy Society annual meeting.
At this point, “I feel like we’ve pretty much figured out the technique in terms of minimizing the complications. There’s no reason to wait anymore” for surgery as newborns get worse and worse, she said.
The technique
In two or three stages over several days, the major branches of the affected hemisphere’s anterior, middle, and posterior cerebral arteries are embolized. “You have to glue a long area and put in a lot of glue and glue up the secondary branches because [newborns] are so good at forming collaterals,” Dr. Chang said.
Fresh frozen plasma is given before and after each embolization session to boost coagulation proteins. Nicardipine is given during the procedure to prevent vasospasms. The one death in the series, case four, was in an 11-day old girl who vasospasmed, ruptured an artery over the tip of the guidewire, and hemorrhaged.
After the procedure, body temperature is kept at 36° C to prevent fever; sodium is kept high, and ins and outs are matched, to reduce brain edema; and blood pressure is tightly controlled. Children are kept on EEG during embolization and for days afterwards, and seizures, if any, are treated. The next embolization comes after peak swelling has passed in about 48-72 hours.
“The reason we can get away with this without herniation is that newborns’ skulls are soft, and their sutures are open,” so cerebral edema is manageable, Dr. Chang said.
Learning curve and outcomes
“What we learned in the first two cases” – a 23-day-old boy and 49-day-old girl – “was to create effective strokes. That’s not something any of us are taught to do,” she said.
“We were not trying to destroy the whole hemisphere, just the area that was seizing on EEG.” That was a mistake, she said: Adjacent areas began seizing and both children went on to anatomical hemispherectomies and needed shunts.
They are 5 years old now, and both on four seizure medications. The boy is in a wheelchair, fed by a G-tube, and has fewer than 20 words. The girl has a gait trainer, is fed mostly by G-tube, and has more than 50 words.
The third patient had her middle and posterior cerebral arteries embolized beginning when she was 43 days old. She was seizure free when she left the NICU, but eventually had a functional hemispherectomy. She’s 2 years old now, eating by mouth, in a gait trainer, and speaks in one- or two-word sentences. She’s on three seizure medications.
Outcomes have been best for patient five. Her posterior, middle, and anterior cerebral arteries were embolized starting at 14 days. She’s 1 year old now, seizure free on three medications, eating by G-tube and mouth, and has three-five words.
Dr. Chang said that newborns with hemimegalencephaly at Children’s National aren’t lingering as long on failing drug regimens these days. “We go to intervention now that we have this option” after they fail just two or three medications.
Given that the fifth patient, treated at 2 weeks old, is the only one who has been seizure free, she suspects it’s probably best to do embolization sooner rather than later, just as with anatomical hemispherectomy in older children. “We’ve got the sense that even a couple of weeks makes a difference. People need to come to us sooner,” Dr. Chang said.
It’s possible embolization could be a sound alternative to surgery even after 3 months of age. Focal embolization might also be a viable alternative to surgery to knock out epileptogenic lesions in children with tuberous sclerosis. Dr. Chang and her colleagues are interested in those and other possibilities, and plan to continue to develop the approach, she said.
There was no funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Chang T et al. AES 2019, Abstract 1.225.
BALTIMORE – About one in 4,000 children are born with hemimegalencephaly, meaning one brain hemisphere is abnormally formed and larger than the other.
The abnormal hemisphere causes seizures, and when they become intractable, the standard of care is to remove it as soon as possible; the longer the abnormal hemisphere is left in, the worse children do developmentally, and the less likely hemispherectomy will stop the seizures.
A problem comes up, however, when children become intractable before they’re 3 months old: “Neurosurgeons won’t touch them,” said Taeun Chang, MD, a neonatal neurointensivist at Children’s National Medical Center in Washington.
Newborns’ coagulation systems aren’t fully developed, and the risk of fatal hemorrhage is too high, she explained.
Out of what she said was a sense of “desperation” to address the situation, Dr. Chang has spearheaded a new approach for newborns at Children’s National, serial glue embolization to induce targeted strokes in the affected hemisphere. She reported on the first five cases at the American Epilepsy Society annual meeting.
At this point, “I feel like we’ve pretty much figured out the technique in terms of minimizing the complications. There’s no reason to wait anymore” for surgery as newborns get worse and worse, she said.
The technique
In two or three stages over several days, the major branches of the affected hemisphere’s anterior, middle, and posterior cerebral arteries are embolized. “You have to glue a long area and put in a lot of glue and glue up the secondary branches because [newborns] are so good at forming collaterals,” Dr. Chang said.
Fresh frozen plasma is given before and after each embolization session to boost coagulation proteins. Nicardipine is given during the procedure to prevent vasospasms. The one death in the series, case four, was in an 11-day old girl who vasospasmed, ruptured an artery over the tip of the guidewire, and hemorrhaged.
After the procedure, body temperature is kept at 36° C to prevent fever; sodium is kept high, and ins and outs are matched, to reduce brain edema; and blood pressure is tightly controlled. Children are kept on EEG during embolization and for days afterwards, and seizures, if any, are treated. The next embolization comes after peak swelling has passed in about 48-72 hours.
“The reason we can get away with this without herniation is that newborns’ skulls are soft, and their sutures are open,” so cerebral edema is manageable, Dr. Chang said.
Learning curve and outcomes
“What we learned in the first two cases” – a 23-day-old boy and 49-day-old girl – “was to create effective strokes. That’s not something any of us are taught to do,” she said.
“We were not trying to destroy the whole hemisphere, just the area that was seizing on EEG.” That was a mistake, she said: Adjacent areas began seizing and both children went on to anatomical hemispherectomies and needed shunts.
They are 5 years old now, and both on four seizure medications. The boy is in a wheelchair, fed by a G-tube, and has fewer than 20 words. The girl has a gait trainer, is fed mostly by G-tube, and has more than 50 words.
The third patient had her middle and posterior cerebral arteries embolized beginning when she was 43 days old. She was seizure free when she left the NICU, but eventually had a functional hemispherectomy. She’s 2 years old now, eating by mouth, in a gait trainer, and speaks in one- or two-word sentences. She’s on three seizure medications.
Outcomes have been best for patient five. Her posterior, middle, and anterior cerebral arteries were embolized starting at 14 days. She’s 1 year old now, seizure free on three medications, eating by G-tube and mouth, and has three-five words.
Dr. Chang said that newborns with hemimegalencephaly at Children’s National aren’t lingering as long on failing drug regimens these days. “We go to intervention now that we have this option” after they fail just two or three medications.
Given that the fifth patient, treated at 2 weeks old, is the only one who has been seizure free, she suspects it’s probably best to do embolization sooner rather than later, just as with anatomical hemispherectomy in older children. “We’ve got the sense that even a couple of weeks makes a difference. People need to come to us sooner,” Dr. Chang said.
It’s possible embolization could be a sound alternative to surgery even after 3 months of age. Focal embolization might also be a viable alternative to surgery to knock out epileptogenic lesions in children with tuberous sclerosis. Dr. Chang and her colleagues are interested in those and other possibilities, and plan to continue to develop the approach, she said.
There was no funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Chang T et al. AES 2019, Abstract 1.225.
BALTIMORE – About one in 4,000 children are born with hemimegalencephaly, meaning one brain hemisphere is abnormally formed and larger than the other.
The abnormal hemisphere causes seizures, and when they become intractable, the standard of care is to remove it as soon as possible; the longer the abnormal hemisphere is left in, the worse children do developmentally, and the less likely hemispherectomy will stop the seizures.
A problem comes up, however, when children become intractable before they’re 3 months old: “Neurosurgeons won’t touch them,” said Taeun Chang, MD, a neonatal neurointensivist at Children’s National Medical Center in Washington.
Newborns’ coagulation systems aren’t fully developed, and the risk of fatal hemorrhage is too high, she explained.
Out of what she said was a sense of “desperation” to address the situation, Dr. Chang has spearheaded a new approach for newborns at Children’s National, serial glue embolization to induce targeted strokes in the affected hemisphere. She reported on the first five cases at the American Epilepsy Society annual meeting.
At this point, “I feel like we’ve pretty much figured out the technique in terms of minimizing the complications. There’s no reason to wait anymore” for surgery as newborns get worse and worse, she said.
The technique
In two or three stages over several days, the major branches of the affected hemisphere’s anterior, middle, and posterior cerebral arteries are embolized. “You have to glue a long area and put in a lot of glue and glue up the secondary branches because [newborns] are so good at forming collaterals,” Dr. Chang said.
Fresh frozen plasma is given before and after each embolization session to boost coagulation proteins. Nicardipine is given during the procedure to prevent vasospasms. The one death in the series, case four, was in an 11-day old girl who vasospasmed, ruptured an artery over the tip of the guidewire, and hemorrhaged.
After the procedure, body temperature is kept at 36° C to prevent fever; sodium is kept high, and ins and outs are matched, to reduce brain edema; and blood pressure is tightly controlled. Children are kept on EEG during embolization and for days afterwards, and seizures, if any, are treated. The next embolization comes after peak swelling has passed in about 48-72 hours.
“The reason we can get away with this without herniation is that newborns’ skulls are soft, and their sutures are open,” so cerebral edema is manageable, Dr. Chang said.
Learning curve and outcomes
“What we learned in the first two cases” – a 23-day-old boy and 49-day-old girl – “was to create effective strokes. That’s not something any of us are taught to do,” she said.
“We were not trying to destroy the whole hemisphere, just the area that was seizing on EEG.” That was a mistake, she said: Adjacent areas began seizing and both children went on to anatomical hemispherectomies and needed shunts.
They are 5 years old now, and both on four seizure medications. The boy is in a wheelchair, fed by a G-tube, and has fewer than 20 words. The girl has a gait trainer, is fed mostly by G-tube, and has more than 50 words.
The third patient had her middle and posterior cerebral arteries embolized beginning when she was 43 days old. She was seizure free when she left the NICU, but eventually had a functional hemispherectomy. She’s 2 years old now, eating by mouth, in a gait trainer, and speaks in one- or two-word sentences. She’s on three seizure medications.
Outcomes have been best for patient five. Her posterior, middle, and anterior cerebral arteries were embolized starting at 14 days. She’s 1 year old now, seizure free on three medications, eating by G-tube and mouth, and has three-five words.
Dr. Chang said that newborns with hemimegalencephaly at Children’s National aren’t lingering as long on failing drug regimens these days. “We go to intervention now that we have this option” after they fail just two or three medications.
Given that the fifth patient, treated at 2 weeks old, is the only one who has been seizure free, she suspects it’s probably best to do embolization sooner rather than later, just as with anatomical hemispherectomy in older children. “We’ve got the sense that even a couple of weeks makes a difference. People need to come to us sooner,” Dr. Chang said.
It’s possible embolization could be a sound alternative to surgery even after 3 months of age. Focal embolization might also be a viable alternative to surgery to knock out epileptogenic lesions in children with tuberous sclerosis. Dr. Chang and her colleagues are interested in those and other possibilities, and plan to continue to develop the approach, she said.
There was no funding, and the investigators didn’t have any relevant disclosures.
SOURCE: Chang T et al. AES 2019, Abstract 1.225.
REPORTING FROM AES 2019
When Horses and Zebras Coexist: Achieving Diagnostic Excellence in the Age of High-Value Care
Safe, timely, and efficient diagnosis is fundamental for high-quality, effective healthcare. Why is diagnosis so important? First, it informs the two other main areas of medical decision-making: treatment and prognosis. These are the means by which physicians can actually change health outcomes for patients, as well as ensure that patients and their families have a realistic and accurate understanding of what the future holds with respect to their health. Second, patients and families tend to feel a sense of closure from having a name and an explanation for symptoms, even in the absence of specific treatment. Proper labeling allows patients and families to connect with others with the same diagnosis, who are best positioned to offer empathy by virtue of their similar experiences.
Despite the fundamental role of diagnosis, diagnostic error is pervasive in medicine, with unacceptable levels of resultant harm.1 In 2015, the Institute of Medicine published a landmark report, “Improving Diagnosis in Health Care,” bringing the problem to the forefront of the minds of healthcare professionals and the general public alike. According to the report, “improving the diagnostic process…represents a moral, professional, and public health imperative.”1 We must do more than avoid diagnostic error, however—we must aim to achieve diagnostic excellence. Not getting it wrong is not enough.
There are real challenges to achieving diagnostic safety, let alone excellence. The “churn” of modern hospital medicine does not reward deep diagnostic thought, nor does it often encourage reflection or collaboration, important components of being able to achieve diagnostic excellence.2 Furthermore, despite their years of training, physicians often have difficulty applying probabilistic reasoning and appropriately incorporating diagnostic information in the best evidence-based manner.3,4 In addition, there are no validated measures of diagnostic performance in practice. It is telling that many hospitalists, despite a professed interest in complex diagnosis, would rather be assigned to care for a patient with cellulitis than a patient with a complicated differential diagnosis.
Given these challenges, how can the modern healthcare ecosystem be changed to achieve diagnostic excellence? In this month’s issue of Journal of Hospital Medicine, Singer and colleagues describe a pilot project of a proposed solution to the problem.5 Aptly named, the Socrates Project is an intervention that makes available a team of “diagnosticians” that can be consulted for assistance with challenging diagnostic cases. The physicians on the team volunteer their time, allowing for deep diagnostic evaluation that is not limited by one’s daily workload, thus overcoming one of the major hurdles to achieving diagnostic excellence. The described program also focuses on harnessing the power of teamwork, which is especially relevant given recent descriptions of the effectiveness of collective intelligence in improving diagnostic performance.6 Importantly, the authors recognize that their intervention will not achieve a diagnosis in every case for which they are consulted; rather, they hope that their thorough evaluation will uncover additional potential diagnostic avenues for the referring team to pursue, with a goal to “improve patient care by providing…ideas to reduce—or at least manage—diagnostic uncertainty.”
Programs of this nature are exciting for hospitalists. Hospital medicine is, perhaps, a place in modern medicine where diagnostic excellence has a natural home. Patients admitted to the hospital are acutely (and often severely) ill, and hospitalists are tasked with rapidly identifying the cause of their illness in order to initiate appropriate treatment and accurately inform prognosis. Hospitalists, as generalists, take a broad approach to challenging cases, and they tend to practice in well-resourced environments with nearly every diagnostic modality at their disposal. Many hospitalists would envy participating in a program such as the Socrates Project.
While Singer et al.’s innovation—and the institutional support thereof—should be lauded, some discussion must be had about how to assess the effectiveness of such a program. The authors acknowledge the need for evaluation of both the diagnostic process and the outcomes that process achieves. Measuring diagnostic performance is challenging, however, and while there is substantial progress being made in this area, recent efforts tend to focus on identifying diagnostic errors rather than measuring diagnostic excellence. Moreover, even if a program does improve diagnostic performance, how should we evaluate for unintended consequences of its implementation? In the age of high-value care, how can we ensure that efforts to do a better job of spotting proverbial zebras do not come at the cost of harming too many horses?7
Hospitalists are well primed to answer this question. The juxtaposition of Singer et al.’s article with the Journal of Hospital Medicine’s long-running series on Choosing Wisely®: Things We Do for No Reason™ provides a natural synergy to begin crafting a framework to evaluate unintended consequences of a program in diagnostic excellence. More diagnosis is not the goal; more appropriate diagnosis is what is needed. A clinical program aimed at achieving diagnostic excellence should not employ low-value, wasteful strategies that do not add substantively to the diagnostic process but should instead seek to improve the overall efficiency of even complicated diagnostic odysseys. Avoiding waste throughout will allow for allocation of diagnostic resources where they are needed. In turn, hospitalists can do a better job of correctly identifying both horses and zebras for what they are. While a given hospitalization for a diagnostically complex patient may be relatively expensive, better diagnosis during an index hospitalization is likely to lead to decreased downstream costs, such as those related to readmissions and further testing, as well as better health outcomes.
The Socrates Project, along with similar programs at other institutions, are exciting innovations. These programs are not only likely to be good for patients but are also good for hospitalists. The field of hospital medicine should leverage its collective expertise in clinical medicine, systems of care, and high-value care to become a home for diagnostic excellence.
1. National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015. https://doi.org/10.17226/21794
2. Olson A, Rencic J, Cosby K, et al. Competencies for improving diagnosis: an interprofessional framework for education and training in health care. Diagnosis. 2019;6(4):335-341. https://doi.org/10.1515/dx-2018-0107.
3. Baduashvili A, Guyatt G, Evans AT. ROC anatomy—getting the most out of your diagnostic test. J Gen Intern Med. 2019;34(9):1892-1898. https://doi.org/10.1007/s11606-019-05125-0.
4. Manrai AK, Bhatia G, Strymish J, Kohane IS, Jain SH. Medicine’s uncomfortable relationship with math: calculating positive predictive value. JAMA Intern Med. 2014;174(6):991-993. https://doi.org/10.1001/jamainternmed.2014.1059.
5. Singer BD, Goodwin AM, Patel AA, Vaughan DE. The Socrates Project for difficult diagnosis at Northwestern Medicine. J Hosp Med. 2020;15(2):116-118. https://doi.org/ 10.12788/jhm.3335.
6. Barnett ML, Boddupalli D, Nundy S, Bates DW. Comparative accuracy of diagnosis by collective intelligence of multiple physicians vs individual physicians. JAMA Netw Open. 2019;2(3):e190096. https://doi.org/10.1001/jamanetworkopen.2019.0096.
7. Dhaliwal G. Bringing high-value care to the inpatient teaching service. JAMA Intern Med. 2014;174(7):1021-1022. https://doi.org/10.1001/jamainternmed.2014.2012.
Safe, timely, and efficient diagnosis is fundamental for high-quality, effective healthcare. Why is diagnosis so important? First, it informs the two other main areas of medical decision-making: treatment and prognosis. These are the means by which physicians can actually change health outcomes for patients, as well as ensure that patients and their families have a realistic and accurate understanding of what the future holds with respect to their health. Second, patients and families tend to feel a sense of closure from having a name and an explanation for symptoms, even in the absence of specific treatment. Proper labeling allows patients and families to connect with others with the same diagnosis, who are best positioned to offer empathy by virtue of their similar experiences.
Despite the fundamental role of diagnosis, diagnostic error is pervasive in medicine, with unacceptable levels of resultant harm.1 In 2015, the Institute of Medicine published a landmark report, “Improving Diagnosis in Health Care,” bringing the problem to the forefront of the minds of healthcare professionals and the general public alike. According to the report, “improving the diagnostic process…represents a moral, professional, and public health imperative.”1 We must do more than avoid diagnostic error, however—we must aim to achieve diagnostic excellence. Not getting it wrong is not enough.
There are real challenges to achieving diagnostic safety, let alone excellence. The “churn” of modern hospital medicine does not reward deep diagnostic thought, nor does it often encourage reflection or collaboration, important components of being able to achieve diagnostic excellence.2 Furthermore, despite their years of training, physicians often have difficulty applying probabilistic reasoning and appropriately incorporating diagnostic information in the best evidence-based manner.3,4 In addition, there are no validated measures of diagnostic performance in practice. It is telling that many hospitalists, despite a professed interest in complex diagnosis, would rather be assigned to care for a patient with cellulitis than a patient with a complicated differential diagnosis.
Given these challenges, how can the modern healthcare ecosystem be changed to achieve diagnostic excellence? In this month’s issue of Journal of Hospital Medicine, Singer and colleagues describe a pilot project of a proposed solution to the problem.5 Aptly named, the Socrates Project is an intervention that makes available a team of “diagnosticians” that can be consulted for assistance with challenging diagnostic cases. The physicians on the team volunteer their time, allowing for deep diagnostic evaluation that is not limited by one’s daily workload, thus overcoming one of the major hurdles to achieving diagnostic excellence. The described program also focuses on harnessing the power of teamwork, which is especially relevant given recent descriptions of the effectiveness of collective intelligence in improving diagnostic performance.6 Importantly, the authors recognize that their intervention will not achieve a diagnosis in every case for which they are consulted; rather, they hope that their thorough evaluation will uncover additional potential diagnostic avenues for the referring team to pursue, with a goal to “improve patient care by providing…ideas to reduce—or at least manage—diagnostic uncertainty.”
Programs of this nature are exciting for hospitalists. Hospital medicine is, perhaps, a place in modern medicine where diagnostic excellence has a natural home. Patients admitted to the hospital are acutely (and often severely) ill, and hospitalists are tasked with rapidly identifying the cause of their illness in order to initiate appropriate treatment and accurately inform prognosis. Hospitalists, as generalists, take a broad approach to challenging cases, and they tend to practice in well-resourced environments with nearly every diagnostic modality at their disposal. Many hospitalists would envy participating in a program such as the Socrates Project.
While Singer et al.’s innovation—and the institutional support thereof—should be lauded, some discussion must be had about how to assess the effectiveness of such a program. The authors acknowledge the need for evaluation of both the diagnostic process and the outcomes that process achieves. Measuring diagnostic performance is challenging, however, and while there is substantial progress being made in this area, recent efforts tend to focus on identifying diagnostic errors rather than measuring diagnostic excellence. Moreover, even if a program does improve diagnostic performance, how should we evaluate for unintended consequences of its implementation? In the age of high-value care, how can we ensure that efforts to do a better job of spotting proverbial zebras do not come at the cost of harming too many horses?7
Hospitalists are well primed to answer this question. The juxtaposition of Singer et al.’s article with the Journal of Hospital Medicine’s long-running series on Choosing Wisely®: Things We Do for No Reason™ provides a natural synergy to begin crafting a framework to evaluate unintended consequences of a program in diagnostic excellence. More diagnosis is not the goal; more appropriate diagnosis is what is needed. A clinical program aimed at achieving diagnostic excellence should not employ low-value, wasteful strategies that do not add substantively to the diagnostic process but should instead seek to improve the overall efficiency of even complicated diagnostic odysseys. Avoiding waste throughout will allow for allocation of diagnostic resources where they are needed. In turn, hospitalists can do a better job of correctly identifying both horses and zebras for what they are. While a given hospitalization for a diagnostically complex patient may be relatively expensive, better diagnosis during an index hospitalization is likely to lead to decreased downstream costs, such as those related to readmissions and further testing, as well as better health outcomes.
The Socrates Project, along with similar programs at other institutions, are exciting innovations. These programs are not only likely to be good for patients but are also good for hospitalists. The field of hospital medicine should leverage its collective expertise in clinical medicine, systems of care, and high-value care to become a home for diagnostic excellence.
Safe, timely, and efficient diagnosis is fundamental for high-quality, effective healthcare. Why is diagnosis so important? First, it informs the two other main areas of medical decision-making: treatment and prognosis. These are the means by which physicians can actually change health outcomes for patients, as well as ensure that patients and their families have a realistic and accurate understanding of what the future holds with respect to their health. Second, patients and families tend to feel a sense of closure from having a name and an explanation for symptoms, even in the absence of specific treatment. Proper labeling allows patients and families to connect with others with the same diagnosis, who are best positioned to offer empathy by virtue of their similar experiences.
Despite the fundamental role of diagnosis, diagnostic error is pervasive in medicine, with unacceptable levels of resultant harm.1 In 2015, the Institute of Medicine published a landmark report, “Improving Diagnosis in Health Care,” bringing the problem to the forefront of the minds of healthcare professionals and the general public alike. According to the report, “improving the diagnostic process…represents a moral, professional, and public health imperative.”1 We must do more than avoid diagnostic error, however—we must aim to achieve diagnostic excellence. Not getting it wrong is not enough.
There are real challenges to achieving diagnostic safety, let alone excellence. The “churn” of modern hospital medicine does not reward deep diagnostic thought, nor does it often encourage reflection or collaboration, important components of being able to achieve diagnostic excellence.2 Furthermore, despite their years of training, physicians often have difficulty applying probabilistic reasoning and appropriately incorporating diagnostic information in the best evidence-based manner.3,4 In addition, there are no validated measures of diagnostic performance in practice. It is telling that many hospitalists, despite a professed interest in complex diagnosis, would rather be assigned to care for a patient with cellulitis than a patient with a complicated differential diagnosis.
Given these challenges, how can the modern healthcare ecosystem be changed to achieve diagnostic excellence? In this month’s issue of Journal of Hospital Medicine, Singer and colleagues describe a pilot project of a proposed solution to the problem.5 Aptly named, the Socrates Project is an intervention that makes available a team of “diagnosticians” that can be consulted for assistance with challenging diagnostic cases. The physicians on the team volunteer their time, allowing for deep diagnostic evaluation that is not limited by one’s daily workload, thus overcoming one of the major hurdles to achieving diagnostic excellence. The described program also focuses on harnessing the power of teamwork, which is especially relevant given recent descriptions of the effectiveness of collective intelligence in improving diagnostic performance.6 Importantly, the authors recognize that their intervention will not achieve a diagnosis in every case for which they are consulted; rather, they hope that their thorough evaluation will uncover additional potential diagnostic avenues for the referring team to pursue, with a goal to “improve patient care by providing…ideas to reduce—or at least manage—diagnostic uncertainty.”
Programs of this nature are exciting for hospitalists. Hospital medicine is, perhaps, a place in modern medicine where diagnostic excellence has a natural home. Patients admitted to the hospital are acutely (and often severely) ill, and hospitalists are tasked with rapidly identifying the cause of their illness in order to initiate appropriate treatment and accurately inform prognosis. Hospitalists, as generalists, take a broad approach to challenging cases, and they tend to practice in well-resourced environments with nearly every diagnostic modality at their disposal. Many hospitalists would envy participating in a program such as the Socrates Project.
While Singer et al.’s innovation—and the institutional support thereof—should be lauded, some discussion must be had about how to assess the effectiveness of such a program. The authors acknowledge the need for evaluation of both the diagnostic process and the outcomes that process achieves. Measuring diagnostic performance is challenging, however, and while there is substantial progress being made in this area, recent efforts tend to focus on identifying diagnostic errors rather than measuring diagnostic excellence. Moreover, even if a program does improve diagnostic performance, how should we evaluate for unintended consequences of its implementation? In the age of high-value care, how can we ensure that efforts to do a better job of spotting proverbial zebras do not come at the cost of harming too many horses?7
Hospitalists are well primed to answer this question. The juxtaposition of Singer et al.’s article with the Journal of Hospital Medicine’s long-running series on Choosing Wisely®: Things We Do for No Reason™ provides a natural synergy to begin crafting a framework to evaluate unintended consequences of a program in diagnostic excellence. More diagnosis is not the goal; more appropriate diagnosis is what is needed. A clinical program aimed at achieving diagnostic excellence should not employ low-value, wasteful strategies that do not add substantively to the diagnostic process but should instead seek to improve the overall efficiency of even complicated diagnostic odysseys. Avoiding waste throughout will allow for allocation of diagnostic resources where they are needed. In turn, hospitalists can do a better job of correctly identifying both horses and zebras for what they are. While a given hospitalization for a diagnostically complex patient may be relatively expensive, better diagnosis during an index hospitalization is likely to lead to decreased downstream costs, such as those related to readmissions and further testing, as well as better health outcomes.
The Socrates Project, along with similar programs at other institutions, are exciting innovations. These programs are not only likely to be good for patients but are also good for hospitalists. The field of hospital medicine should leverage its collective expertise in clinical medicine, systems of care, and high-value care to become a home for diagnostic excellence.
1. National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015. https://doi.org/10.17226/21794
2. Olson A, Rencic J, Cosby K, et al. Competencies for improving diagnosis: an interprofessional framework for education and training in health care. Diagnosis. 2019;6(4):335-341. https://doi.org/10.1515/dx-2018-0107.
3. Baduashvili A, Guyatt G, Evans AT. ROC anatomy—getting the most out of your diagnostic test. J Gen Intern Med. 2019;34(9):1892-1898. https://doi.org/10.1007/s11606-019-05125-0.
4. Manrai AK, Bhatia G, Strymish J, Kohane IS, Jain SH. Medicine’s uncomfortable relationship with math: calculating positive predictive value. JAMA Intern Med. 2014;174(6):991-993. https://doi.org/10.1001/jamainternmed.2014.1059.
5. Singer BD, Goodwin AM, Patel AA, Vaughan DE. The Socrates Project for difficult diagnosis at Northwestern Medicine. J Hosp Med. 2020;15(2):116-118. https://doi.org/ 10.12788/jhm.3335.
6. Barnett ML, Boddupalli D, Nundy S, Bates DW. Comparative accuracy of diagnosis by collective intelligence of multiple physicians vs individual physicians. JAMA Netw Open. 2019;2(3):e190096. https://doi.org/10.1001/jamanetworkopen.2019.0096.
7. Dhaliwal G. Bringing high-value care to the inpatient teaching service. JAMA Intern Med. 2014;174(7):1021-1022. https://doi.org/10.1001/jamainternmed.2014.2012.
1. National Academies of Sciences, Engineering, and Medicine. Improving Diagnosis in Health Care. Washington, DC: The National Academies Press; 2015. https://doi.org/10.17226/21794
2. Olson A, Rencic J, Cosby K, et al. Competencies for improving diagnosis: an interprofessional framework for education and training in health care. Diagnosis. 2019;6(4):335-341. https://doi.org/10.1515/dx-2018-0107.
3. Baduashvili A, Guyatt G, Evans AT. ROC anatomy—getting the most out of your diagnostic test. J Gen Intern Med. 2019;34(9):1892-1898. https://doi.org/10.1007/s11606-019-05125-0.
4. Manrai AK, Bhatia G, Strymish J, Kohane IS, Jain SH. Medicine’s uncomfortable relationship with math: calculating positive predictive value. JAMA Intern Med. 2014;174(6):991-993. https://doi.org/10.1001/jamainternmed.2014.1059.
5. Singer BD, Goodwin AM, Patel AA, Vaughan DE. The Socrates Project for difficult diagnosis at Northwestern Medicine. J Hosp Med. 2020;15(2):116-118. https://doi.org/ 10.12788/jhm.3335.
6. Barnett ML, Boddupalli D, Nundy S, Bates DW. Comparative accuracy of diagnosis by collective intelligence of multiple physicians vs individual physicians. JAMA Netw Open. 2019;2(3):e190096. https://doi.org/10.1001/jamanetworkopen.2019.0096.
7. Dhaliwal G. Bringing high-value care to the inpatient teaching service. JAMA Intern Med. 2014;174(7):1021-1022. https://doi.org/10.1001/jamainternmed.2014.2012.
© 2020 Society of Hospital Medicine
Leadership & Professional Development: A Letter to the Future Teaching Physician
“No one cares how much you know, until they know how much you care.”
—Theodore Roosevelt (attributed)
Like many early career clinician-educators, you are likely embarking on your teaching role with excitement and trepidation. Excitement accompanies the opportunity to develop the next generation of physicians. Trepidation arises from a fear of insufficient knowledge. This concern is understandable but misplaced: great teachers are great because of their emotional intelligence, not their medical intelligence. These five principles will help you establish an optimal learning environment.
Small-Talk before Med-Talk. “What do you like to do outside of the hospital?” “Where is your favorite place to eat?” These questions indicate that your interest in learners transcends clinical work. Leaders who are more relationship- than task-oriented achieve greater group cohesion and more team learning. Exemplary inpatient attending physicians use learners’ first names and get to know them on a personal level to signal that they care as much about the person as they do about the performance.1
Be Available. Medical educators balance supervision and autonomy while trainees engage in high-stakes decisions. The best teachers get this right by signaling “I have faith in you” and “I’m always available.” Clinician-educator Kimberly Manning, MD portrayed this balance in a recent Twitter thread. The resident called: “I am sorry to bother you.” Dr. Manning responded, “Never be sorry.” The resident was concerned about a patient with new abdominal pain but reassured Dr. Manning that she did not need to return to the hospital. She returned anyway. She assessed the patient and had nothing to add to the resident’s outstanding management. As the patient recovered from his operation for a perforated ulcer, Dr. Manning reflected, “On a perfect Saturday afternoon, I chose to return to the hospital. To make not one decision or write one single order. But instead to stand beside my resident and intentionally affirm her.”
Build from the Ground Up. Asking questions is the teacher’s core procedure. Strive to master the true Socratic method of starting with an elemental inquiry and then leading a conversation that poses questions of increasing difficulty until you reach the limits of the learner’s understanding. This method reinforces their hard-earned knowledge and sets the stage for growth. “What would be your first test to evaluate tachycardia?” Once the correct answer is firmly in hand, explore the margin of their knowledge. “Which regular, narrow complex tachycardias stop with adenosine?”
Never Judge. Never endorse an incorrect response—but do not disparage it either. A trainee must learn that their answer was wrong but should not feel defeated or embarrassed. Use judgment regarding whether constructive feedback should be delivered in public or in private.
I recall answering a question incorrectly in medical school. The attending responded, “How many years did you take off before starting third year?” I had not taken any time off. The attending was a phenomenal clinician but a lousy teacher. A master teacher would have accessed a foothold and built my knowledge without judgment.
Remain Humble. One of the most liberating phrases you will deploy as a teacher is “I don’t know.” Its utterance demonstrates the honesty and humility you hope to instill in learners. Be on the lookout for the many times your trainees will know more than you.
Recently my team evaluated a patient with blunted facial expression, bradykinesia, and a resting hand tremor. I disclosed to my team: “I don’t know the key maneuvers to distinguish the Parkinson plus syndromes from Parkinson disease.” The medical student had spent one year studying patients with neurodegenerative diseases (I learned this during the “small-talk before med-talk” phase). I invited him to demonstrate the neurologic exam, which he did admirably. That day I did not know the subject well, and we all learned because I freely admitted it.
Being a physician is the greatest job in the world. If you leverage your EQ (emotional quotient) as much as your IQ (intelligence quotient), your learners will conclude the same.
1. Houchens N, Harrod M, Moody S, Fowler KE, Saint S. Techniques and behaviors associated with exemplary inpatient general medicine teaching: an exploratory qualitative study. J Hosp Med. 2017;12(7):503-509. https://doi.org/10.12788/jhm.2763.
“No one cares how much you know, until they know how much you care.”
—Theodore Roosevelt (attributed)
Like many early career clinician-educators, you are likely embarking on your teaching role with excitement and trepidation. Excitement accompanies the opportunity to develop the next generation of physicians. Trepidation arises from a fear of insufficient knowledge. This concern is understandable but misplaced: great teachers are great because of their emotional intelligence, not their medical intelligence. These five principles will help you establish an optimal learning environment.
Small-Talk before Med-Talk. “What do you like to do outside of the hospital?” “Where is your favorite place to eat?” These questions indicate that your interest in learners transcends clinical work. Leaders who are more relationship- than task-oriented achieve greater group cohesion and more team learning. Exemplary inpatient attending physicians use learners’ first names and get to know them on a personal level to signal that they care as much about the person as they do about the performance.1
Be Available. Medical educators balance supervision and autonomy while trainees engage in high-stakes decisions. The best teachers get this right by signaling “I have faith in you” and “I’m always available.” Clinician-educator Kimberly Manning, MD portrayed this balance in a recent Twitter thread. The resident called: “I am sorry to bother you.” Dr. Manning responded, “Never be sorry.” The resident was concerned about a patient with new abdominal pain but reassured Dr. Manning that she did not need to return to the hospital. She returned anyway. She assessed the patient and had nothing to add to the resident’s outstanding management. As the patient recovered from his operation for a perforated ulcer, Dr. Manning reflected, “On a perfect Saturday afternoon, I chose to return to the hospital. To make not one decision or write one single order. But instead to stand beside my resident and intentionally affirm her.”
Build from the Ground Up. Asking questions is the teacher’s core procedure. Strive to master the true Socratic method of starting with an elemental inquiry and then leading a conversation that poses questions of increasing difficulty until you reach the limits of the learner’s understanding. This method reinforces their hard-earned knowledge and sets the stage for growth. “What would be your first test to evaluate tachycardia?” Once the correct answer is firmly in hand, explore the margin of their knowledge. “Which regular, narrow complex tachycardias stop with adenosine?”
Never Judge. Never endorse an incorrect response—but do not disparage it either. A trainee must learn that their answer was wrong but should not feel defeated or embarrassed. Use judgment regarding whether constructive feedback should be delivered in public or in private.
I recall answering a question incorrectly in medical school. The attending responded, “How many years did you take off before starting third year?” I had not taken any time off. The attending was a phenomenal clinician but a lousy teacher. A master teacher would have accessed a foothold and built my knowledge without judgment.
Remain Humble. One of the most liberating phrases you will deploy as a teacher is “I don’t know.” Its utterance demonstrates the honesty and humility you hope to instill in learners. Be on the lookout for the many times your trainees will know more than you.
Recently my team evaluated a patient with blunted facial expression, bradykinesia, and a resting hand tremor. I disclosed to my team: “I don’t know the key maneuvers to distinguish the Parkinson plus syndromes from Parkinson disease.” The medical student had spent one year studying patients with neurodegenerative diseases (I learned this during the “small-talk before med-talk” phase). I invited him to demonstrate the neurologic exam, which he did admirably. That day I did not know the subject well, and we all learned because I freely admitted it.
Being a physician is the greatest job in the world. If you leverage your EQ (emotional quotient) as much as your IQ (intelligence quotient), your learners will conclude the same.
“No one cares how much you know, until they know how much you care.”
—Theodore Roosevelt (attributed)
Like many early career clinician-educators, you are likely embarking on your teaching role with excitement and trepidation. Excitement accompanies the opportunity to develop the next generation of physicians. Trepidation arises from a fear of insufficient knowledge. This concern is understandable but misplaced: great teachers are great because of their emotional intelligence, not their medical intelligence. These five principles will help you establish an optimal learning environment.
Small-Talk before Med-Talk. “What do you like to do outside of the hospital?” “Where is your favorite place to eat?” These questions indicate that your interest in learners transcends clinical work. Leaders who are more relationship- than task-oriented achieve greater group cohesion and more team learning. Exemplary inpatient attending physicians use learners’ first names and get to know them on a personal level to signal that they care as much about the person as they do about the performance.1
Be Available. Medical educators balance supervision and autonomy while trainees engage in high-stakes decisions. The best teachers get this right by signaling “I have faith in you” and “I’m always available.” Clinician-educator Kimberly Manning, MD portrayed this balance in a recent Twitter thread. The resident called: “I am sorry to bother you.” Dr. Manning responded, “Never be sorry.” The resident was concerned about a patient with new abdominal pain but reassured Dr. Manning that she did not need to return to the hospital. She returned anyway. She assessed the patient and had nothing to add to the resident’s outstanding management. As the patient recovered from his operation for a perforated ulcer, Dr. Manning reflected, “On a perfect Saturday afternoon, I chose to return to the hospital. To make not one decision or write one single order. But instead to stand beside my resident and intentionally affirm her.”
Build from the Ground Up. Asking questions is the teacher’s core procedure. Strive to master the true Socratic method of starting with an elemental inquiry and then leading a conversation that poses questions of increasing difficulty until you reach the limits of the learner’s understanding. This method reinforces their hard-earned knowledge and sets the stage for growth. “What would be your first test to evaluate tachycardia?” Once the correct answer is firmly in hand, explore the margin of their knowledge. “Which regular, narrow complex tachycardias stop with adenosine?”
Never Judge. Never endorse an incorrect response—but do not disparage it either. A trainee must learn that their answer was wrong but should not feel defeated or embarrassed. Use judgment regarding whether constructive feedback should be delivered in public or in private.
I recall answering a question incorrectly in medical school. The attending responded, “How many years did you take off before starting third year?” I had not taken any time off. The attending was a phenomenal clinician but a lousy teacher. A master teacher would have accessed a foothold and built my knowledge without judgment.
Remain Humble. One of the most liberating phrases you will deploy as a teacher is “I don’t know.” Its utterance demonstrates the honesty and humility you hope to instill in learners. Be on the lookout for the many times your trainees will know more than you.
Recently my team evaluated a patient with blunted facial expression, bradykinesia, and a resting hand tremor. I disclosed to my team: “I don’t know the key maneuvers to distinguish the Parkinson plus syndromes from Parkinson disease.” The medical student had spent one year studying patients with neurodegenerative diseases (I learned this during the “small-talk before med-talk” phase). I invited him to demonstrate the neurologic exam, which he did admirably. That day I did not know the subject well, and we all learned because I freely admitted it.
Being a physician is the greatest job in the world. If you leverage your EQ (emotional quotient) as much as your IQ (intelligence quotient), your learners will conclude the same.
1. Houchens N, Harrod M, Moody S, Fowler KE, Saint S. Techniques and behaviors associated with exemplary inpatient general medicine teaching: an exploratory qualitative study. J Hosp Med. 2017;12(7):503-509. https://doi.org/10.12788/jhm.2763.
1. Houchens N, Harrod M, Moody S, Fowler KE, Saint S. Techniques and behaviors associated with exemplary inpatient general medicine teaching: an exploratory qualitative study. J Hosp Med. 2017;12(7):503-509. https://doi.org/10.12788/jhm.2763.
© 2020 Society of Hospital Medicine
Decreasing Hypoglycemia following Insulin Administration for Inpatient Hyperkalemia
Hyperkalemia (serum potassium ≥5.1 mEq/L), if left untreated, may result in cardiac arrhythmias, severe muscle weakness, or paralysis.1,2 Insulin administration can rapidly correct hyperkalemia by shifting serum potassiufm intracellularly.3 Treatment of hyperkalemia with insulin may lead to hypoglycemia, which, when severe, can cause confusion, seizures, loss of consciousness, and death. The use of regular and short-acting insulins to correct hyperkalemia quickly in hospitalized patients results in the greatest risk of hypoglycemia within three hours of treatment.4 Nonetheless, monitoring blood glucose levels within six hours of postinsulin administration is not a standard part of hyperkalemia treatment guidelines,3 leaving the rates of hypoglycemia in this setting poorly characterized.
Without standardized blood glucose measurement protocols, retrospective studies have reported posttreatment hypoglycemia rates of 8.7%-17.5% among all patients with hyperkalemia,5,6 and 13% among patients with end-stage renal disease.4 These estimates likely underestimate the true hypoglycemia rates as they measure blood glucose sporadically and are often outside the three-hour window of highest risk after insulin administration.
At the University of California, San Francisco Medical Center (UCSFMC), we faced similar issues in measuring the true hypoglycemia rates associated with hyperkalemia treatment. In December 2015, a 12-month retrospective review revealed a 12% hypoglycemia rate among patients treated with insulin for hyperkalemia. This review was limited by the inclusion of only patients treated for hyperkalemia using the standard orderset supplied with the electronic health record system (EHR; EPIC Systems, Verona, Wisconsin) and the absence of specific orders for glucose monitoring. As a result, more than 40% of these inpatients had no documented glucose within six hours of postinsulin administration.
We subsequently designed and implemented an adult inpatient hyperkalemia treatment orderset aimed at reducing iatrogenic hypoglycemia by promoting appropriate insulin use and blood glucose monitoring during the treatment of hyperkalemia. Through rapid improvement cycles, we iteratively revised the orderset to optimally mitigate the risk of hypoglycemia that was associated with insulin use. We describe implementation and outcomes of weight-based insulin dosing,7 automated alerts to identify patients at greatest risk for hypoglycemia, and clinical decision support based on the preinsulin blood glucose level. We report the rates of iatrogenic hypoglycemia after the implementation of these order-set changes.
METHODS
Design Overview
EHR data were extracted from Epic Clarity. We analyzed data following Orderset 1.1 implementation (January 1, 2016-March 19, 2017) when hypoglycemia rates were reliably quantifiable and following orderset revision 1.2 (March 20, 2017-September 30, 2017) to evaluate the impact of the orderset intervention. The data collection was approved by the Institutional Review Board at the University of California, San Francisco.
Additionally, we explored the frequency in which providers ordered insulin through the hyperkalemia orderset for each version of the orderset via two-month baseline reviews. Investigation for Orderset 1.1 was from January 1, 2017 to February 28, 2017 and for Orderset 1.2 was from August 1, 2017 to September 30, 2017. Insulin ordering frequency through the hyperkalemia orderset was defined as ordering insulin through the adult inpatient hyperkalemia orderset versus ordering insulin in and outside of the hyperkalemia orderset.
Last, we measured the nursing point of care testing (POCT) blood glucose measurement compliance with the hyperkalemia orderset. Nursing utilization acceptance of the hyperkalemia orderset was defined as adequate POCT blood glucose levels monitored in comparison to all insulin treatments via the hyperkalemia orderset.
Setting and Participants
We evaluated nonobstetric adult inpatients admitted to UCSF Medical Center between January 2016 and September 2017. All medical and surgical wards and intensive care units were included in the analysis.
Intervention
In June 2012, an EHR developed by Epic Systems was introduced at UCSFMC. In January 2016, we designed a new EHR-based hyperkalemia treatment orderset (Orderset 1.1), which added standard POCT blood glucose checks before and at one, two, four, and six hours after insulin injection (Appendix 1). In March 2017, a newly designed orderset (Orderset 1.2) replaced the previous hyperkalemia treatment orderset (Appendix 2). Orderset 1.2 included three updates. First, providers were now presented the option of ordering insulin as a
CORRECTED FIGURE PER ERRATUM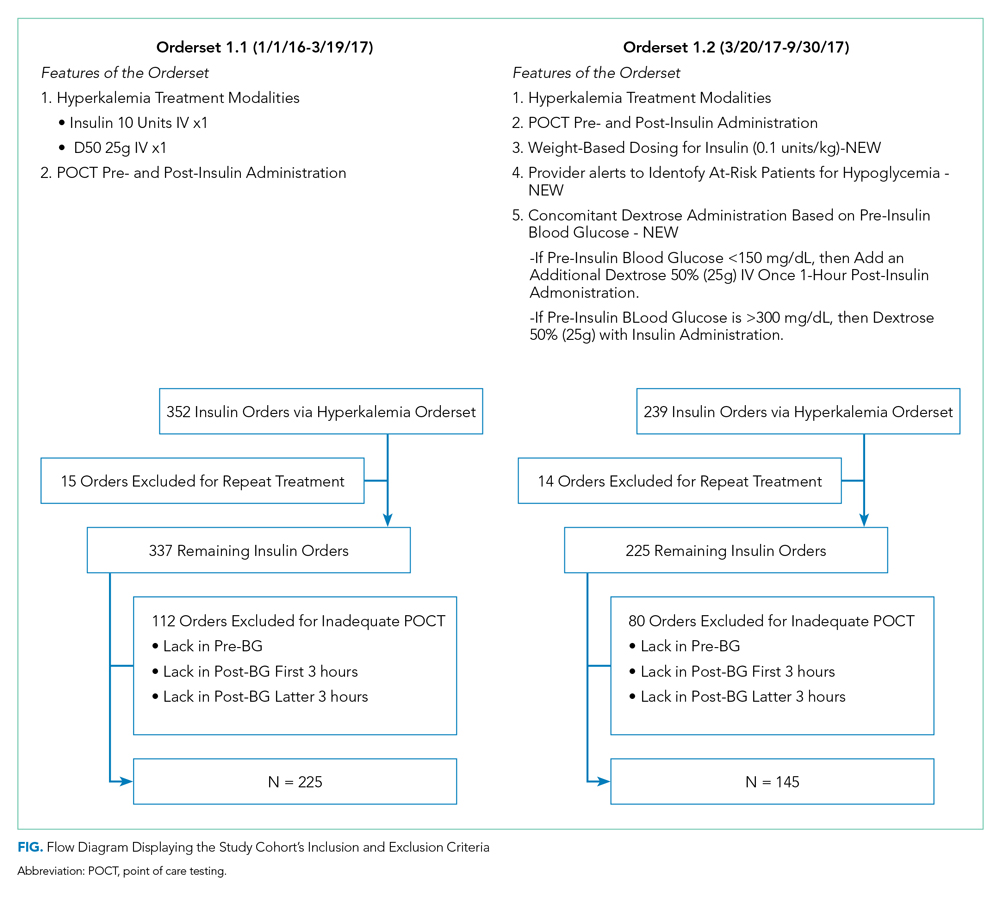
Inclusion and exclusion criteria are shown in the Figure. All patients who had insulin ordered via a hyperkalemia orderset were included in an intention-to-treat analysis. A further analysis was performed for patients for whom orderset compliance was achieved (ie, insulin ordered through the ordersets with adequate blood glucose monitoring). These patients were required to have a POCT blood glucose check preinsulin administration and postinsulin administration as follows: (1) between 30 to 180 minutes (0.5 to three hours) after insulin administration, and (2) between 180 and 360 minutes (three to six hours) after insulin administration. For patients receiving repeated insulin treatments for hyperkalemia within six hours, the first treatment data points were excluded to prevent duplication.
Outcomes
We extracted data on all nonobstetric adult patients admitted to UCSFMC between January 1, 2016 and March 19, 2017 (Orderset 1.1) and between March 20, 2017 and September 30, 2017 (Orderset 1.2).
We measured unique insulin administrations given that each insulin injection poses a risk of iatrogenic hypoglycemia. Hypoglycemia was defined as glucose <70 mg/dL and severe hypoglycemia was defined as glucose <40 mg/dL. Covariates included time and date of insulin administration; blood glucose levels before and at one, two, four, and six hours after insulin injection (if available); sex; weight; dose of insulin given for hyperkalemia treatment; creatinine; known diagnosis of diabetes; concomitant use of albuterol; and concomitant use of corticosteroids. Hyperglycemia was defined as glucose >180 mg/dL. We collected potassium levels pre- and postinsulin treatment. The responsible team’s discipline and the location of the patient (eg, medical/surgical unit, intensive care unit, emergency department) where the insulin orderset was used were recorded.
Statistical Analysis
Statistical analysis for our data included the χ2 test for categorical data and Student t test for continuous data. The bivariate analysis identified potential risk factors and protective factors for hypoglycemia, and logistic regression was used to determine independent predictors of hypoglycemia. Through bivariate analyses, any factor with a P value below .05 was included in the multivariable analyses to investigate a significant contribution to hypoglycemia outcomes. Analyses for hypoglycemia and severe hypoglycemia rates, potassium levels pre- and postinsulin treatment, and hyperglycemia rates were done for both the intention-to-treat group and the group with all criteria met. All analyses were rendered utilizing Stata version 14 (Stata Corp LLC, College Station, Texas).
RESULTS
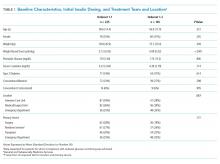
Baseline patient characteristics, initial insulin dosing, the treatment team, and the location are shown in Table 1. With the implementation of weight-based dosing, a lower dose of insulin was administered with Orderset 1.2 compared with Orderset 1.1.
Orderset adherence rates for Orderset 1.1 and 1.2 were as follows: Acute Care Floor 65% (70%), Intensive Care Unit 63% (66%), and Emergency Department 60% (55%). A two-month audit of orderset usage and compliance revealed that 73% (70 of 96) of insulin treatments were ordered through Orderset 1.1, and 77% (71 of 92) of insulin treatments were ordered through Orderset 1.2. The distribution of orderset usage across location and primary service are shown in Table 1.
The patient distribution is shown in the Figure. In the Orderset 1.1 period, there were 352 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 225 patients for whom compliance with orderset monitoring was achieved. Notably, 112 treatments were excluded for the lack of adequate blood glucose monitoring. In the Orderset 1.2 period, there were 239 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 145 patients for whom compliance with orderset monitoring was achieved. During this phase, 80 treatments were excluded for inadequate blood glucose monitoring.
Predictors of hypoglycemia following the implementation of Orderset 1.1 are shown in Table 2, and the logistic regression model of these risks is shown in Appendix Table 1. Female gender, weight-based dosing of insulin exceeding 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dl were associated with an increased risk of hypoglycemia. A known diagnosis of Type 2 diabetes, concomitant albuterol within one hour of insulin administration, and corticosteroid administration within two hours of insulin administration were associated with a decreased risk of hypoglycemia.
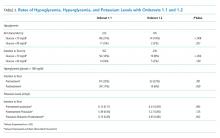
The rates of hypoglycemia (<70 mg/dl) and severe hypoglycemia (<40 mg/dl) are shown in Table 3. During the Orderset 1.1 period,
During the Orderset 1.2 period, for patients with all criteria met, 14 of 145 (10%) had hypoglycemia, and three of 145 (2%) had severe hypoglycemia. Ten of 14 (72%) of these hypoglycemic events occurred in the first three hours, with the remaining four hypoglycemic events (28%) occurring in the last three hours.
An intention-to-treat analysis for hyperglycemia, defined as glucose >180 mg/dl, revealed that during the Orderset 1.1 period, 80 of 352 (23%) had hyperglycemia before insulin administration, and 38 of 352 (11%) had hyperglycemia after insulin administration. During the Orderset 1.2 period, 52 of 239 (22%) had hyperglycemia before insulin administration, and 15 of 239 (6%) had hyperglycemia after insulin administration. Results can be found in Table 3.
Pre- and posttreatment potassium levels are shown in Table 3. An intention-to-treat analysis for potassium reduction postinsulin administration revealed that during the Orderset 1.1 period, there was an absolute reduction of 0.73 mmol/L, while during the Orderset 1.2 period, there was an absolute reduction of 0.95 mmol/L.
DISCUSSION
Treatment of hyperkalemia with insulin may result in significant iatrogenic hypoglycemia. Prior studies have likely underestimated the incidence of hyperkalemia treatment-associated hypoglycemia as glucose levels are rarely checked within three hours of insulin administration.8 In our study, which was designed to ensure appropriate blood glucose measurement, 21% of insulin treatments for hyperkalemia resulted in hypoglycemia, with 92% of hypoglycemic events occurring within the first three hours.
For the Orderset 1.1 period, patient risk factors identified for iatrogenic hypoglycemia postinsulin administration were female sex, doses of regular insulin greater than 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dL. These results are consistent with studies suggesting that preinsulin blood glucose levels less than 140 mg/dL and the standard 10 units of insulin for hyperkalemia treatment may increase the risk of hypoglycemia.4,7,9
To decrease the risk of iatrogenic hypoglycemia, we redesigned our hyperkalemia insulin orderset to address the strongest predictors of hypoglycemia (doses of regular insulin greater than 0.14 units/kg and preinsulin blood glucose less than 140 mg/dL). The main changes were weight-based insulin dosing (based on previously published data)10 and adjustment of glucose administration based on the patient’s glucose levels.11 Following these changes, the rates of both hypoglycemia and severe hypoglycemia were statistically significantly reduced. In addition, of the 14 hypoglycemia events identified after the introduction of Orderset 1.2, five could have been prevented (36%) had the protocol been strictly followed. These five hypoglycemia events occurred later than one-hour postinsulin administration in patients with blood sugars < 150 mg/dL prior to insulin administration. In each of these cases, Orderset 1.2 called for an additional dextrose 50% (50 mL) IV bolus, which likely would have prevented the subsequently recorded hypoglycemia. In other words, our orderset indicated that these patients received an additional bolus of dextrose. However, they did not receive their glucose at the appropriate time, contributing to the hypoglycemia events. The orderset did not include a best practice alert (BPA) to remind providers about the extra dextrose bolus. In the future, we plan to add this BPA.
The hypoglycemia rate identified by Orderset 1.1 was 21% and the hypoglycemia rate identified by the Orderset 1.2 was 10%. The severe hypoglycemia rate identified by Orderset 1.1 was 5% and the severe hypoglycemia rate identified by Orderset 1.2 was 2%. The hypoglycemia and severe hypoglycemia rates significantly decreased after the introduction of Orderset 1.2. To mimic a real-world clinical setting, where monitoring of blood glucose is not always achieved multiple times within a six-hour timeframe of postinsulin treatment for hyperkalemia, we conducted an intention-to-treat analysis. Even when including patients for whom full blood glucose monitoring was not achieved, the introduction of Orderset 1.2 was associated with a significant decrease in the hypoglycemia rate.
To demonstrate whether weight-based dosing of insulin was as effective as a standard dose for hyperkalemia treatment, we compared the impact of Orderset 1.1, which only had the option for single standard doses of insulin, with the impact of Orderset 1.2, which included weight-based dosing options. With the introduction of Orderset 1.2, there was a significant decrease in serum potassium, indicating that weight-based dosing options may not only prevent hypoglycemia but may potentially provide more effective hyperkalemia treatment.
We also compared the rate of hyperglycemia (a glucose >180 mg/dl) pre- and posttreatment (Table 3). Although not statistically significant, the rate of hyperglycemia decreased from 11% to 6%, suggesting a trend toward decreased hyperglycemia with orderset usage.
As orderset usage for hyperkalemia management only occurred approximately 75% of the time, likely, forcing the use of these ordersets would further reduce the incidence of treatment-associated hypoglycemia. To encourage the use of ordersets for hyperkalemia management, our medical center has largely restricted insulin ordering so that it can only be done through ordersets with the proper precautions in place, regardless of the indication. Furthermore, adherence to all the blood glucose monitoring orders embedded in the ordersets remained suboptimal irrespective of managing the service or clinical setting
Finally, development and implementation of these hyperkalemia treatment ordersets required an experienced multidisciplinary team, including pharmacists, nurses, hospitalists, endocrinologists, and EHR system programmers.12,13 We, therefore, encourage interprofessional collaboration for any institutions seeking to establish innovative clinical protocols.
This analysis was limited to the insulin administration meeting our inclusion criteria. Thus, we could not identify a true hypoglycemia rate for treatments that were not followed by adequate blood glucose monitoring postinsulin administration, or for insulin administration ordered outside of the hyperkalemia ordersets.
CONCLUSION
The use of a comprehensive EHR orderset for the treatment of hyperkalemia with predefined times for blood glucose monitoring, weight-based insulin dosing, and prompts to warn providers of an individual patient’s risk for hypoglycemia may significantly reduce the incidence of iatrogenic hypoglycemia.
1. Acker CG, Johnson JP, Palevsky PM, Greenberg A. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med. 1998;158(8):917-924. https://doi.org/10.1001/archinte.158.8.917.
2. Fordjour KN, Walton T, Doran JJ. Management of hyperkalemia in hospitalized patients. Am J Med Sci. 2014;347(2):93-100. https://doi.org/10.1097/MAJ.0b013e318279b105.
3. Part-10-Special-Circumstances-of-Resuscitation.pdf. https://eccguidelines.heart.org/wp-content/themes/eccstaging/dompdf-master/pdffiles/part-10-special-circumstances-of-resuscitation.pdf. Accessed December 16, 2017.
4. Apel J, Reutrakul S, Baldwin D. Hypoglycemia in the treatment of hyperkalemia with insulin in patients with end-stage renal disease. Clin Kidney J. 2014;7(3):248-250. https://doi.org/10.1093/ckj/sfu026.
5. Schafers S, Naunheim R, Vijayan A, Tobin G. Incidence of hypoglycemia following insulin-based acute stabilization of hyperkalemia treatment. J Hosp Med. 2012;7(3):239-242. https://doi.org/10.1002/jhm.977.
6. Boughton CK, Dixon D, Goble E, et al. Preventing hypoglycemia following treatment of hyperkalemia in hospitalized patients. J Hosp Med. 2019;14:E1-E4. https://doi.org/10.12788/jhm.3145.
7. Wheeler DT, Schafers SJ, Horwedel TA, Deal EN, Tobin GS. Weight-based insulin dosing for acute hyperkalemia results in less hypoglycemia. J Hosp Med. 2016;11(5):355-357. https://doi.org/10.1002/jhm.2545.
8. Coca A, Valencia AL, Bustamante J, Mendiluce A, Floege J. Hypoglycemia following intravenous insulin plus glucose for hyperkalemia in patients with impaired renal function. PLoS ONE. 2017;12(2):e0172961. https://doi.org/10.1371/journal.pone.0172961.
9. LaRue HA, Peksa GD, Shah SC. A comparison of insulin doses for the treatment of hyperkalemia in patients with renal insufficiency. Pharmacotherapy. 2017;37(12):1516-1522. https://doi.org/10.1002/phar.2038.
10. Brown K, Setji TL, Hale SL, et al. Assessing the impact of an order panel utilizing weight-based insulin and standardized monitoring of blood glucose for patients with hyperkalemia. Am J Med Qual. 2018;33(6):598-603. https://doi.org/10.1177/1062860618764610.
11. Farina N, Anderson C. Impact of dextrose dose on hypoglycemia development following treatment of hyperkalemia. Ther Adv Drug Saf. 2018;9(6):323-329. https://doi.org/10.1177/2042098618768725.
12. Neinstein A, MacMaster HW, Sullivan MM, Rushakoff R. A detailed description of the implementation of inpatient insulin orders with a commercial electronic health record system. J Diabetes Sci Technol. 2014;8(4):641-651. https://doi.org/10.1177/1932296814536290.
13. MacMaster HW, Gonzalez S, Maruoka A, et al. Development and implementation of a subcutaneous Insulin pen label bar code scanning protocol to prevent wrong-patient insulin pen errors. Jt Comm J Qual Patient Saf. 2019;45(5):380-386. https://doi.org/10.1016/j.jcjq.2018.08.006.
Hyperkalemia (serum potassium ≥5.1 mEq/L), if left untreated, may result in cardiac arrhythmias, severe muscle weakness, or paralysis.1,2 Insulin administration can rapidly correct hyperkalemia by shifting serum potassiufm intracellularly.3 Treatment of hyperkalemia with insulin may lead to hypoglycemia, which, when severe, can cause confusion, seizures, loss of consciousness, and death. The use of regular and short-acting insulins to correct hyperkalemia quickly in hospitalized patients results in the greatest risk of hypoglycemia within three hours of treatment.4 Nonetheless, monitoring blood glucose levels within six hours of postinsulin administration is not a standard part of hyperkalemia treatment guidelines,3 leaving the rates of hypoglycemia in this setting poorly characterized.
Without standardized blood glucose measurement protocols, retrospective studies have reported posttreatment hypoglycemia rates of 8.7%-17.5% among all patients with hyperkalemia,5,6 and 13% among patients with end-stage renal disease.4 These estimates likely underestimate the true hypoglycemia rates as they measure blood glucose sporadically and are often outside the three-hour window of highest risk after insulin administration.
At the University of California, San Francisco Medical Center (UCSFMC), we faced similar issues in measuring the true hypoglycemia rates associated with hyperkalemia treatment. In December 2015, a 12-month retrospective review revealed a 12% hypoglycemia rate among patients treated with insulin for hyperkalemia. This review was limited by the inclusion of only patients treated for hyperkalemia using the standard orderset supplied with the electronic health record system (EHR; EPIC Systems, Verona, Wisconsin) and the absence of specific orders for glucose monitoring. As a result, more than 40% of these inpatients had no documented glucose within six hours of postinsulin administration.
We subsequently designed and implemented an adult inpatient hyperkalemia treatment orderset aimed at reducing iatrogenic hypoglycemia by promoting appropriate insulin use and blood glucose monitoring during the treatment of hyperkalemia. Through rapid improvement cycles, we iteratively revised the orderset to optimally mitigate the risk of hypoglycemia that was associated with insulin use. We describe implementation and outcomes of weight-based insulin dosing,7 automated alerts to identify patients at greatest risk for hypoglycemia, and clinical decision support based on the preinsulin blood glucose level. We report the rates of iatrogenic hypoglycemia after the implementation of these order-set changes.
METHODS
Design Overview
EHR data were extracted from Epic Clarity. We analyzed data following Orderset 1.1 implementation (January 1, 2016-March 19, 2017) when hypoglycemia rates were reliably quantifiable and following orderset revision 1.2 (March 20, 2017-September 30, 2017) to evaluate the impact of the orderset intervention. The data collection was approved by the Institutional Review Board at the University of California, San Francisco.
Additionally, we explored the frequency in which providers ordered insulin through the hyperkalemia orderset for each version of the orderset via two-month baseline reviews. Investigation for Orderset 1.1 was from January 1, 2017 to February 28, 2017 and for Orderset 1.2 was from August 1, 2017 to September 30, 2017. Insulin ordering frequency through the hyperkalemia orderset was defined as ordering insulin through the adult inpatient hyperkalemia orderset versus ordering insulin in and outside of the hyperkalemia orderset.
Last, we measured the nursing point of care testing (POCT) blood glucose measurement compliance with the hyperkalemia orderset. Nursing utilization acceptance of the hyperkalemia orderset was defined as adequate POCT blood glucose levels monitored in comparison to all insulin treatments via the hyperkalemia orderset.
Setting and Participants
We evaluated nonobstetric adult inpatients admitted to UCSF Medical Center between January 2016 and September 2017. All medical and surgical wards and intensive care units were included in the analysis.
Intervention
In June 2012, an EHR developed by Epic Systems was introduced at UCSFMC. In January 2016, we designed a new EHR-based hyperkalemia treatment orderset (Orderset 1.1), which added standard POCT blood glucose checks before and at one, two, four, and six hours after insulin injection (Appendix 1). In March 2017, a newly designed orderset (Orderset 1.2) replaced the previous hyperkalemia treatment orderset (Appendix 2). Orderset 1.2 included three updates. First, providers were now presented the option of ordering insulin as a
CORRECTED FIGURE PER ERRATUM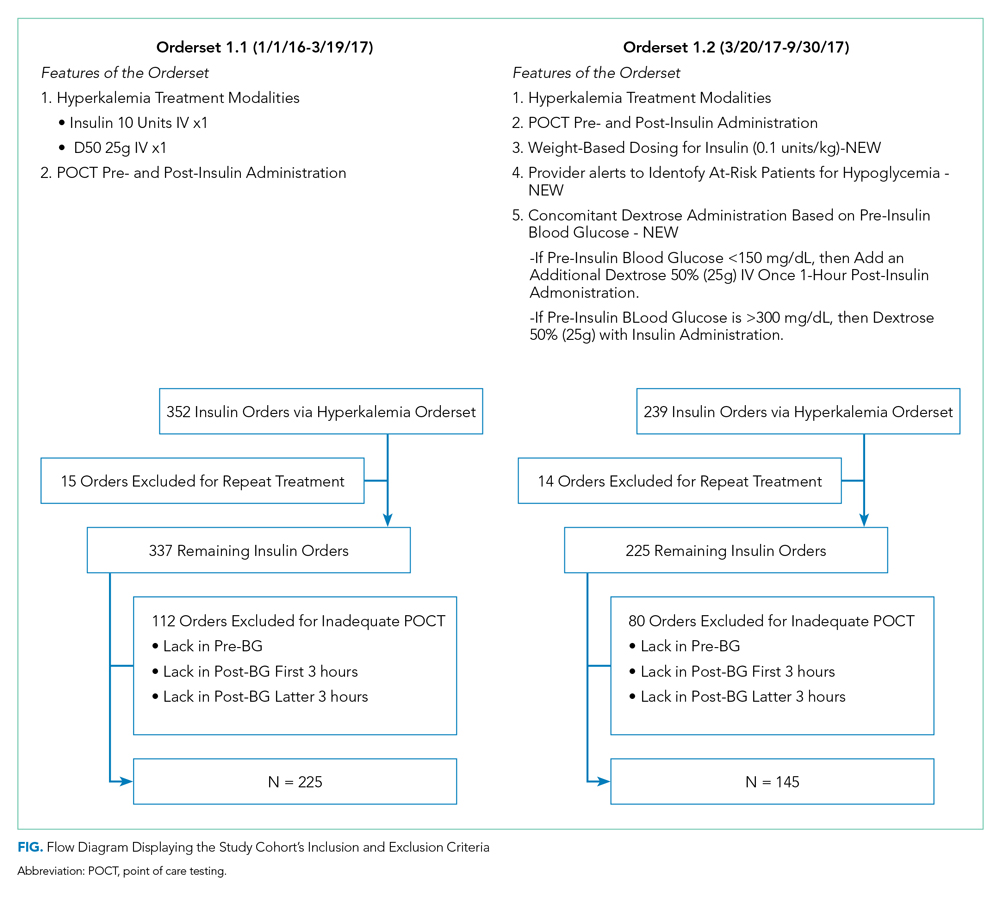
Inclusion and exclusion criteria are shown in the Figure. All patients who had insulin ordered via a hyperkalemia orderset were included in an intention-to-treat analysis. A further analysis was performed for patients for whom orderset compliance was achieved (ie, insulin ordered through the ordersets with adequate blood glucose monitoring). These patients were required to have a POCT blood glucose check preinsulin administration and postinsulin administration as follows: (1) between 30 to 180 minutes (0.5 to three hours) after insulin administration, and (2) between 180 and 360 minutes (three to six hours) after insulin administration. For patients receiving repeated insulin treatments for hyperkalemia within six hours, the first treatment data points were excluded to prevent duplication.
Outcomes
We extracted data on all nonobstetric adult patients admitted to UCSFMC between January 1, 2016 and March 19, 2017 (Orderset 1.1) and between March 20, 2017 and September 30, 2017 (Orderset 1.2).
We measured unique insulin administrations given that each insulin injection poses a risk of iatrogenic hypoglycemia. Hypoglycemia was defined as glucose <70 mg/dL and severe hypoglycemia was defined as glucose <40 mg/dL. Covariates included time and date of insulin administration; blood glucose levels before and at one, two, four, and six hours after insulin injection (if available); sex; weight; dose of insulin given for hyperkalemia treatment; creatinine; known diagnosis of diabetes; concomitant use of albuterol; and concomitant use of corticosteroids. Hyperglycemia was defined as glucose >180 mg/dL. We collected potassium levels pre- and postinsulin treatment. The responsible team’s discipline and the location of the patient (eg, medical/surgical unit, intensive care unit, emergency department) where the insulin orderset was used were recorded.
Statistical Analysis
Statistical analysis for our data included the χ2 test for categorical data and Student t test for continuous data. The bivariate analysis identified potential risk factors and protective factors for hypoglycemia, and logistic regression was used to determine independent predictors of hypoglycemia. Through bivariate analyses, any factor with a P value below .05 was included in the multivariable analyses to investigate a significant contribution to hypoglycemia outcomes. Analyses for hypoglycemia and severe hypoglycemia rates, potassium levels pre- and postinsulin treatment, and hyperglycemia rates were done for both the intention-to-treat group and the group with all criteria met. All analyses were rendered utilizing Stata version 14 (Stata Corp LLC, College Station, Texas).
RESULTS
Baseline patient characteristics, initial insulin dosing, the treatment team, and the location are shown in Table 1. With the implementation of weight-based dosing, a lower dose of insulin was administered with Orderset 1.2 compared with Orderset 1.1.
Orderset adherence rates for Orderset 1.1 and 1.2 were as follows: Acute Care Floor 65% (70%), Intensive Care Unit 63% (66%), and Emergency Department 60% (55%). A two-month audit of orderset usage and compliance revealed that 73% (70 of 96) of insulin treatments were ordered through Orderset 1.1, and 77% (71 of 92) of insulin treatments were ordered through Orderset 1.2. The distribution of orderset usage across location and primary service are shown in Table 1.
The patient distribution is shown in the Figure. In the Orderset 1.1 period, there were 352 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 225 patients for whom compliance with orderset monitoring was achieved. Notably, 112 treatments were excluded for the lack of adequate blood glucose monitoring. In the Orderset 1.2 period, there were 239 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 145 patients for whom compliance with orderset monitoring was achieved. During this phase, 80 treatments were excluded for inadequate blood glucose monitoring.
Predictors of hypoglycemia following the implementation of Orderset 1.1 are shown in Table 2, and the logistic regression model of these risks is shown in Appendix Table 1. Female gender, weight-based dosing of insulin exceeding 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dl were associated with an increased risk of hypoglycemia. A known diagnosis of Type 2 diabetes, concomitant albuterol within one hour of insulin administration, and corticosteroid administration within two hours of insulin administration were associated with a decreased risk of hypoglycemia.
The rates of hypoglycemia (<70 mg/dl) and severe hypoglycemia (<40 mg/dl) are shown in Table 3. During the Orderset 1.1 period,
During the Orderset 1.2 period, for patients with all criteria met, 14 of 145 (10%) had hypoglycemia, and three of 145 (2%) had severe hypoglycemia. Ten of 14 (72%) of these hypoglycemic events occurred in the first three hours, with the remaining four hypoglycemic events (28%) occurring in the last three hours.
An intention-to-treat analysis for hyperglycemia, defined as glucose >180 mg/dl, revealed that during the Orderset 1.1 period, 80 of 352 (23%) had hyperglycemia before insulin administration, and 38 of 352 (11%) had hyperglycemia after insulin administration. During the Orderset 1.2 period, 52 of 239 (22%) had hyperglycemia before insulin administration, and 15 of 239 (6%) had hyperglycemia after insulin administration. Results can be found in Table 3.
Pre- and posttreatment potassium levels are shown in Table 3. An intention-to-treat analysis for potassium reduction postinsulin administration revealed that during the Orderset 1.1 period, there was an absolute reduction of 0.73 mmol/L, while during the Orderset 1.2 period, there was an absolute reduction of 0.95 mmol/L.
DISCUSSION
Treatment of hyperkalemia with insulin may result in significant iatrogenic hypoglycemia. Prior studies have likely underestimated the incidence of hyperkalemia treatment-associated hypoglycemia as glucose levels are rarely checked within three hours of insulin administration.8 In our study, which was designed to ensure appropriate blood glucose measurement, 21% of insulin treatments for hyperkalemia resulted in hypoglycemia, with 92% of hypoglycemic events occurring within the first three hours.
For the Orderset 1.1 period, patient risk factors identified for iatrogenic hypoglycemia postinsulin administration were female sex, doses of regular insulin greater than 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dL. These results are consistent with studies suggesting that preinsulin blood glucose levels less than 140 mg/dL and the standard 10 units of insulin for hyperkalemia treatment may increase the risk of hypoglycemia.4,7,9
To decrease the risk of iatrogenic hypoglycemia, we redesigned our hyperkalemia insulin orderset to address the strongest predictors of hypoglycemia (doses of regular insulin greater than 0.14 units/kg and preinsulin blood glucose less than 140 mg/dL). The main changes were weight-based insulin dosing (based on previously published data)10 and adjustment of glucose administration based on the patient’s glucose levels.11 Following these changes, the rates of both hypoglycemia and severe hypoglycemia were statistically significantly reduced. In addition, of the 14 hypoglycemia events identified after the introduction of Orderset 1.2, five could have been prevented (36%) had the protocol been strictly followed. These five hypoglycemia events occurred later than one-hour postinsulin administration in patients with blood sugars < 150 mg/dL prior to insulin administration. In each of these cases, Orderset 1.2 called for an additional dextrose 50% (50 mL) IV bolus, which likely would have prevented the subsequently recorded hypoglycemia. In other words, our orderset indicated that these patients received an additional bolus of dextrose. However, they did not receive their glucose at the appropriate time, contributing to the hypoglycemia events. The orderset did not include a best practice alert (BPA) to remind providers about the extra dextrose bolus. In the future, we plan to add this BPA.
The hypoglycemia rate identified by Orderset 1.1 was 21% and the hypoglycemia rate identified by the Orderset 1.2 was 10%. The severe hypoglycemia rate identified by Orderset 1.1 was 5% and the severe hypoglycemia rate identified by Orderset 1.2 was 2%. The hypoglycemia and severe hypoglycemia rates significantly decreased after the introduction of Orderset 1.2. To mimic a real-world clinical setting, where monitoring of blood glucose is not always achieved multiple times within a six-hour timeframe of postinsulin treatment for hyperkalemia, we conducted an intention-to-treat analysis. Even when including patients for whom full blood glucose monitoring was not achieved, the introduction of Orderset 1.2 was associated with a significant decrease in the hypoglycemia rate.
To demonstrate whether weight-based dosing of insulin was as effective as a standard dose for hyperkalemia treatment, we compared the impact of Orderset 1.1, which only had the option for single standard doses of insulin, with the impact of Orderset 1.2, which included weight-based dosing options. With the introduction of Orderset 1.2, there was a significant decrease in serum potassium, indicating that weight-based dosing options may not only prevent hypoglycemia but may potentially provide more effective hyperkalemia treatment.
We also compared the rate of hyperglycemia (a glucose >180 mg/dl) pre- and posttreatment (Table 3). Although not statistically significant, the rate of hyperglycemia decreased from 11% to 6%, suggesting a trend toward decreased hyperglycemia with orderset usage.
As orderset usage for hyperkalemia management only occurred approximately 75% of the time, likely, forcing the use of these ordersets would further reduce the incidence of treatment-associated hypoglycemia. To encourage the use of ordersets for hyperkalemia management, our medical center has largely restricted insulin ordering so that it can only be done through ordersets with the proper precautions in place, regardless of the indication. Furthermore, adherence to all the blood glucose monitoring orders embedded in the ordersets remained suboptimal irrespective of managing the service or clinical setting
Finally, development and implementation of these hyperkalemia treatment ordersets required an experienced multidisciplinary team, including pharmacists, nurses, hospitalists, endocrinologists, and EHR system programmers.12,13 We, therefore, encourage interprofessional collaboration for any institutions seeking to establish innovative clinical protocols.
This analysis was limited to the insulin administration meeting our inclusion criteria. Thus, we could not identify a true hypoglycemia rate for treatments that were not followed by adequate blood glucose monitoring postinsulin administration, or for insulin administration ordered outside of the hyperkalemia ordersets.
CONCLUSION
The use of a comprehensive EHR orderset for the treatment of hyperkalemia with predefined times for blood glucose monitoring, weight-based insulin dosing, and prompts to warn providers of an individual patient’s risk for hypoglycemia may significantly reduce the incidence of iatrogenic hypoglycemia.
Hyperkalemia (serum potassium ≥5.1 mEq/L), if left untreated, may result in cardiac arrhythmias, severe muscle weakness, or paralysis.1,2 Insulin administration can rapidly correct hyperkalemia by shifting serum potassiufm intracellularly.3 Treatment of hyperkalemia with insulin may lead to hypoglycemia, which, when severe, can cause confusion, seizures, loss of consciousness, and death. The use of regular and short-acting insulins to correct hyperkalemia quickly in hospitalized patients results in the greatest risk of hypoglycemia within three hours of treatment.4 Nonetheless, monitoring blood glucose levels within six hours of postinsulin administration is not a standard part of hyperkalemia treatment guidelines,3 leaving the rates of hypoglycemia in this setting poorly characterized.
Without standardized blood glucose measurement protocols, retrospective studies have reported posttreatment hypoglycemia rates of 8.7%-17.5% among all patients with hyperkalemia,5,6 and 13% among patients with end-stage renal disease.4 These estimates likely underestimate the true hypoglycemia rates as they measure blood glucose sporadically and are often outside the three-hour window of highest risk after insulin administration.
At the University of California, San Francisco Medical Center (UCSFMC), we faced similar issues in measuring the true hypoglycemia rates associated with hyperkalemia treatment. In December 2015, a 12-month retrospective review revealed a 12% hypoglycemia rate among patients treated with insulin for hyperkalemia. This review was limited by the inclusion of only patients treated for hyperkalemia using the standard orderset supplied with the electronic health record system (EHR; EPIC Systems, Verona, Wisconsin) and the absence of specific orders for glucose monitoring. As a result, more than 40% of these inpatients had no documented glucose within six hours of postinsulin administration.
We subsequently designed and implemented an adult inpatient hyperkalemia treatment orderset aimed at reducing iatrogenic hypoglycemia by promoting appropriate insulin use and blood glucose monitoring during the treatment of hyperkalemia. Through rapid improvement cycles, we iteratively revised the orderset to optimally mitigate the risk of hypoglycemia that was associated with insulin use. We describe implementation and outcomes of weight-based insulin dosing,7 automated alerts to identify patients at greatest risk for hypoglycemia, and clinical decision support based on the preinsulin blood glucose level. We report the rates of iatrogenic hypoglycemia after the implementation of these order-set changes.
METHODS
Design Overview
EHR data were extracted from Epic Clarity. We analyzed data following Orderset 1.1 implementation (January 1, 2016-March 19, 2017) when hypoglycemia rates were reliably quantifiable and following orderset revision 1.2 (March 20, 2017-September 30, 2017) to evaluate the impact of the orderset intervention. The data collection was approved by the Institutional Review Board at the University of California, San Francisco.
Additionally, we explored the frequency in which providers ordered insulin through the hyperkalemia orderset for each version of the orderset via two-month baseline reviews. Investigation for Orderset 1.1 was from January 1, 2017 to February 28, 2017 and for Orderset 1.2 was from August 1, 2017 to September 30, 2017. Insulin ordering frequency through the hyperkalemia orderset was defined as ordering insulin through the adult inpatient hyperkalemia orderset versus ordering insulin in and outside of the hyperkalemia orderset.
Last, we measured the nursing point of care testing (POCT) blood glucose measurement compliance with the hyperkalemia orderset. Nursing utilization acceptance of the hyperkalemia orderset was defined as adequate POCT blood glucose levels monitored in comparison to all insulin treatments via the hyperkalemia orderset.
Setting and Participants
We evaluated nonobstetric adult inpatients admitted to UCSF Medical Center between January 2016 and September 2017. All medical and surgical wards and intensive care units were included in the analysis.
Intervention
In June 2012, an EHR developed by Epic Systems was introduced at UCSFMC. In January 2016, we designed a new EHR-based hyperkalemia treatment orderset (Orderset 1.1), which added standard POCT blood glucose checks before and at one, two, four, and six hours after insulin injection (Appendix 1). In March 2017, a newly designed orderset (Orderset 1.2) replaced the previous hyperkalemia treatment orderset (Appendix 2). Orderset 1.2 included three updates. First, providers were now presented the option of ordering insulin as a
CORRECTED FIGURE PER ERRATUM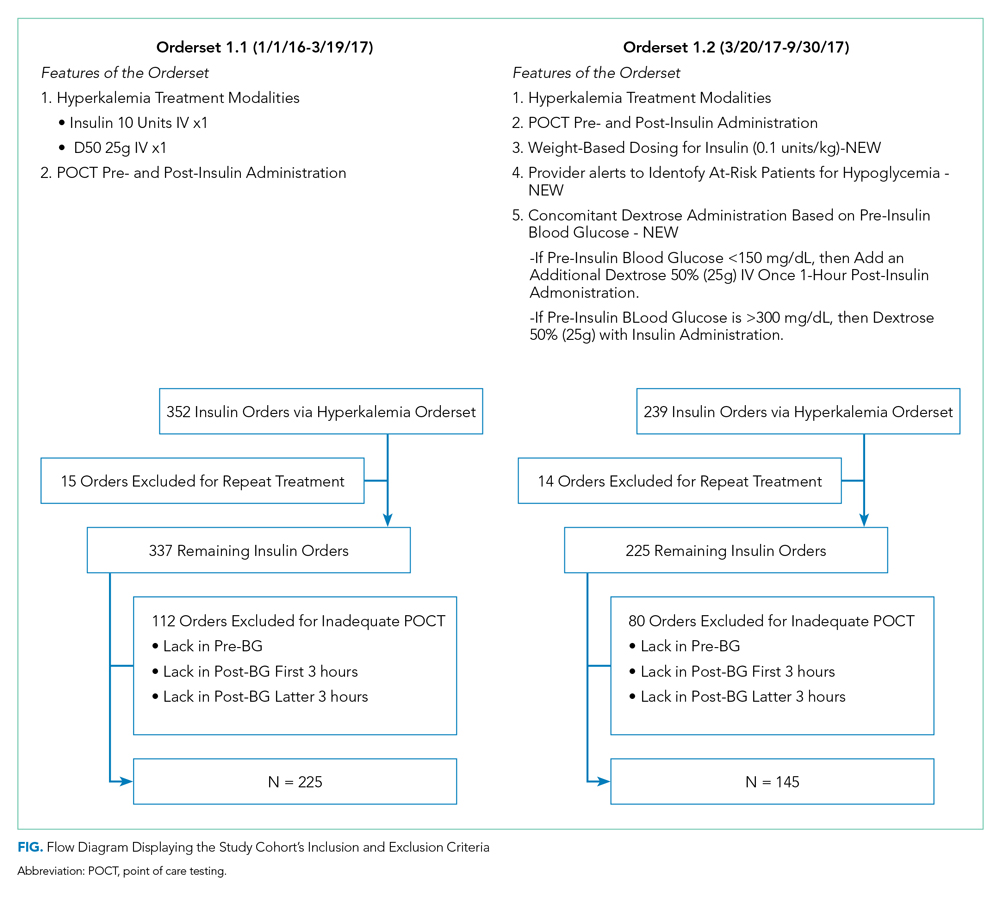
Inclusion and exclusion criteria are shown in the Figure. All patients who had insulin ordered via a hyperkalemia orderset were included in an intention-to-treat analysis. A further analysis was performed for patients for whom orderset compliance was achieved (ie, insulin ordered through the ordersets with adequate blood glucose monitoring). These patients were required to have a POCT blood glucose check preinsulin administration and postinsulin administration as follows: (1) between 30 to 180 minutes (0.5 to three hours) after insulin administration, and (2) between 180 and 360 minutes (three to six hours) after insulin administration. For patients receiving repeated insulin treatments for hyperkalemia within six hours, the first treatment data points were excluded to prevent duplication.
Outcomes
We extracted data on all nonobstetric adult patients admitted to UCSFMC between January 1, 2016 and March 19, 2017 (Orderset 1.1) and between March 20, 2017 and September 30, 2017 (Orderset 1.2).
We measured unique insulin administrations given that each insulin injection poses a risk of iatrogenic hypoglycemia. Hypoglycemia was defined as glucose <70 mg/dL and severe hypoglycemia was defined as glucose <40 mg/dL. Covariates included time and date of insulin administration; blood glucose levels before and at one, two, four, and six hours after insulin injection (if available); sex; weight; dose of insulin given for hyperkalemia treatment; creatinine; known diagnosis of diabetes; concomitant use of albuterol; and concomitant use of corticosteroids. Hyperglycemia was defined as glucose >180 mg/dL. We collected potassium levels pre- and postinsulin treatment. The responsible team’s discipline and the location of the patient (eg, medical/surgical unit, intensive care unit, emergency department) where the insulin orderset was used were recorded.
Statistical Analysis
Statistical analysis for our data included the χ2 test for categorical data and Student t test for continuous data. The bivariate analysis identified potential risk factors and protective factors for hypoglycemia, and logistic regression was used to determine independent predictors of hypoglycemia. Through bivariate analyses, any factor with a P value below .05 was included in the multivariable analyses to investigate a significant contribution to hypoglycemia outcomes. Analyses for hypoglycemia and severe hypoglycemia rates, potassium levels pre- and postinsulin treatment, and hyperglycemia rates were done for both the intention-to-treat group and the group with all criteria met. All analyses were rendered utilizing Stata version 14 (Stata Corp LLC, College Station, Texas).
RESULTS
Baseline patient characteristics, initial insulin dosing, the treatment team, and the location are shown in Table 1. With the implementation of weight-based dosing, a lower dose of insulin was administered with Orderset 1.2 compared with Orderset 1.1.
Orderset adherence rates for Orderset 1.1 and 1.2 were as follows: Acute Care Floor 65% (70%), Intensive Care Unit 63% (66%), and Emergency Department 60% (55%). A two-month audit of orderset usage and compliance revealed that 73% (70 of 96) of insulin treatments were ordered through Orderset 1.1, and 77% (71 of 92) of insulin treatments were ordered through Orderset 1.2. The distribution of orderset usage across location and primary service are shown in Table 1.
The patient distribution is shown in the Figure. In the Orderset 1.1 period, there were 352 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 225 patients for whom compliance with orderset monitoring was achieved. Notably, 112 treatments were excluded for the lack of adequate blood glucose monitoring. In the Orderset 1.2 period, there were 239 total insulin treatments utilizing the newly revised UCSFMC adult inpatient hyperkalemia orderset that were used for the intention-to-treat analysis, and there were 145 patients for whom compliance with orderset monitoring was achieved. During this phase, 80 treatments were excluded for inadequate blood glucose monitoring.
Predictors of hypoglycemia following the implementation of Orderset 1.1 are shown in Table 2, and the logistic regression model of these risks is shown in Appendix Table 1. Female gender, weight-based dosing of insulin exceeding 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dl were associated with an increased risk of hypoglycemia. A known diagnosis of Type 2 diabetes, concomitant albuterol within one hour of insulin administration, and corticosteroid administration within two hours of insulin administration were associated with a decreased risk of hypoglycemia.
The rates of hypoglycemia (<70 mg/dl) and severe hypoglycemia (<40 mg/dl) are shown in Table 3. During the Orderset 1.1 period,
During the Orderset 1.2 period, for patients with all criteria met, 14 of 145 (10%) had hypoglycemia, and three of 145 (2%) had severe hypoglycemia. Ten of 14 (72%) of these hypoglycemic events occurred in the first three hours, with the remaining four hypoglycemic events (28%) occurring in the last three hours.
An intention-to-treat analysis for hyperglycemia, defined as glucose >180 mg/dl, revealed that during the Orderset 1.1 period, 80 of 352 (23%) had hyperglycemia before insulin administration, and 38 of 352 (11%) had hyperglycemia after insulin administration. During the Orderset 1.2 period, 52 of 239 (22%) had hyperglycemia before insulin administration, and 15 of 239 (6%) had hyperglycemia after insulin administration. Results can be found in Table 3.
Pre- and posttreatment potassium levels are shown in Table 3. An intention-to-treat analysis for potassium reduction postinsulin administration revealed that during the Orderset 1.1 period, there was an absolute reduction of 0.73 mmol/L, while during the Orderset 1.2 period, there was an absolute reduction of 0.95 mmol/L.
DISCUSSION
Treatment of hyperkalemia with insulin may result in significant iatrogenic hypoglycemia. Prior studies have likely underestimated the incidence of hyperkalemia treatment-associated hypoglycemia as glucose levels are rarely checked within three hours of insulin administration.8 In our study, which was designed to ensure appropriate blood glucose measurement, 21% of insulin treatments for hyperkalemia resulted in hypoglycemia, with 92% of hypoglycemic events occurring within the first three hours.
For the Orderset 1.1 period, patient risk factors identified for iatrogenic hypoglycemia postinsulin administration were female sex, doses of regular insulin greater than 0.14 units/kg, preinsulin blood glucose less than 140 mg/dL, and serum creatinine greater than 2.5 mg/dL. These results are consistent with studies suggesting that preinsulin blood glucose levels less than 140 mg/dL and the standard 10 units of insulin for hyperkalemia treatment may increase the risk of hypoglycemia.4,7,9
To decrease the risk of iatrogenic hypoglycemia, we redesigned our hyperkalemia insulin orderset to address the strongest predictors of hypoglycemia (doses of regular insulin greater than 0.14 units/kg and preinsulin blood glucose less than 140 mg/dL). The main changes were weight-based insulin dosing (based on previously published data)10 and adjustment of glucose administration based on the patient’s glucose levels.11 Following these changes, the rates of both hypoglycemia and severe hypoglycemia were statistically significantly reduced. In addition, of the 14 hypoglycemia events identified after the introduction of Orderset 1.2, five could have been prevented (36%) had the protocol been strictly followed. These five hypoglycemia events occurred later than one-hour postinsulin administration in patients with blood sugars < 150 mg/dL prior to insulin administration. In each of these cases, Orderset 1.2 called for an additional dextrose 50% (50 mL) IV bolus, which likely would have prevented the subsequently recorded hypoglycemia. In other words, our orderset indicated that these patients received an additional bolus of dextrose. However, they did not receive their glucose at the appropriate time, contributing to the hypoglycemia events. The orderset did not include a best practice alert (BPA) to remind providers about the extra dextrose bolus. In the future, we plan to add this BPA.
The hypoglycemia rate identified by Orderset 1.1 was 21% and the hypoglycemia rate identified by the Orderset 1.2 was 10%. The severe hypoglycemia rate identified by Orderset 1.1 was 5% and the severe hypoglycemia rate identified by Orderset 1.2 was 2%. The hypoglycemia and severe hypoglycemia rates significantly decreased after the introduction of Orderset 1.2. To mimic a real-world clinical setting, where monitoring of blood glucose is not always achieved multiple times within a six-hour timeframe of postinsulin treatment for hyperkalemia, we conducted an intention-to-treat analysis. Even when including patients for whom full blood glucose monitoring was not achieved, the introduction of Orderset 1.2 was associated with a significant decrease in the hypoglycemia rate.
To demonstrate whether weight-based dosing of insulin was as effective as a standard dose for hyperkalemia treatment, we compared the impact of Orderset 1.1, which only had the option for single standard doses of insulin, with the impact of Orderset 1.2, which included weight-based dosing options. With the introduction of Orderset 1.2, there was a significant decrease in serum potassium, indicating that weight-based dosing options may not only prevent hypoglycemia but may potentially provide more effective hyperkalemia treatment.
We also compared the rate of hyperglycemia (a glucose >180 mg/dl) pre- and posttreatment (Table 3). Although not statistically significant, the rate of hyperglycemia decreased from 11% to 6%, suggesting a trend toward decreased hyperglycemia with orderset usage.
As orderset usage for hyperkalemia management only occurred approximately 75% of the time, likely, forcing the use of these ordersets would further reduce the incidence of treatment-associated hypoglycemia. To encourage the use of ordersets for hyperkalemia management, our medical center has largely restricted insulin ordering so that it can only be done through ordersets with the proper precautions in place, regardless of the indication. Furthermore, adherence to all the blood glucose monitoring orders embedded in the ordersets remained suboptimal irrespective of managing the service or clinical setting
Finally, development and implementation of these hyperkalemia treatment ordersets required an experienced multidisciplinary team, including pharmacists, nurses, hospitalists, endocrinologists, and EHR system programmers.12,13 We, therefore, encourage interprofessional collaboration for any institutions seeking to establish innovative clinical protocols.
This analysis was limited to the insulin administration meeting our inclusion criteria. Thus, we could not identify a true hypoglycemia rate for treatments that were not followed by adequate blood glucose monitoring postinsulin administration, or for insulin administration ordered outside of the hyperkalemia ordersets.
CONCLUSION
The use of a comprehensive EHR orderset for the treatment of hyperkalemia with predefined times for blood glucose monitoring, weight-based insulin dosing, and prompts to warn providers of an individual patient’s risk for hypoglycemia may significantly reduce the incidence of iatrogenic hypoglycemia.
1. Acker CG, Johnson JP, Palevsky PM, Greenberg A. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med. 1998;158(8):917-924. https://doi.org/10.1001/archinte.158.8.917.
2. Fordjour KN, Walton T, Doran JJ. Management of hyperkalemia in hospitalized patients. Am J Med Sci. 2014;347(2):93-100. https://doi.org/10.1097/MAJ.0b013e318279b105.
3. Part-10-Special-Circumstances-of-Resuscitation.pdf. https://eccguidelines.heart.org/wp-content/themes/eccstaging/dompdf-master/pdffiles/part-10-special-circumstances-of-resuscitation.pdf. Accessed December 16, 2017.
4. Apel J, Reutrakul S, Baldwin D. Hypoglycemia in the treatment of hyperkalemia with insulin in patients with end-stage renal disease. Clin Kidney J. 2014;7(3):248-250. https://doi.org/10.1093/ckj/sfu026.
5. Schafers S, Naunheim R, Vijayan A, Tobin G. Incidence of hypoglycemia following insulin-based acute stabilization of hyperkalemia treatment. J Hosp Med. 2012;7(3):239-242. https://doi.org/10.1002/jhm.977.
6. Boughton CK, Dixon D, Goble E, et al. Preventing hypoglycemia following treatment of hyperkalemia in hospitalized patients. J Hosp Med. 2019;14:E1-E4. https://doi.org/10.12788/jhm.3145.
7. Wheeler DT, Schafers SJ, Horwedel TA, Deal EN, Tobin GS. Weight-based insulin dosing for acute hyperkalemia results in less hypoglycemia. J Hosp Med. 2016;11(5):355-357. https://doi.org/10.1002/jhm.2545.
8. Coca A, Valencia AL, Bustamante J, Mendiluce A, Floege J. Hypoglycemia following intravenous insulin plus glucose for hyperkalemia in patients with impaired renal function. PLoS ONE. 2017;12(2):e0172961. https://doi.org/10.1371/journal.pone.0172961.
9. LaRue HA, Peksa GD, Shah SC. A comparison of insulin doses for the treatment of hyperkalemia in patients with renal insufficiency. Pharmacotherapy. 2017;37(12):1516-1522. https://doi.org/10.1002/phar.2038.
10. Brown K, Setji TL, Hale SL, et al. Assessing the impact of an order panel utilizing weight-based insulin and standardized monitoring of blood glucose for patients with hyperkalemia. Am J Med Qual. 2018;33(6):598-603. https://doi.org/10.1177/1062860618764610.
11. Farina N, Anderson C. Impact of dextrose dose on hypoglycemia development following treatment of hyperkalemia. Ther Adv Drug Saf. 2018;9(6):323-329. https://doi.org/10.1177/2042098618768725.
12. Neinstein A, MacMaster HW, Sullivan MM, Rushakoff R. A detailed description of the implementation of inpatient insulin orders with a commercial electronic health record system. J Diabetes Sci Technol. 2014;8(4):641-651. https://doi.org/10.1177/1932296814536290.
13. MacMaster HW, Gonzalez S, Maruoka A, et al. Development and implementation of a subcutaneous Insulin pen label bar code scanning protocol to prevent wrong-patient insulin pen errors. Jt Comm J Qual Patient Saf. 2019;45(5):380-386. https://doi.org/10.1016/j.jcjq.2018.08.006.
1. Acker CG, Johnson JP, Palevsky PM, Greenberg A. Hyperkalemia in hospitalized patients: causes, adequacy of treatment, and results of an attempt to improve physician compliance with published therapy guidelines. Arch Intern Med. 1998;158(8):917-924. https://doi.org/10.1001/archinte.158.8.917.
2. Fordjour KN, Walton T, Doran JJ. Management of hyperkalemia in hospitalized patients. Am J Med Sci. 2014;347(2):93-100. https://doi.org/10.1097/MAJ.0b013e318279b105.
3. Part-10-Special-Circumstances-of-Resuscitation.pdf. https://eccguidelines.heart.org/wp-content/themes/eccstaging/dompdf-master/pdffiles/part-10-special-circumstances-of-resuscitation.pdf. Accessed December 16, 2017.
4. Apel J, Reutrakul S, Baldwin D. Hypoglycemia in the treatment of hyperkalemia with insulin in patients with end-stage renal disease. Clin Kidney J. 2014;7(3):248-250. https://doi.org/10.1093/ckj/sfu026.
5. Schafers S, Naunheim R, Vijayan A, Tobin G. Incidence of hypoglycemia following insulin-based acute stabilization of hyperkalemia treatment. J Hosp Med. 2012;7(3):239-242. https://doi.org/10.1002/jhm.977.
6. Boughton CK, Dixon D, Goble E, et al. Preventing hypoglycemia following treatment of hyperkalemia in hospitalized patients. J Hosp Med. 2019;14:E1-E4. https://doi.org/10.12788/jhm.3145.
7. Wheeler DT, Schafers SJ, Horwedel TA, Deal EN, Tobin GS. Weight-based insulin dosing for acute hyperkalemia results in less hypoglycemia. J Hosp Med. 2016;11(5):355-357. https://doi.org/10.1002/jhm.2545.
8. Coca A, Valencia AL, Bustamante J, Mendiluce A, Floege J. Hypoglycemia following intravenous insulin plus glucose for hyperkalemia in patients with impaired renal function. PLoS ONE. 2017;12(2):e0172961. https://doi.org/10.1371/journal.pone.0172961.
9. LaRue HA, Peksa GD, Shah SC. A comparison of insulin doses for the treatment of hyperkalemia in patients with renal insufficiency. Pharmacotherapy. 2017;37(12):1516-1522. https://doi.org/10.1002/phar.2038.
10. Brown K, Setji TL, Hale SL, et al. Assessing the impact of an order panel utilizing weight-based insulin and standardized monitoring of blood glucose for patients with hyperkalemia. Am J Med Qual. 2018;33(6):598-603. https://doi.org/10.1177/1062860618764610.
11. Farina N, Anderson C. Impact of dextrose dose on hypoglycemia development following treatment of hyperkalemia. Ther Adv Drug Saf. 2018;9(6):323-329. https://doi.org/10.1177/2042098618768725.
12. Neinstein A, MacMaster HW, Sullivan MM, Rushakoff R. A detailed description of the implementation of inpatient insulin orders with a commercial electronic health record system. J Diabetes Sci Technol. 2014;8(4):641-651. https://doi.org/10.1177/1932296814536290.
13. MacMaster HW, Gonzalez S, Maruoka A, et al. Development and implementation of a subcutaneous Insulin pen label bar code scanning protocol to prevent wrong-patient insulin pen errors. Jt Comm J Qual Patient Saf. 2019;45(5):380-386. https://doi.org/10.1016/j.jcjq.2018.08.006.
© 2020 Society of Hospital Medicine
New medical ethics series debuts
Dear colleagues,
The first issue of The New Gastroenterologist in 2020 consists of a particularly interesting array of articles and the introduction of a new medical ethics series!
This month’s “In Focus” article, brought to you by Jennifer Maratt (Indiana University) and Elena Stoffel (University of Michigan), provides a high yield overview of hereditary colorectal cancer and polyposis syndromes, with guidance on when a referral to a high risk cancer specialist and geneticist is warranted.
Daniel Mills (Cunningham, Meyer & Vedrine P.C.) gives us a valuable legal perspective of the role of electronic patient portals in the dissemination of information and medical advice to patients – such an important topic for everyone to be aware of as the nature of patient communication now strongly relies on electronic messaging.
R. Thomas Finn III (Palo Alto Medical Foundation) and David Leiman (Duke) nicely broach the issue of patient satisfaction. This is a timely topic as many institutions are not only publishing patient reviews online so that they are readily available to the public, but are also making financial incentives contingent on high patient ratings. The article discusses the evolution of the emphasis placed on patient satisfaction throughout the years with tips on how to navigate some of the distinct challenges within gastroenterology.
As part of our DHPA Private Practice Perspectives series, David Stokesberry (Digestive Disease Specialists Inc, Oklahoma City) discusses the nuts and bolts of ambulatory endoscopy centers and some of the challenges and benefits that accompany ownership of such centers.
An often overlooked aspect of gastroenterology training is nutrition. In our postfellowship pathways section, Dejan Micic (University of Chicago) outlines his decision to pursue a career in nutrition support, small bowel disorders, and the practice of deep enteroscopy.
Finally, this quarter’s newsletter features the start of a new section, which I am very excited to introduce – a case based series which will address issues in clinical medical ethics specific to gastroenterology. Lauren Feld (University of Washington) writes the inaugural piece for the section, providing a systematic approach to the patient with an existing do-not-resuscitate (DNR) order that is about to undergo endoscopy.
If you have interest in contributing or have ideas for future TNG topics, please contact me (vijayarao@medicine.bsd.uchicago.edu), or Ryan Farrell (rfarrell@gastro.org), managing editor of TNG.
Sincerely,
Vijaya L. Rao, MD
Editor in Chief
Dear colleagues,
The first issue of The New Gastroenterologist in 2020 consists of a particularly interesting array of articles and the introduction of a new medical ethics series!
This month’s “In Focus” article, brought to you by Jennifer Maratt (Indiana University) and Elena Stoffel (University of Michigan), provides a high yield overview of hereditary colorectal cancer and polyposis syndromes, with guidance on when a referral to a high risk cancer specialist and geneticist is warranted.
Daniel Mills (Cunningham, Meyer & Vedrine P.C.) gives us a valuable legal perspective of the role of electronic patient portals in the dissemination of information and medical advice to patients – such an important topic for everyone to be aware of as the nature of patient communication now strongly relies on electronic messaging.
R. Thomas Finn III (Palo Alto Medical Foundation) and David Leiman (Duke) nicely broach the issue of patient satisfaction. This is a timely topic as many institutions are not only publishing patient reviews online so that they are readily available to the public, but are also making financial incentives contingent on high patient ratings. The article discusses the evolution of the emphasis placed on patient satisfaction throughout the years with tips on how to navigate some of the distinct challenges within gastroenterology.
As part of our DHPA Private Practice Perspectives series, David Stokesberry (Digestive Disease Specialists Inc, Oklahoma City) discusses the nuts and bolts of ambulatory endoscopy centers and some of the challenges and benefits that accompany ownership of such centers.
An often overlooked aspect of gastroenterology training is nutrition. In our postfellowship pathways section, Dejan Micic (University of Chicago) outlines his decision to pursue a career in nutrition support, small bowel disorders, and the practice of deep enteroscopy.
Finally, this quarter’s newsletter features the start of a new section, which I am very excited to introduce – a case based series which will address issues in clinical medical ethics specific to gastroenterology. Lauren Feld (University of Washington) writes the inaugural piece for the section, providing a systematic approach to the patient with an existing do-not-resuscitate (DNR) order that is about to undergo endoscopy.
If you have interest in contributing or have ideas for future TNG topics, please contact me (vijayarao@medicine.bsd.uchicago.edu), or Ryan Farrell (rfarrell@gastro.org), managing editor of TNG.
Sincerely,
Vijaya L. Rao, MD
Editor in Chief
Dear colleagues,
The first issue of The New Gastroenterologist in 2020 consists of a particularly interesting array of articles and the introduction of a new medical ethics series!
This month’s “In Focus” article, brought to you by Jennifer Maratt (Indiana University) and Elena Stoffel (University of Michigan), provides a high yield overview of hereditary colorectal cancer and polyposis syndromes, with guidance on when a referral to a high risk cancer specialist and geneticist is warranted.
Daniel Mills (Cunningham, Meyer & Vedrine P.C.) gives us a valuable legal perspective of the role of electronic patient portals in the dissemination of information and medical advice to patients – such an important topic for everyone to be aware of as the nature of patient communication now strongly relies on electronic messaging.
R. Thomas Finn III (Palo Alto Medical Foundation) and David Leiman (Duke) nicely broach the issue of patient satisfaction. This is a timely topic as many institutions are not only publishing patient reviews online so that they are readily available to the public, but are also making financial incentives contingent on high patient ratings. The article discusses the evolution of the emphasis placed on patient satisfaction throughout the years with tips on how to navigate some of the distinct challenges within gastroenterology.
As part of our DHPA Private Practice Perspectives series, David Stokesberry (Digestive Disease Specialists Inc, Oklahoma City) discusses the nuts and bolts of ambulatory endoscopy centers and some of the challenges and benefits that accompany ownership of such centers.
An often overlooked aspect of gastroenterology training is nutrition. In our postfellowship pathways section, Dejan Micic (University of Chicago) outlines his decision to pursue a career in nutrition support, small bowel disorders, and the practice of deep enteroscopy.
Finally, this quarter’s newsletter features the start of a new section, which I am very excited to introduce – a case based series which will address issues in clinical medical ethics specific to gastroenterology. Lauren Feld (University of Washington) writes the inaugural piece for the section, providing a systematic approach to the patient with an existing do-not-resuscitate (DNR) order that is about to undergo endoscopy.
If you have interest in contributing or have ideas for future TNG topics, please contact me (vijayarao@medicine.bsd.uchicago.edu), or Ryan Farrell (rfarrell@gastro.org), managing editor of TNG.
Sincerely,
Vijaya L. Rao, MD
Editor in Chief
Colorectal polyps and cancer – when to refer to genetics
Introduction
Genetic predisposition to colorectal polyps and colorectal cancer (CRC) is more common than previously recognized. Approximately 5%-10% of all individuals diagnosed with CRC have a known genetic association. However, among those with early-onset CRC (diagnosed at age less than 50 years), recent studies show that up to 20% have an associated genetic mutation.1,2 In addition, the risk of CRC in patients with certain hereditary syndromes, such as familial adenomatous polyposis (FAP), approaches 80%-90% without timely management.3 This overall high risk of CRC and extracolonic malignancies in patients with a hereditary syndrome, along with the rising rates of early-onset CRC, underscores the importance of early diagnosis and management of a hereditary condition.
Despite increasing awareness of hereditary polyposis and nonpolyposis syndromes, referral rates for genetic counseling and testing remain low.4 As gastroenterologists we have several unique opportunities, in clinic and in endoscopy, to identify patients at risk for hereditary syndromes.
Risk stratification
Personal and family history
Reviewing personal medical history and family history in detail should be a routine part of our practice. This is often when initial signs of a potential hereditary syndrome can be detected. For example, if a patient reports a personal or family history of colorectal polyps or CRC, additional information that becomes important includes age at time of diagnosis, polyp burden (number and histologic subtype), presence of inflammatory bowel disease, and history of any extracolonic malignancies. Patients with multiple colorectal polyps (e.g. more than 10-20 adenomas or more than 2 hamartomas) and those with CRC diagnosed at a young age (younger than 50 years) should be considered candidates for genetic evaluation.5
Lynch syndrome (LS), an autosomal dominant condition caused by loss of DNA mismatch repair (MMR) genes, is the most common hereditary CRC syndrome, accounting for 2%-4% of all CRCs.3,6 Extracolonic LS-associated cancers to keep in mind while reviewing personal and family histories include those involving the gastrointestinal (GI) tract such as gastric, pancreatic, biliary tract, and small intestine cancers, and also non-GI tract cancers including endometrial, ovarian, urinary tract, and renal cancers along with brain tumors, and skin lesions including sebaceous adenomas, sebaceous carcinomas, and keratoacanthomas. Notably, after CRC, endometrial cancer is the second most common cancer among women with LS. Prior diagnosis of endometrial cancer should also prompt additional history-taking and evaluation for LS.
As the National Comprehensive Cancer Network (NCCN) highlights in its recent guidelines, several key findings in family history that should prompt referral to genetics for evaluation and testing for LS include: one or more first-degree relatives (FDR) with CRC or endometrial cancer diagnosed at less than 50 years of age, one or more FDR with CRC or endometrial cancer and another synchronous or metachronous LS-related cancer, two or more FDR or second-degree relatives (SDR) with LS-related cancer (including at least one diagnosed at age less than 50 years), and three or more FDR or SDR with LS-related cancers (regardless of age).5
Comprehensive assessment of family history should include all cancer diagnoses in first- and second-degree relatives, including age at diagnosis and cancer type, as well as ethnicity, as these inform the likelihood that the patient harbors a germline pathogenic variant associated with cancer predisposition.5 Given the difficulty of eliciting this level of detail, the family histories elicited in clinical settings are often limited or incomplete. Unknown family history should not be mistaken for unremarkable family history. Alternatively, if family history is unimpressive, this is not necessarily reassuring, as there can be variability in disease penetrance, including autosomal recessive syndromes that may skip generations, and de novo mutations do occur. In fact, among individuals with early-onset CRC diagnosed at age less than 50, only half of mutation carriers reported a family history of CRC in an FDR.2 Thus, individuals with concerning personal histories should undergo a genetic evaluation even if family history is not concerning.
Polyp phenotype
In addition to personal and family history, colon polyp history (including number, size, and histology) can provide important clues to identifying individuals with genetic predisposition to CRC. Table 1 highlights hereditary syndromes and polyp phenotypes associated with increased CRC risk. Based on consensus guidelines, individuals with a history of greater than 10-20 adenomas, 2 or more hamartomas, or 5 or more sessile serrated polyps should be referred for genetic testing.5,7 Serrated polyposis syndrome (SPS) is diagnosed based on at least one of the following criteria: 1) 5 or more serrated polyps, all at least 5 mm in size, proximal to the rectum including at least 2 that are 10 mm or larger in size, or 2) more than 20 serrated polyps distributed throughout the colon with at least 5 proximal to the rectum.8 Pathogenic germline variants in RNF43, a tumor suppressor gene, have been associated with SPS in rare families; however, in most cases genetic testing is uninformative and further genetic and environmental discovery studies are needed to determine the underlying cause.8,9

Risk prediction models
Models have been developed that integrate family history and phenotype data to help identify patients who may be at risk for LS. The Amsterdam criteria (more than 3 relatives with LS-associated cancers, more than 2 generations involving LS-associated cancers, and more than 1 cancer diagnosed before the age of 50; “3:2:1” criteria) were initially developed for research purposes to identify individuals who were likely to be carriers of mutations of LS based on CRC and later revised to include extracolonic malignancies (Amsterdam II).11 However, they have limited sensitivity for identifying high-risk patients. Similarly, the Bethesda guidelines have also been modified and revised to identify patients at risk for LS whose tumors should be tested with microsatellite instability (MSI), but also with limited sensitivity.12
Several risk prediction models have been developed that perform better than the Amsterdam criteria or Bethesda guidelines for determining which patients should be referred for genetic testing for LS. These include MMRPredict, MMRpro, and PREMM5.13-16 These models use clinical data (personal and family history of cancer and tumor phenotypes) to calculate the probability of a germline mutation in one of the mismatch repair (MMR) genes associated with LS. The current threshold at which to refer a patient for genetic counseling and testing is a predicted probability of 5% or greater using any one of these models, though some have proposed lowering the threshold to 2.5%.16,17
Universal tumor testing
Because of the limitations of relying on clinical family history, such as with the Amsterdam criteria and the Bethesda guidelines,18,19 as of 2014 the NCCN recommended universal tumor screening for DNA MMR deficiency associated with LS. This approach, also known as “universal testing,” has been shown to be cost effective and more sensitive in identifying at-risk patients than clinical criteria alone.20,21 Specifically, the NCCN recommends that tumor specimens of all patients diagnosed with CRC undergo testing for microsatellite instability (MSI) or loss of MMR proteins (MLH1, MSH2, MSH6, PMS2) expression by immunohistochemistry (IHC).5 Loss of MMR proteins or MSI-high findings should prompt a referral to genetics for counseling and consideration of testing for germline mutations. Universal testing of CRC and endometrial cancers is considered the most reliable way to screen patients for LS.
Universal testing by MSI or IHC may be performed on premalignant or malignant lesions. However, it is important to recognize that DNA MMR deficiency testing may not be as reliable when applied to colorectal polyps. Using data from three cancer registries (Dana-Farber Cancer Institute, University of Michigan, MD Anderson Cancer Center), Yurgelun and colleagues investigated the yield of MSI and IHC in colorectal polyps removed from patients with known LS.22 Overall, high-level MSI was found in only 41% of Lynch-associated adenomas and loss of MMR protein expression was evident in only 50%. While adenomas 8 mm in size or greater were more likely to have MSI-high or loss of MMR protein expression compared with those less than 8 mm in size, MMR-deficiency phenotype was less reliable in smaller adenomas. Consequently, results of MSI and/or IHC should therefore be interpreted with caution and in the context of the specimen upon which they are performed.
Considerations for clinical genetic testing
Genetic testing for cancer susceptibility should include informed consent and counseling for patients regarding potential risks and benefits. Clinicians ordering genetic testing should have the expertise necessary to interpret test results, which may be positive (pathogenic or likely pathogenic germline variant identified), or negative (no variants identified), or may yield one or more variants of uncertain clinical significance. Individuals found to carry a pathogenic or likely pathogenic germline variant associated with cancer susceptibility should be referred for additional genetic counseling and may require additional expert consultation for management of extracolonic cancer risks. It is important that individuals diagnosed with a hereditary cancer syndrome be informed that this diagnosis has implications for family members, who may also be at risk for the condition and may benefit from genetic testing.
Practical considerations
Given the difficulty in obtaining a detailed family history while in clinic or in endoscopy, several studies have investigated strategies that may be integrated into practice to identify high-risk patients without substantial burden on providers or patients. Kastrinos and colleagues identified the following three high-yield questions as part of a CRC Risk Assessment Tool that can be used while performing a precolonoscopy assessment: 1) Do you have a first-degree relative with CRC or LS-related cancer diagnosed before age 50?; 2) Have you had CRC or polyps diagnosed prior to age 50?; and 3) Do you have three or more relatives with CRC? The authors found that these three questions alone identified 77% of high-risk individuals.23 In addition, implementation of family history screening instruments using standardized surveys or self-administered risk prediction models at the time of colonoscopy have been shown to improve ascertainment of high-risk patients.24,25 Such strategies may become increasingly easier to implement with integration into patients’ electronic medical records.
Conclusions
Hereditary CRC syndromes are becoming increasingly important to identify, especially in an era where we are seeing rising rates of early-onset CRC. Early identification of high-risk features (Table 2) can lead to timely diagnosis with the goal to implement preventive strategies for screening and/or surveillance, ideally prior to development of cancers.
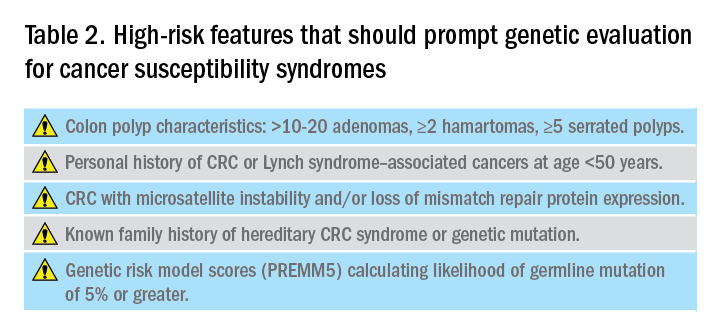
As gastroenterologists, we have several unique opportunities to identify these individuals and must maintain a high level of suspicion with careful attention when obtaining personal and family history details in clinic and in endoscopy.
Dr. Maratt is assistant professor, Indiana University, Richard L. Roudebush VA Medical Center, Indianapolis. Dr. Stoffel is assistant professor, University of Michigan; director of Cancer Genetic Clinic, Rogel Cancer Center, Ann Arbor. They have no conflicts of interest.
References
1. Pearlman R et al. JAMA Oncol. 2017;3(4):464-71.
2. Stoffel EM et al. Gastroenterology. 2018;154(4):897-905.
3. Kanth P et al. Am J Gastroenterol. 2017;112:1509-25.
4. Brennan B et al. Ther Adv Gastroenterol. 2017;10:361-71.
5. National Comprehensive Cancer Network. Available at: nccn.org.
6. Lynch HT et al. Nat Rev Cancer. 2015;15:181-94.
7. Syngal S et al. Am J Gastroenterol. 2015;110:223-62.
8. Mankaney G et al. Clin Gastroenterol Hepatol. 2020:(in press)
9. Yan HHN et al. Gut 2017;66:1645-56.
10. Ma H et al. Pathology. 2018;50:49-59.
11. Vasen H et al. Gastroenterology 1999;116:1453-6.
12. Umar A et al. J Natl Cancer Inst. 2004;96:261-8.
13. Kastrinos F et al. J Natl Cancer Inst. 2015;108(2):1-9.
14. Chen S et al. JAMA. 2006;296(12):1479-87.
15. Barnetson RA et al. N Engl J Med. 2006;354(26):2751-63.
16. Kastrinos F et al. J Clin Oncol. 2017;35:2165-72.
17. Kastrinos F et al. Fam Cancer. 2018;17:567-67.
18. Cohen SA et al. Annu Rev Genomics Hum Genet. 2019;20:293-307.
19. Matloff J et al. J Natl Compr Canc Netw. 2013;11:1380-5.
20. Ladabaum U et al. Ann Intern Med. 2011;155(2):69-79.
21. Hampel H et al. N Engl J Med. 2005;352(18):1851-60.
22. Yurgelun MB et al. Cancer Prev Res. 2012;5:574-82.
23. Kastrinos F et al. Am J Gastroenterol. 2009;104:1508-18.
24. Luba DG et al. Clin Gastroenterol Hepatol. 2018;16:49-58.
25. Guivatchian T et al. Gastrointest Endosc. 2017;86:684-91.
Introduction
Genetic predisposition to colorectal polyps and colorectal cancer (CRC) is more common than previously recognized. Approximately 5%-10% of all individuals diagnosed with CRC have a known genetic association. However, among those with early-onset CRC (diagnosed at age less than 50 years), recent studies show that up to 20% have an associated genetic mutation.1,2 In addition, the risk of CRC in patients with certain hereditary syndromes, such as familial adenomatous polyposis (FAP), approaches 80%-90% without timely management.3 This overall high risk of CRC and extracolonic malignancies in patients with a hereditary syndrome, along with the rising rates of early-onset CRC, underscores the importance of early diagnosis and management of a hereditary condition.
Despite increasing awareness of hereditary polyposis and nonpolyposis syndromes, referral rates for genetic counseling and testing remain low.4 As gastroenterologists we have several unique opportunities, in clinic and in endoscopy, to identify patients at risk for hereditary syndromes.
Risk stratification
Personal and family history
Reviewing personal medical history and family history in detail should be a routine part of our practice. This is often when initial signs of a potential hereditary syndrome can be detected. For example, if a patient reports a personal or family history of colorectal polyps or CRC, additional information that becomes important includes age at time of diagnosis, polyp burden (number and histologic subtype), presence of inflammatory bowel disease, and history of any extracolonic malignancies. Patients with multiple colorectal polyps (e.g. more than 10-20 adenomas or more than 2 hamartomas) and those with CRC diagnosed at a young age (younger than 50 years) should be considered candidates for genetic evaluation.5
Lynch syndrome (LS), an autosomal dominant condition caused by loss of DNA mismatch repair (MMR) genes, is the most common hereditary CRC syndrome, accounting for 2%-4% of all CRCs.3,6 Extracolonic LS-associated cancers to keep in mind while reviewing personal and family histories include those involving the gastrointestinal (GI) tract such as gastric, pancreatic, biliary tract, and small intestine cancers, and also non-GI tract cancers including endometrial, ovarian, urinary tract, and renal cancers along with brain tumors, and skin lesions including sebaceous adenomas, sebaceous carcinomas, and keratoacanthomas. Notably, after CRC, endometrial cancer is the second most common cancer among women with LS. Prior diagnosis of endometrial cancer should also prompt additional history-taking and evaluation for LS.
As the National Comprehensive Cancer Network (NCCN) highlights in its recent guidelines, several key findings in family history that should prompt referral to genetics for evaluation and testing for LS include: one or more first-degree relatives (FDR) with CRC or endometrial cancer diagnosed at less than 50 years of age, one or more FDR with CRC or endometrial cancer and another synchronous or metachronous LS-related cancer, two or more FDR or second-degree relatives (SDR) with LS-related cancer (including at least one diagnosed at age less than 50 years), and three or more FDR or SDR with LS-related cancers (regardless of age).5
Comprehensive assessment of family history should include all cancer diagnoses in first- and second-degree relatives, including age at diagnosis and cancer type, as well as ethnicity, as these inform the likelihood that the patient harbors a germline pathogenic variant associated with cancer predisposition.5 Given the difficulty of eliciting this level of detail, the family histories elicited in clinical settings are often limited or incomplete. Unknown family history should not be mistaken for unremarkable family history. Alternatively, if family history is unimpressive, this is not necessarily reassuring, as there can be variability in disease penetrance, including autosomal recessive syndromes that may skip generations, and de novo mutations do occur. In fact, among individuals with early-onset CRC diagnosed at age less than 50, only half of mutation carriers reported a family history of CRC in an FDR.2 Thus, individuals with concerning personal histories should undergo a genetic evaluation even if family history is not concerning.
Polyp phenotype
In addition to personal and family history, colon polyp history (including number, size, and histology) can provide important clues to identifying individuals with genetic predisposition to CRC. Table 1 highlights hereditary syndromes and polyp phenotypes associated with increased CRC risk. Based on consensus guidelines, individuals with a history of greater than 10-20 adenomas, 2 or more hamartomas, or 5 or more sessile serrated polyps should be referred for genetic testing.5,7 Serrated polyposis syndrome (SPS) is diagnosed based on at least one of the following criteria: 1) 5 or more serrated polyps, all at least 5 mm in size, proximal to the rectum including at least 2 that are 10 mm or larger in size, or 2) more than 20 serrated polyps distributed throughout the colon with at least 5 proximal to the rectum.8 Pathogenic germline variants in RNF43, a tumor suppressor gene, have been associated with SPS in rare families; however, in most cases genetic testing is uninformative and further genetic and environmental discovery studies are needed to determine the underlying cause.8,9

Risk prediction models
Models have been developed that integrate family history and phenotype data to help identify patients who may be at risk for LS. The Amsterdam criteria (more than 3 relatives with LS-associated cancers, more than 2 generations involving LS-associated cancers, and more than 1 cancer diagnosed before the age of 50; “3:2:1” criteria) were initially developed for research purposes to identify individuals who were likely to be carriers of mutations of LS based on CRC and later revised to include extracolonic malignancies (Amsterdam II).11 However, they have limited sensitivity for identifying high-risk patients. Similarly, the Bethesda guidelines have also been modified and revised to identify patients at risk for LS whose tumors should be tested with microsatellite instability (MSI), but also with limited sensitivity.12
Several risk prediction models have been developed that perform better than the Amsterdam criteria or Bethesda guidelines for determining which patients should be referred for genetic testing for LS. These include MMRPredict, MMRpro, and PREMM5.13-16 These models use clinical data (personal and family history of cancer and tumor phenotypes) to calculate the probability of a germline mutation in one of the mismatch repair (MMR) genes associated with LS. The current threshold at which to refer a patient for genetic counseling and testing is a predicted probability of 5% or greater using any one of these models, though some have proposed lowering the threshold to 2.5%.16,17
Universal tumor testing
Because of the limitations of relying on clinical family history, such as with the Amsterdam criteria and the Bethesda guidelines,18,19 as of 2014 the NCCN recommended universal tumor screening for DNA MMR deficiency associated with LS. This approach, also known as “universal testing,” has been shown to be cost effective and more sensitive in identifying at-risk patients than clinical criteria alone.20,21 Specifically, the NCCN recommends that tumor specimens of all patients diagnosed with CRC undergo testing for microsatellite instability (MSI) or loss of MMR proteins (MLH1, MSH2, MSH6, PMS2) expression by immunohistochemistry (IHC).5 Loss of MMR proteins or MSI-high findings should prompt a referral to genetics for counseling and consideration of testing for germline mutations. Universal testing of CRC and endometrial cancers is considered the most reliable way to screen patients for LS.
Universal testing by MSI or IHC may be performed on premalignant or malignant lesions. However, it is important to recognize that DNA MMR deficiency testing may not be as reliable when applied to colorectal polyps. Using data from three cancer registries (Dana-Farber Cancer Institute, University of Michigan, MD Anderson Cancer Center), Yurgelun and colleagues investigated the yield of MSI and IHC in colorectal polyps removed from patients with known LS.22 Overall, high-level MSI was found in only 41% of Lynch-associated adenomas and loss of MMR protein expression was evident in only 50%. While adenomas 8 mm in size or greater were more likely to have MSI-high or loss of MMR protein expression compared with those less than 8 mm in size, MMR-deficiency phenotype was less reliable in smaller adenomas. Consequently, results of MSI and/or IHC should therefore be interpreted with caution and in the context of the specimen upon which they are performed.
Considerations for clinical genetic testing
Genetic testing for cancer susceptibility should include informed consent and counseling for patients regarding potential risks and benefits. Clinicians ordering genetic testing should have the expertise necessary to interpret test results, which may be positive (pathogenic or likely pathogenic germline variant identified), or negative (no variants identified), or may yield one or more variants of uncertain clinical significance. Individuals found to carry a pathogenic or likely pathogenic germline variant associated with cancer susceptibility should be referred for additional genetic counseling and may require additional expert consultation for management of extracolonic cancer risks. It is important that individuals diagnosed with a hereditary cancer syndrome be informed that this diagnosis has implications for family members, who may also be at risk for the condition and may benefit from genetic testing.
Practical considerations
Given the difficulty in obtaining a detailed family history while in clinic or in endoscopy, several studies have investigated strategies that may be integrated into practice to identify high-risk patients without substantial burden on providers or patients. Kastrinos and colleagues identified the following three high-yield questions as part of a CRC Risk Assessment Tool that can be used while performing a precolonoscopy assessment: 1) Do you have a first-degree relative with CRC or LS-related cancer diagnosed before age 50?; 2) Have you had CRC or polyps diagnosed prior to age 50?; and 3) Do you have three or more relatives with CRC? The authors found that these three questions alone identified 77% of high-risk individuals.23 In addition, implementation of family history screening instruments using standardized surveys or self-administered risk prediction models at the time of colonoscopy have been shown to improve ascertainment of high-risk patients.24,25 Such strategies may become increasingly easier to implement with integration into patients’ electronic medical records.
Conclusions
Hereditary CRC syndromes are becoming increasingly important to identify, especially in an era where we are seeing rising rates of early-onset CRC. Early identification of high-risk features (Table 2) can lead to timely diagnosis with the goal to implement preventive strategies for screening and/or surveillance, ideally prior to development of cancers.
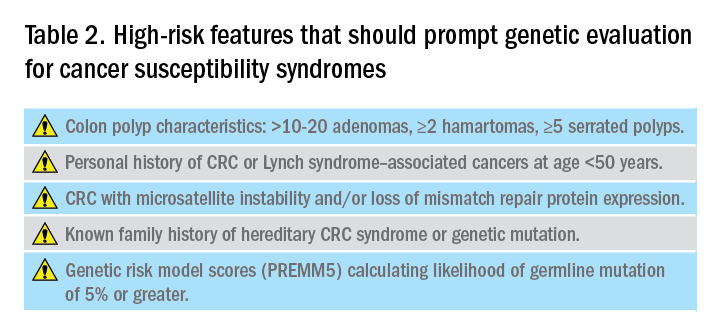
As gastroenterologists, we have several unique opportunities to identify these individuals and must maintain a high level of suspicion with careful attention when obtaining personal and family history details in clinic and in endoscopy.
Dr. Maratt is assistant professor, Indiana University, Richard L. Roudebush VA Medical Center, Indianapolis. Dr. Stoffel is assistant professor, University of Michigan; director of Cancer Genetic Clinic, Rogel Cancer Center, Ann Arbor. They have no conflicts of interest.
References
1. Pearlman R et al. JAMA Oncol. 2017;3(4):464-71.
2. Stoffel EM et al. Gastroenterology. 2018;154(4):897-905.
3. Kanth P et al. Am J Gastroenterol. 2017;112:1509-25.
4. Brennan B et al. Ther Adv Gastroenterol. 2017;10:361-71.
5. National Comprehensive Cancer Network. Available at: nccn.org.
6. Lynch HT et al. Nat Rev Cancer. 2015;15:181-94.
7. Syngal S et al. Am J Gastroenterol. 2015;110:223-62.
8. Mankaney G et al. Clin Gastroenterol Hepatol. 2020:(in press)
9. Yan HHN et al. Gut 2017;66:1645-56.
10. Ma H et al. Pathology. 2018;50:49-59.
11. Vasen H et al. Gastroenterology 1999;116:1453-6.
12. Umar A et al. J Natl Cancer Inst. 2004;96:261-8.
13. Kastrinos F et al. J Natl Cancer Inst. 2015;108(2):1-9.
14. Chen S et al. JAMA. 2006;296(12):1479-87.
15. Barnetson RA et al. N Engl J Med. 2006;354(26):2751-63.
16. Kastrinos F et al. J Clin Oncol. 2017;35:2165-72.
17. Kastrinos F et al. Fam Cancer. 2018;17:567-67.
18. Cohen SA et al. Annu Rev Genomics Hum Genet. 2019;20:293-307.
19. Matloff J et al. J Natl Compr Canc Netw. 2013;11:1380-5.
20. Ladabaum U et al. Ann Intern Med. 2011;155(2):69-79.
21. Hampel H et al. N Engl J Med. 2005;352(18):1851-60.
22. Yurgelun MB et al. Cancer Prev Res. 2012;5:574-82.
23. Kastrinos F et al. Am J Gastroenterol. 2009;104:1508-18.
24. Luba DG et al. Clin Gastroenterol Hepatol. 2018;16:49-58.
25. Guivatchian T et al. Gastrointest Endosc. 2017;86:684-91.
Introduction
Genetic predisposition to colorectal polyps and colorectal cancer (CRC) is more common than previously recognized. Approximately 5%-10% of all individuals diagnosed with CRC have a known genetic association. However, among those with early-onset CRC (diagnosed at age less than 50 years), recent studies show that up to 20% have an associated genetic mutation.1,2 In addition, the risk of CRC in patients with certain hereditary syndromes, such as familial adenomatous polyposis (FAP), approaches 80%-90% without timely management.3 This overall high risk of CRC and extracolonic malignancies in patients with a hereditary syndrome, along with the rising rates of early-onset CRC, underscores the importance of early diagnosis and management of a hereditary condition.
Despite increasing awareness of hereditary polyposis and nonpolyposis syndromes, referral rates for genetic counseling and testing remain low.4 As gastroenterologists we have several unique opportunities, in clinic and in endoscopy, to identify patients at risk for hereditary syndromes.
Risk stratification
Personal and family history
Reviewing personal medical history and family history in detail should be a routine part of our practice. This is often when initial signs of a potential hereditary syndrome can be detected. For example, if a patient reports a personal or family history of colorectal polyps or CRC, additional information that becomes important includes age at time of diagnosis, polyp burden (number and histologic subtype), presence of inflammatory bowel disease, and history of any extracolonic malignancies. Patients with multiple colorectal polyps (e.g. more than 10-20 adenomas or more than 2 hamartomas) and those with CRC diagnosed at a young age (younger than 50 years) should be considered candidates for genetic evaluation.5
Lynch syndrome (LS), an autosomal dominant condition caused by loss of DNA mismatch repair (MMR) genes, is the most common hereditary CRC syndrome, accounting for 2%-4% of all CRCs.3,6 Extracolonic LS-associated cancers to keep in mind while reviewing personal and family histories include those involving the gastrointestinal (GI) tract such as gastric, pancreatic, biliary tract, and small intestine cancers, and also non-GI tract cancers including endometrial, ovarian, urinary tract, and renal cancers along with brain tumors, and skin lesions including sebaceous adenomas, sebaceous carcinomas, and keratoacanthomas. Notably, after CRC, endometrial cancer is the second most common cancer among women with LS. Prior diagnosis of endometrial cancer should also prompt additional history-taking and evaluation for LS.
As the National Comprehensive Cancer Network (NCCN) highlights in its recent guidelines, several key findings in family history that should prompt referral to genetics for evaluation and testing for LS include: one or more first-degree relatives (FDR) with CRC or endometrial cancer diagnosed at less than 50 years of age, one or more FDR with CRC or endometrial cancer and another synchronous or metachronous LS-related cancer, two or more FDR or second-degree relatives (SDR) with LS-related cancer (including at least one diagnosed at age less than 50 years), and three or more FDR or SDR with LS-related cancers (regardless of age).5
Comprehensive assessment of family history should include all cancer diagnoses in first- and second-degree relatives, including age at diagnosis and cancer type, as well as ethnicity, as these inform the likelihood that the patient harbors a germline pathogenic variant associated with cancer predisposition.5 Given the difficulty of eliciting this level of detail, the family histories elicited in clinical settings are often limited or incomplete. Unknown family history should not be mistaken for unremarkable family history. Alternatively, if family history is unimpressive, this is not necessarily reassuring, as there can be variability in disease penetrance, including autosomal recessive syndromes that may skip generations, and de novo mutations do occur. In fact, among individuals with early-onset CRC diagnosed at age less than 50, only half of mutation carriers reported a family history of CRC in an FDR.2 Thus, individuals with concerning personal histories should undergo a genetic evaluation even if family history is not concerning.
Polyp phenotype
In addition to personal and family history, colon polyp history (including number, size, and histology) can provide important clues to identifying individuals with genetic predisposition to CRC. Table 1 highlights hereditary syndromes and polyp phenotypes associated with increased CRC risk. Based on consensus guidelines, individuals with a history of greater than 10-20 adenomas, 2 or more hamartomas, or 5 or more sessile serrated polyps should be referred for genetic testing.5,7 Serrated polyposis syndrome (SPS) is diagnosed based on at least one of the following criteria: 1) 5 or more serrated polyps, all at least 5 mm in size, proximal to the rectum including at least 2 that are 10 mm or larger in size, or 2) more than 20 serrated polyps distributed throughout the colon with at least 5 proximal to the rectum.8 Pathogenic germline variants in RNF43, a tumor suppressor gene, have been associated with SPS in rare families; however, in most cases genetic testing is uninformative and further genetic and environmental discovery studies are needed to determine the underlying cause.8,9

Risk prediction models
Models have been developed that integrate family history and phenotype data to help identify patients who may be at risk for LS. The Amsterdam criteria (more than 3 relatives with LS-associated cancers, more than 2 generations involving LS-associated cancers, and more than 1 cancer diagnosed before the age of 50; “3:2:1” criteria) were initially developed for research purposes to identify individuals who were likely to be carriers of mutations of LS based on CRC and later revised to include extracolonic malignancies (Amsterdam II).11 However, they have limited sensitivity for identifying high-risk patients. Similarly, the Bethesda guidelines have also been modified and revised to identify patients at risk for LS whose tumors should be tested with microsatellite instability (MSI), but also with limited sensitivity.12
Several risk prediction models have been developed that perform better than the Amsterdam criteria or Bethesda guidelines for determining which patients should be referred for genetic testing for LS. These include MMRPredict, MMRpro, and PREMM5.13-16 These models use clinical data (personal and family history of cancer and tumor phenotypes) to calculate the probability of a germline mutation in one of the mismatch repair (MMR) genes associated with LS. The current threshold at which to refer a patient for genetic counseling and testing is a predicted probability of 5% or greater using any one of these models, though some have proposed lowering the threshold to 2.5%.16,17
Universal tumor testing
Because of the limitations of relying on clinical family history, such as with the Amsterdam criteria and the Bethesda guidelines,18,19 as of 2014 the NCCN recommended universal tumor screening for DNA MMR deficiency associated with LS. This approach, also known as “universal testing,” has been shown to be cost effective and more sensitive in identifying at-risk patients than clinical criteria alone.20,21 Specifically, the NCCN recommends that tumor specimens of all patients diagnosed with CRC undergo testing for microsatellite instability (MSI) or loss of MMR proteins (MLH1, MSH2, MSH6, PMS2) expression by immunohistochemistry (IHC).5 Loss of MMR proteins or MSI-high findings should prompt a referral to genetics for counseling and consideration of testing for germline mutations. Universal testing of CRC and endometrial cancers is considered the most reliable way to screen patients for LS.
Universal testing by MSI or IHC may be performed on premalignant or malignant lesions. However, it is important to recognize that DNA MMR deficiency testing may not be as reliable when applied to colorectal polyps. Using data from three cancer registries (Dana-Farber Cancer Institute, University of Michigan, MD Anderson Cancer Center), Yurgelun and colleagues investigated the yield of MSI and IHC in colorectal polyps removed from patients with known LS.22 Overall, high-level MSI was found in only 41% of Lynch-associated adenomas and loss of MMR protein expression was evident in only 50%. While adenomas 8 mm in size or greater were more likely to have MSI-high or loss of MMR protein expression compared with those less than 8 mm in size, MMR-deficiency phenotype was less reliable in smaller adenomas. Consequently, results of MSI and/or IHC should therefore be interpreted with caution and in the context of the specimen upon which they are performed.
Considerations for clinical genetic testing
Genetic testing for cancer susceptibility should include informed consent and counseling for patients regarding potential risks and benefits. Clinicians ordering genetic testing should have the expertise necessary to interpret test results, which may be positive (pathogenic or likely pathogenic germline variant identified), or negative (no variants identified), or may yield one or more variants of uncertain clinical significance. Individuals found to carry a pathogenic or likely pathogenic germline variant associated with cancer susceptibility should be referred for additional genetic counseling and may require additional expert consultation for management of extracolonic cancer risks. It is important that individuals diagnosed with a hereditary cancer syndrome be informed that this diagnosis has implications for family members, who may also be at risk for the condition and may benefit from genetic testing.
Practical considerations
Given the difficulty in obtaining a detailed family history while in clinic or in endoscopy, several studies have investigated strategies that may be integrated into practice to identify high-risk patients without substantial burden on providers or patients. Kastrinos and colleagues identified the following three high-yield questions as part of a CRC Risk Assessment Tool that can be used while performing a precolonoscopy assessment: 1) Do you have a first-degree relative with CRC or LS-related cancer diagnosed before age 50?; 2) Have you had CRC or polyps diagnosed prior to age 50?; and 3) Do you have three or more relatives with CRC? The authors found that these three questions alone identified 77% of high-risk individuals.23 In addition, implementation of family history screening instruments using standardized surveys or self-administered risk prediction models at the time of colonoscopy have been shown to improve ascertainment of high-risk patients.24,25 Such strategies may become increasingly easier to implement with integration into patients’ electronic medical records.
Conclusions
Hereditary CRC syndromes are becoming increasingly important to identify, especially in an era where we are seeing rising rates of early-onset CRC. Early identification of high-risk features (Table 2) can lead to timely diagnosis with the goal to implement preventive strategies for screening and/or surveillance, ideally prior to development of cancers.
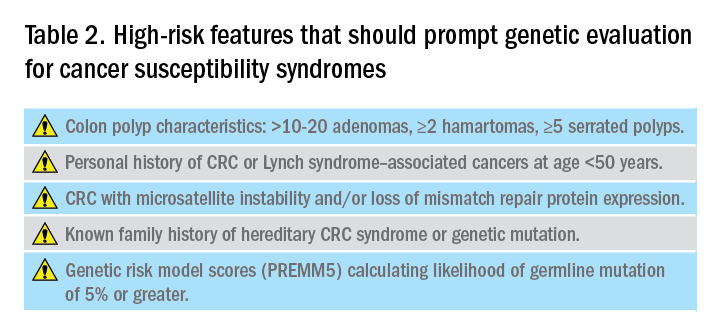
As gastroenterologists, we have several unique opportunities to identify these individuals and must maintain a high level of suspicion with careful attention when obtaining personal and family history details in clinic and in endoscopy.
Dr. Maratt is assistant professor, Indiana University, Richard L. Roudebush VA Medical Center, Indianapolis. Dr. Stoffel is assistant professor, University of Michigan; director of Cancer Genetic Clinic, Rogel Cancer Center, Ann Arbor. They have no conflicts of interest.
References
1. Pearlman R et al. JAMA Oncol. 2017;3(4):464-71.
2. Stoffel EM et al. Gastroenterology. 2018;154(4):897-905.
3. Kanth P et al. Am J Gastroenterol. 2017;112:1509-25.
4. Brennan B et al. Ther Adv Gastroenterol. 2017;10:361-71.
5. National Comprehensive Cancer Network. Available at: nccn.org.
6. Lynch HT et al. Nat Rev Cancer. 2015;15:181-94.
7. Syngal S et al. Am J Gastroenterol. 2015;110:223-62.
8. Mankaney G et al. Clin Gastroenterol Hepatol. 2020:(in press)
9. Yan HHN et al. Gut 2017;66:1645-56.
10. Ma H et al. Pathology. 2018;50:49-59.
11. Vasen H et al. Gastroenterology 1999;116:1453-6.
12. Umar A et al. J Natl Cancer Inst. 2004;96:261-8.
13. Kastrinos F et al. J Natl Cancer Inst. 2015;108(2):1-9.
14. Chen S et al. JAMA. 2006;296(12):1479-87.
15. Barnetson RA et al. N Engl J Med. 2006;354(26):2751-63.
16. Kastrinos F et al. J Clin Oncol. 2017;35:2165-72.
17. Kastrinos F et al. Fam Cancer. 2018;17:567-67.
18. Cohen SA et al. Annu Rev Genomics Hum Genet. 2019;20:293-307.
19. Matloff J et al. J Natl Compr Canc Netw. 2013;11:1380-5.
20. Ladabaum U et al. Ann Intern Med. 2011;155(2):69-79.
21. Hampel H et al. N Engl J Med. 2005;352(18):1851-60.
22. Yurgelun MB et al. Cancer Prev Res. 2012;5:574-82.
23. Kastrinos F et al. Am J Gastroenterol. 2009;104:1508-18.
24. Luba DG et al. Clin Gastroenterol Hepatol. 2018;16:49-58.
25. Guivatchian T et al. Gastrointest Endosc. 2017;86:684-91.
Hope springs eternal
As practicing clinicians, we all want to do what is best for patients. We hope our treatments will improve actual health outcomes (and not intermediate process metrics), so we make decisions based on “evidence” that lies on a continuum from “I hope” on one end to “I’m sure” on the other. This month, our three lead articles represent differing points along that continuum.
First, we consider H. pylori and gastric cancer. We know H. pylori eradication reduces ulcer risk and that H. pylori is a risk for gastric cancer. We did not know whether eradication reduces cancer risk. In a large retrospective study from the VA, Kumar et al demonstrated that eradication (not just treatment) substantially reduced subsequent gastric cancers. These data are not definitive, but they nudge us towards the “I’m sure” end of the continuum.
A second group of studies (both retrospective and prospective) suggests that successful weight loss after bariatric surgery was associated with a substantial reduction of risk for 13 cancer types related to obesity. Moderate evidence but again nudging us away from “I hope.”
A third article highlights the recent Clinical Practice Update on Barrett’s esophagus published by the AGA Clinical Practice Update Committee in Gastroenterology’s February 2020 issue. This practice update helps us understand the impact we will make on cancer reduction with surveillance and treatment of Barrett’s. Despite this publication, Barrett’s management remains closer to “hope” than “sure.”
The difficulty we face, as clinician or patient, is what to do when outcomes are really serious but evidence remains close to the “I hope” end. Take a reasonably healthy 68-year-old man with asymptomatic coronary disease, but a very high (and increasing) coronary artery calcium score, despite maximum statins and appropriate lifestyle practices. Should he initiate a PCSK9 inhibitor ($14,000 per year) absent evidence that it would alter cardiac risk? Recently, a retrospective study nudged us along the continuum (Peng et al. JACC Cardiovascular Imaging. 2020 Jan;13[1 Pt 1]:83-93). A serious outcome, suggestive but not definitive evidence, and no time for an RCT. Will such aggressive therapy help? I sure hope so.
John I. Allen, MD, MBA, AGAF
Editor in Chief
As practicing clinicians, we all want to do what is best for patients. We hope our treatments will improve actual health outcomes (and not intermediate process metrics), so we make decisions based on “evidence” that lies on a continuum from “I hope” on one end to “I’m sure” on the other. This month, our three lead articles represent differing points along that continuum.
First, we consider H. pylori and gastric cancer. We know H. pylori eradication reduces ulcer risk and that H. pylori is a risk for gastric cancer. We did not know whether eradication reduces cancer risk. In a large retrospective study from the VA, Kumar et al demonstrated that eradication (not just treatment) substantially reduced subsequent gastric cancers. These data are not definitive, but they nudge us towards the “I’m sure” end of the continuum.
A second group of studies (both retrospective and prospective) suggests that successful weight loss after bariatric surgery was associated with a substantial reduction of risk for 13 cancer types related to obesity. Moderate evidence but again nudging us away from “I hope.”
A third article highlights the recent Clinical Practice Update on Barrett’s esophagus published by the AGA Clinical Practice Update Committee in Gastroenterology’s February 2020 issue. This practice update helps us understand the impact we will make on cancer reduction with surveillance and treatment of Barrett’s. Despite this publication, Barrett’s management remains closer to “hope” than “sure.”
The difficulty we face, as clinician or patient, is what to do when outcomes are really serious but evidence remains close to the “I hope” end. Take a reasonably healthy 68-year-old man with asymptomatic coronary disease, but a very high (and increasing) coronary artery calcium score, despite maximum statins and appropriate lifestyle practices. Should he initiate a PCSK9 inhibitor ($14,000 per year) absent evidence that it would alter cardiac risk? Recently, a retrospective study nudged us along the continuum (Peng et al. JACC Cardiovascular Imaging. 2020 Jan;13[1 Pt 1]:83-93). A serious outcome, suggestive but not definitive evidence, and no time for an RCT. Will such aggressive therapy help? I sure hope so.
John I. Allen, MD, MBA, AGAF
Editor in Chief
As practicing clinicians, we all want to do what is best for patients. We hope our treatments will improve actual health outcomes (and not intermediate process metrics), so we make decisions based on “evidence” that lies on a continuum from “I hope” on one end to “I’m sure” on the other. This month, our three lead articles represent differing points along that continuum.
First, we consider H. pylori and gastric cancer. We know H. pylori eradication reduces ulcer risk and that H. pylori is a risk for gastric cancer. We did not know whether eradication reduces cancer risk. In a large retrospective study from the VA, Kumar et al demonstrated that eradication (not just treatment) substantially reduced subsequent gastric cancers. These data are not definitive, but they nudge us towards the “I’m sure” end of the continuum.
A second group of studies (both retrospective and prospective) suggests that successful weight loss after bariatric surgery was associated with a substantial reduction of risk for 13 cancer types related to obesity. Moderate evidence but again nudging us away from “I hope.”
A third article highlights the recent Clinical Practice Update on Barrett’s esophagus published by the AGA Clinical Practice Update Committee in Gastroenterology’s February 2020 issue. This practice update helps us understand the impact we will make on cancer reduction with surveillance and treatment of Barrett’s. Despite this publication, Barrett’s management remains closer to “hope” than “sure.”
The difficulty we face, as clinician or patient, is what to do when outcomes are really serious but evidence remains close to the “I hope” end. Take a reasonably healthy 68-year-old man with asymptomatic coronary disease, but a very high (and increasing) coronary artery calcium score, despite maximum statins and appropriate lifestyle practices. Should he initiate a PCSK9 inhibitor ($14,000 per year) absent evidence that it would alter cardiac risk? Recently, a retrospective study nudged us along the continuum (Peng et al. JACC Cardiovascular Imaging. 2020 Jan;13[1 Pt 1]:83-93). A serious outcome, suggestive but not definitive evidence, and no time for an RCT. Will such aggressive therapy help? I sure hope so.
John I. Allen, MD, MBA, AGAF
Editor in Chief
Dependent trait in chronic migraine may predict nonresponse to onabotulinumtoxin A
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
according to research published in the January issue of Headache. The research may be the first to show that personality traits predict response to onabotulinumtoxin A in this population.
“These findings point out that conducting an evaluation of personality traits in patients with chronic migraine might be helpful in the prediction of the course and election of the treatment, as well as identifying patients who might benefit from a multidisciplinary approach,” wrote Alicia Gonzalez-Martinez, MD, of the Hospital Universitario de La Princesa and Instituto de Investigación Sanitaria de La Princesa in Madrid and colleagues. “Categorical questionnaires such as the Salamanca screening test seem to be useful for this purpose.”
Researchers used ICD-10 personality criteria
Personality patterns in patients with migraine and other primary headaches have been the subject of decades of research. Munoz et al. found that certain personality traits are associated with migraine and chronic migraine, and this association may influence clinical management and treatment. The effect of personality traits on response to treatment, however, had not been studied previously.
Dr. Gonzalez-Martinez and colleagues hypothesized that cluster C traits (e.g., obsessive-compulsive, dependent, and anxious), as defined by ICD-10, are associated with nonresponse to onabotulinumtoxin A. To test this hypothesis, they conducted a case-control observational study in a cohort of patients with chronic migraine. Eligible patients presented to one of two headache units of a tertiary hospital between January and May 2018. The investigators obtained a complete headache history and demographic information from each patient. Patients had at least two treatment cycles of onabotulinumtoxin A. Dr. Gonzalez-Martinez and colleagues defined treatment response as a reduction in the number of monthly migraine days of at least 50% after at least two treatment cycles.
The investigators assessed participants’ personality traits by administering the Salamanca test, a brief categorical inventory that examines 11 personality traits using 22 questions. Patients completed the test at the beginning of the study period and before they were classified as responders or nonresponders.
Medication overuse was a potential confounder
The study population included 112 patients with chronic migraine. One hundred patients (89%) were women. Participants’ mean age at initiation of onabotulinumtoxin A treatment was 43 years. The population’s mean duration of chronic migraine was 29 months. Eighty-three patients (74.1%) had medication overuse, and 96 (85.7%) responded to onabotulinumtoxin A.
Cluster A traits in the population included paranoid (prevalence, 10.7%), schizoid (38.4%), and schizotypal (7.1%). Cluster B traits included histrionic (50%), antisocial (1.8%), narcissistic (9.8%), emotional instability subtype impulsive (27.7%), and emotional instability subtype limit (EISL, 24.1%). Cluster C traits were anxious (58.9%) anancastic (i.e., obsessive-compulsive, 54.5%), and dependent (32.1%).
The investigators found no differences in demographics between responders and nonresponders. In a univariate analysis, dependent traits (e.g., passivity and emotional overdependence on others) and EISL traits (e.g., impulsivity and disturbed self-image) were significantly more common among nonresponders. In a multivariate analysis, dependent traits remained significantly associated with nonresponse to onabotulinumtoxin A.
Medication overuse was a potential confounder in the study, according to Dr. Gonzalez-Martinez and colleagues. One of the study’s limitations was its absence of a healthy control group. Another was the fact that the psychometrics of the Salamanca screening test have not been published in a peer-reviewed journal and may need further examination.
Dependent personality “may also be part of the proposed chronic pain sufferer personality,” wrote the investigators. “Early detection of personality traits could improve management and outcome of chronic migraine patients. Additionally, the possibility to predict the effectiveness of onabotulinumtoxin A therapy may reduce costs and latency time of effect in patients with improbable effectiveness.”
The study had no outside funding, and the authors reported no conflicts of interest.
SOURCE: Gonzalez-Martinez A et al. Headache. 2020;60(1):153-61.
FROM HEADACHE
HHS declares coronavirus emergency, orders quarantine
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
The federal government declared a formal public health emergency on Jan. 31 to aid in the response to the 2019 Novel Coronavirus (2019-nCoV). The declaration, issued by Health and Human Services Secretary Alex. M. Azar II gives state, tribal, and local health departments additional flexibility to request assistance from the federal government in responding to the coronavirus.
"While this virus poses a serious public health threat, the risk to the American public remains low at this time, and we are working to keep this risk low."*
2019-nCoV—the first such action taken by the Centers for Disease Control and Prevention in more than 50 years.
“This decision is based on the current scientific facts,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases, said during a press briefing Jan. 31. “While we understand the action seems drastic, our goal today, tomorrow, and always continues to be the safety of the American public. We would rather be remembered for over-reacting than under-reacting.”
These actions come on the heels of the World Health Organization’s Jan. 30 declaration of 2019-nCoV as a public health emergency of international concern, and from a recent spike in cases reported by Chinese health officials. “Every day this week China has reported additional cases,” Dr. Messonnier said. “Today’s numbers are a 26% increase since yesterday. Over the course of the last week, there have been nearly 7,000 new cases reported. This tells us the virus is continuing to spread rapidly in China. The reported deaths have continued to rise as well. In addition, locations outside China have continued to report cases. There have been an increasing number of reports of person-to-person spread, and now, most recently, a report in the New England Journal of Medicine of asymptomatic spread.”
The quarantine of passengers will last 14 days from when the plane left Wuhan, China. Martin Cetron, MD, who directs the CDC’s Division of Global Migration and Quarantine, said that the quarantine order “offers the greatest level of protection for the American public in preventing introduction and spread. That is our primary concern. Prior epidemics suggest that when people are properly informed, they’re usually very compliant with this request to restrict their movement. This allows someone who would become symptomatic to be rapidly identified. Offering early, rapid diagnosis of their illness could alleviate a lot of anxiety and uncertainty. In addition, this is a protective effect on family members. No individual wants to be the source of introducing or exposing a family member or a loved one to their virus. Additionally, this is part of their civic responsibility to protect their communities.”
* This story was updated on 01/31/2020.
Is anxiety about the coronavirus out of proportion?
A number of years ago, a patient I was treating mentioned that she was not eating tomatoes. There had been stories in the news about people contracting bacterial infections from tomatoes, but I paused for a moment, then asked her: “Have there been any contaminated tomatoes here in Maryland?” There had not been and I was still happily eating salsa, but my patient thought about this differently: If disease-causing tomatoes were to come to our state, someone would be the first person to become ill. She did not want to take any risks. My patient, however, was a heavy smoker and already grappling with health issues that were caused by smoking, so I found her choice of what she should worry about and how it influenced her behavior to be perplexing. I realize it’s not the same; nicotine is an addiction, while tomatoes remain a choice for most of us, and it’s common for people to worry about very unlikely events even when we are surrounded by very real and statistically more probable threats to our well-being.
Today’s news reports are filled with stories about 2019 Novel Coronavirus (2019-nCoV), an illness that started in Wuhan, China; as of Jan. 31, 2020, there were 9,776 confirmed cases and 213 deaths. There have been an additional 118 cases reported outside of mainland China, including 6 in the United States, and no one outside of China has died.
The response to the virus has been remarkable: Wuhan, a city of more than 11 million inhabitants, is on lockdown, as are 15 other cities in China; 46 million people have been affected, the largest quarantine in human history. Travel is restricted in parts of China, airports all over the world are screening those who fly in from Wuhan, foreign governments are bringing their citizens home from Wuhan, and even Starbucks has temporarily closed half its stores in China. The economics of containing this virus are astounding.
In the meantime, the Centers for Disease Control and Prevention reports that, as of the week of Jan. 25, there have been 19 million cases of the flu in the United States. Of those stricken, 180,000 people have been hospitalized and 10,000 have died, including 68 pediatric patients. No cities are on lockdown, public transportation runs as usual, airports don’t screen passengers for flu symptoms, and Starbucks continues to serve vanilla lattes to any willing customer. Anxiety about illness is not new; we’ve seen it with SARS, Ebola, measles, and even around Chipotle’s food poisoning cases – to name just a few recent scares. We have also seen a lot of media on vaping-related deaths, and as of early January 2020, vaping-related illnesses affected 2,602 people with 59 deaths. It has been a topic of discussion among legislators, with an emphasis on either outlawing the flavoring that might appeal to younger people or simply outlawing e-cigarettes. No one, however, is talking about outlawing regular cigarettes, despite the fact that many people have switched from cigarettes to vaping products as a way to quit smoking. So, while vaping has caused 59 deaths since 2018, cigarettes are responsible for 480,000 fatalities a year in the United States and smokers live, on average, 10 years less than nonsmokers.
So what fuels anxiety about the latest health scare, and why aren’t we more anxious about the more common causes of premature mortality? Certainly, the newness and the unknown are factors in the coronavirus scare. It’s not certain how this illness was introduced into the human population, although one theory is that it started with the consumption of bats who carry the virus. It’s spreading fast, and in some people, it has been lethal. The incubation period is not known, or whether it is contagious before symptoms appear. Coronavirus is getting a lot of public health attention and the World Health Organization just announced that the virus is a public health emergency of international concern. On the televised news on Jan. 29, 2020, coronavirus was the top story in the United States, even though an impeachment trial is in progress for our country’s president.
The public health response of locking down cities may help contain the outbreak and prevent a global epidemic, although millions of people had already left Wuhan, so the heavy-handed attempt to prevent spread of the virus may well be too late. In the case of the Ebola virus – a much more lethal disease that was also thought to be introduced by bats – public health measures certainly curtailed global spread, and the epidemic of 2014-2016 was limited to 28,600 cases and 11,325 deaths, nearly all of them in West Africa.
Most of the things that cause people to die are not new and are not topics the media chooses to sensationalize. Dissemination of news has changed over the decades, with so much more of it, instant reports on social media, and competition for viewers that leads journalists to pull at our emotions. And while we may, or may not, get flu shots and avoid those who have the flu, how and where we position both our anxiety and our resources does not always make sense. Certainly some people are predisposed to worry about both common and uncommon dangers, while others seem never to worry and engage in acts that many of us would consider dangerous. If we are looking for logic, it may be hard to find – there are those who would happily go bungee jumping but wouldn’t dream of leaving the house out without hand sanitizer.
The repercussions from this massive response to the Wuhan coronavirus are significant. For the millions of people on lockdown in China, each day gets emotionally harder; some may begin to have issues procuring food, and the financial losses for the economy will be significant. It’s not really possible to know yet if this response is warranted; we do know that infectious diseases can kill millions. The AIDS pandemic has taken the lives of 36 million people since 1981, and the influenza pandemic of 1918 resulted in an estimated 20 million to 50 million deaths after infecting 500 million people. Still, one might wonder if other, more mundane causes of morbidity and mortality – the ones that no longer garner our dread or make it to the front pages – might also be worthy of more hype and resources.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
A number of years ago, a patient I was treating mentioned that she was not eating tomatoes. There had been stories in the news about people contracting bacterial infections from tomatoes, but I paused for a moment, then asked her: “Have there been any contaminated tomatoes here in Maryland?” There had not been and I was still happily eating salsa, but my patient thought about this differently: If disease-causing tomatoes were to come to our state, someone would be the first person to become ill. She did not want to take any risks. My patient, however, was a heavy smoker and already grappling with health issues that were caused by smoking, so I found her choice of what she should worry about and how it influenced her behavior to be perplexing. I realize it’s not the same; nicotine is an addiction, while tomatoes remain a choice for most of us, and it’s common for people to worry about very unlikely events even when we are surrounded by very real and statistically more probable threats to our well-being.
Today’s news reports are filled with stories about 2019 Novel Coronavirus (2019-nCoV), an illness that started in Wuhan, China; as of Jan. 31, 2020, there were 9,776 confirmed cases and 213 deaths. There have been an additional 118 cases reported outside of mainland China, including 6 in the United States, and no one outside of China has died.
The response to the virus has been remarkable: Wuhan, a city of more than 11 million inhabitants, is on lockdown, as are 15 other cities in China; 46 million people have been affected, the largest quarantine in human history. Travel is restricted in parts of China, airports all over the world are screening those who fly in from Wuhan, foreign governments are bringing their citizens home from Wuhan, and even Starbucks has temporarily closed half its stores in China. The economics of containing this virus are astounding.
In the meantime, the Centers for Disease Control and Prevention reports that, as of the week of Jan. 25, there have been 19 million cases of the flu in the United States. Of those stricken, 180,000 people have been hospitalized and 10,000 have died, including 68 pediatric patients. No cities are on lockdown, public transportation runs as usual, airports don’t screen passengers for flu symptoms, and Starbucks continues to serve vanilla lattes to any willing customer. Anxiety about illness is not new; we’ve seen it with SARS, Ebola, measles, and even around Chipotle’s food poisoning cases – to name just a few recent scares. We have also seen a lot of media on vaping-related deaths, and as of early January 2020, vaping-related illnesses affected 2,602 people with 59 deaths. It has been a topic of discussion among legislators, with an emphasis on either outlawing the flavoring that might appeal to younger people or simply outlawing e-cigarettes. No one, however, is talking about outlawing regular cigarettes, despite the fact that many people have switched from cigarettes to vaping products as a way to quit smoking. So, while vaping has caused 59 deaths since 2018, cigarettes are responsible for 480,000 fatalities a year in the United States and smokers live, on average, 10 years less than nonsmokers.
So what fuels anxiety about the latest health scare, and why aren’t we more anxious about the more common causes of premature mortality? Certainly, the newness and the unknown are factors in the coronavirus scare. It’s not certain how this illness was introduced into the human population, although one theory is that it started with the consumption of bats who carry the virus. It’s spreading fast, and in some people, it has been lethal. The incubation period is not known, or whether it is contagious before symptoms appear. Coronavirus is getting a lot of public health attention and the World Health Organization just announced that the virus is a public health emergency of international concern. On the televised news on Jan. 29, 2020, coronavirus was the top story in the United States, even though an impeachment trial is in progress for our country’s president.
The public health response of locking down cities may help contain the outbreak and prevent a global epidemic, although millions of people had already left Wuhan, so the heavy-handed attempt to prevent spread of the virus may well be too late. In the case of the Ebola virus – a much more lethal disease that was also thought to be introduced by bats – public health measures certainly curtailed global spread, and the epidemic of 2014-2016 was limited to 28,600 cases and 11,325 deaths, nearly all of them in West Africa.
Most of the things that cause people to die are not new and are not topics the media chooses to sensationalize. Dissemination of news has changed over the decades, with so much more of it, instant reports on social media, and competition for viewers that leads journalists to pull at our emotions. And while we may, or may not, get flu shots and avoid those who have the flu, how and where we position both our anxiety and our resources does not always make sense. Certainly some people are predisposed to worry about both common and uncommon dangers, while others seem never to worry and engage in acts that many of us would consider dangerous. If we are looking for logic, it may be hard to find – there are those who would happily go bungee jumping but wouldn’t dream of leaving the house out without hand sanitizer.
The repercussions from this massive response to the Wuhan coronavirus are significant. For the millions of people on lockdown in China, each day gets emotionally harder; some may begin to have issues procuring food, and the financial losses for the economy will be significant. It’s not really possible to know yet if this response is warranted; we do know that infectious diseases can kill millions. The AIDS pandemic has taken the lives of 36 million people since 1981, and the influenza pandemic of 1918 resulted in an estimated 20 million to 50 million deaths after infecting 500 million people. Still, one might wonder if other, more mundane causes of morbidity and mortality – the ones that no longer garner our dread or make it to the front pages – might also be worthy of more hype and resources.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.
A number of years ago, a patient I was treating mentioned that she was not eating tomatoes. There had been stories in the news about people contracting bacterial infections from tomatoes, but I paused for a moment, then asked her: “Have there been any contaminated tomatoes here in Maryland?” There had not been and I was still happily eating salsa, but my patient thought about this differently: If disease-causing tomatoes were to come to our state, someone would be the first person to become ill. She did not want to take any risks. My patient, however, was a heavy smoker and already grappling with health issues that were caused by smoking, so I found her choice of what she should worry about and how it influenced her behavior to be perplexing. I realize it’s not the same; nicotine is an addiction, while tomatoes remain a choice for most of us, and it’s common for people to worry about very unlikely events even when we are surrounded by very real and statistically more probable threats to our well-being.
Today’s news reports are filled with stories about 2019 Novel Coronavirus (2019-nCoV), an illness that started in Wuhan, China; as of Jan. 31, 2020, there were 9,776 confirmed cases and 213 deaths. There have been an additional 118 cases reported outside of mainland China, including 6 in the United States, and no one outside of China has died.
The response to the virus has been remarkable: Wuhan, a city of more than 11 million inhabitants, is on lockdown, as are 15 other cities in China; 46 million people have been affected, the largest quarantine in human history. Travel is restricted in parts of China, airports all over the world are screening those who fly in from Wuhan, foreign governments are bringing their citizens home from Wuhan, and even Starbucks has temporarily closed half its stores in China. The economics of containing this virus are astounding.
In the meantime, the Centers for Disease Control and Prevention reports that, as of the week of Jan. 25, there have been 19 million cases of the flu in the United States. Of those stricken, 180,000 people have been hospitalized and 10,000 have died, including 68 pediatric patients. No cities are on lockdown, public transportation runs as usual, airports don’t screen passengers for flu symptoms, and Starbucks continues to serve vanilla lattes to any willing customer. Anxiety about illness is not new; we’ve seen it with SARS, Ebola, measles, and even around Chipotle’s food poisoning cases – to name just a few recent scares. We have also seen a lot of media on vaping-related deaths, and as of early January 2020, vaping-related illnesses affected 2,602 people with 59 deaths. It has been a topic of discussion among legislators, with an emphasis on either outlawing the flavoring that might appeal to younger people or simply outlawing e-cigarettes. No one, however, is talking about outlawing regular cigarettes, despite the fact that many people have switched from cigarettes to vaping products as a way to quit smoking. So, while vaping has caused 59 deaths since 2018, cigarettes are responsible for 480,000 fatalities a year in the United States and smokers live, on average, 10 years less than nonsmokers.
So what fuels anxiety about the latest health scare, and why aren’t we more anxious about the more common causes of premature mortality? Certainly, the newness and the unknown are factors in the coronavirus scare. It’s not certain how this illness was introduced into the human population, although one theory is that it started with the consumption of bats who carry the virus. It’s spreading fast, and in some people, it has been lethal. The incubation period is not known, or whether it is contagious before symptoms appear. Coronavirus is getting a lot of public health attention and the World Health Organization just announced that the virus is a public health emergency of international concern. On the televised news on Jan. 29, 2020, coronavirus was the top story in the United States, even though an impeachment trial is in progress for our country’s president.
The public health response of locking down cities may help contain the outbreak and prevent a global epidemic, although millions of people had already left Wuhan, so the heavy-handed attempt to prevent spread of the virus may well be too late. In the case of the Ebola virus – a much more lethal disease that was also thought to be introduced by bats – public health measures certainly curtailed global spread, and the epidemic of 2014-2016 was limited to 28,600 cases and 11,325 deaths, nearly all of them in West Africa.
Most of the things that cause people to die are not new and are not topics the media chooses to sensationalize. Dissemination of news has changed over the decades, with so much more of it, instant reports on social media, and competition for viewers that leads journalists to pull at our emotions. And while we may, or may not, get flu shots and avoid those who have the flu, how and where we position both our anxiety and our resources does not always make sense. Certainly some people are predisposed to worry about both common and uncommon dangers, while others seem never to worry and engage in acts that many of us would consider dangerous. If we are looking for logic, it may be hard to find – there are those who would happily go bungee jumping but wouldn’t dream of leaving the house out without hand sanitizer.
The repercussions from this massive response to the Wuhan coronavirus are significant. For the millions of people on lockdown in China, each day gets emotionally harder; some may begin to have issues procuring food, and the financial losses for the economy will be significant. It’s not really possible to know yet if this response is warranted; we do know that infectious diseases can kill millions. The AIDS pandemic has taken the lives of 36 million people since 1981, and the influenza pandemic of 1918 resulted in an estimated 20 million to 50 million deaths after infecting 500 million people. Still, one might wonder if other, more mundane causes of morbidity and mortality – the ones that no longer garner our dread or make it to the front pages – might also be worthy of more hype and resources.
Dr. Miller is coauthor with Annette Hanson, MD, of “Committed: The Battle Over Involuntary Psychiatric Care” (Baltimore: Johns Hopkins University, 2016). She has a private practice and is assistant professor of psychiatry and behavioral sciences at Johns Hopkins, both in Baltimore.